Asthenozoospermia, also known as asthenospermia, is an alteration that affects sperm motility. It is commonly known as slow moving sperm or lazy sperm.
In the situation where a man has a high percentage of spermatozoa that do not have adequate movement, it may be difficult to achieve pregnancy naturally. Therefore, an assisted reproductive technique may be necessary.
Provided below is an index with the 11 points we are going to expand on in this article.
- 1.
- 2.
- 2.1.
- 3.
- 3.1.
- 3.2.
- 4.
- 4.1.
- 5.
- 6.
- 6.1.
- 7.
- 8.
- 8.1.
- 8.2.
- 8.3.
- 8.4.
- 8.5.
- 8.6.
- 8.7.
- 9.
- 10.
- 11.
Definition of astenozoospermia
Astenozoospermia is a sperm quality defect caused by a decrease in the percentage of motile spermatazoa. Sometimes this alteration is accompanied by oligospermia (low concentration of spermatozoa in the ejaculated semen) . In this case, it is known as oligoasthenozoospermia.
A man is considered affected with asthenozoospermia when less than 40% of his spermatozoa are motile.
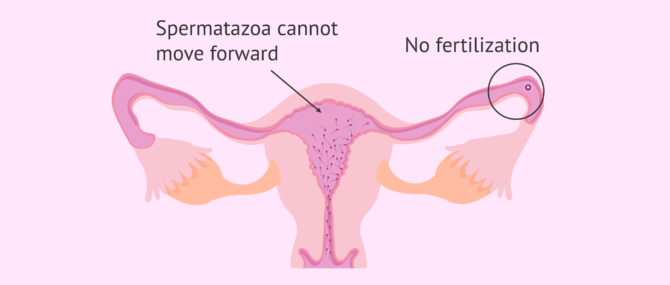
Asthenozoospermia is a cause of male infertility, since the sperm are not able to reach the egg and fertilize it due to their lack of mobility. Therefore, this situation hinders the possibility of getting pregnant.
Diagnosis
Asthenozoospermia does not cause clinical manifestations. The man can have sexual intercourse and ejaculate normally, unaware of the motility problem in his sperm. However, when trying to achieve pregnancy, complications occur.
The seminogram or spermiogram is the test used to analyze the male semen. One of the parameters that is assessed in the semen is the mobility and motility of the spermatozoa.
Analysis of sperm motility
During sperm analysis, a drop of semen is introduced into the sperm-counting chamber (Makler or Neubauer chamber) and observed under the microscope. Next, the movement of approximately 200 spermatozoids is studied.
When performing this study it is not only important to know whether or not the spermatozoa move, but is also important to analyze how they move. Therefore, in the analysis of sperm motility we determine:
- Progresssive motility
- the spermatozoa must be able to advance in distance, to allow them to cross the female reproductive tract and fertilize the ovum. There are times when the spermatozoa show movement, but without it being progressive..
- Speed
- sperm cells can move quickly or slowly.
According to criteria established by the WHO, a man does not suffer from asthenozoospermia, that is to say, their sperm has normal motility when it presents:
- Values equal to or above 40% of motile sperm (progressive and non-progressive).
- Values above 32% of sperm with progressive motility, that is to say, capable of moving forward.
If you want to learn more about sperm motility, you can continue reading here: What values are normal in sperm motility analysis?
Classification according to severity
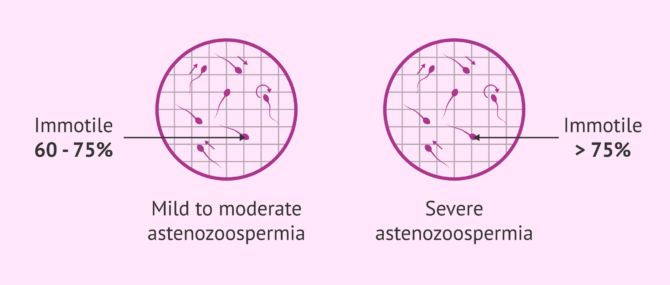
Depending on the exact percentage of immotile sperm found in the sperm sample analyzed, the degree of asthenozoospermia will be more or less severe.
Here we discuss the two levels of asthenozoospermia, according to their severity.
There are no exact criteria to differentiate between severe and mild asthenozoospermia. The fundamental difference is based on the speed and form of the movements, as well as on the quantity of immotile spermatozoa.
Mild to moderate
A semen sample is said to have mild grade asthenozoospermia when the percentage of non-motile or poorly motile sperm is between 60% and 75%.
It is essential to consider the type of movement, since if, at least, a small amount of spermatozoa move with straight, forward movements, an advance of sperm could be seen.
Severe or serious
Severe asthenospermia is diagnosed when there is a very high percentage of spermatozoa with low or no motility.
When the percentage of immotile spermatozoa is close to 75-80% or even higher, it is considered to be a case of severe asthenospermia.
Causes
The causes that can affect sperm motility and lead to asthenozoospermia are diverse and have not been precisely defined. It could be a result of environmental factors, infections, genetic or immunological alterations, etc.
However, it is known that sperm motility can be influenced by the following factors:
- Presence of antisperm antibodies.
- Excessive consumption of alcohol, smoking, marijuana and other drugs.
- Advanced age: a decrease in motility has been studied after 45 years of age.
- Fever.
- Exposure to toxic substances such as fertilizers, chemical solvents etc.
- Infections that affect the semen.
- Poor nutrition, an unbalanced or unhealthy diet. A balanced and healthy diet is fundamental for good sperm motility.
- Prolonged expsosure to heat.
- Testicular problems.
- Cancer treatments such as chemotherapy or radiotherapy.
- Vasectomy.
- Varicocele: the presence of dilated veins in the scrotum.
Similarly, the presence of other alterations in spermatozoa such as teratozoospermia can lead to asthenozoospermia. It should be remembered that the term teratozoospermia refers to alterations affecting the shape or morphology of the spermatozoa, which can also affect their movement.
Genetic causes
If a man is not seen to have any sperm in his semen, or the semen present with motility issues, it could also be due a genetic basis.
Kartagener syndrome, also known as primary ciliary dyskinesia or dyskinetic cilia syndrome, is a rare autosomal recessive disease characterized by defects in the structure and function of the cilia. This syndrome is associated with male infertility, as it affects sperm motility.
Treatment
To help improve sperm motility and even resolve certain cases of mild or mild asthenozoospermia, leading a healthy lifestyle and avoiding toxic habits (smoking, alcohol consumption, etc.) is recommended. These affect overall sperm quality, including sperm motility.
In addition, it may be advisable to take a vitamin supplement containing antioxidants (supervised by the specialist). The physician may recommend the intake of foods rich in vitamins or zinc, for example.
Severe or serious asthenozoospermia is difficult to improve with such natural treatments. Therefore, in these cases, it would be necessary to resort to assisted reproduction techniques in order to achieve pregnancy.
If you need to undergo IVF to become a mother, we recommend that you generate your Fertility Report now. In 3 simple steps, it will show you a list of clinics that fit your preferences and meet our strict quality criteria. Moreover, you will receive a report via email with useful tips to visit a fertility clinic for the first time.
If, however, the cause of the asthenozoospermia is known, a treatment aimed directed at curing that cause can be given. For example, if the cause is an infection, the specialist should prescribe the appropriate antibiotic treatment for the patient and the semen analysis should be repeated after 3 months.
Astenozoospermia and infertility
Asthenozoospermia is a fairly common cause of male infertility. Sperm must travel a long and arduous path from the time they are deposited in the vagina until they reach the egg in the Fallopian tubes.
Therefore, if the mobility of the sperm is affected, it is difficult for them to make the entire journey and fertilize the egg, resulting in infertility. The progressive movement and speed of the spermatozoa are very important aspects to achieve pregnancy in a natural way.
When the sperm do not move, or do so inadequately (without forward progression), natural fertilization becomes very complicated. It is in these cases when assisted reproductive techniques should be used.
Solutions for getting pregnant
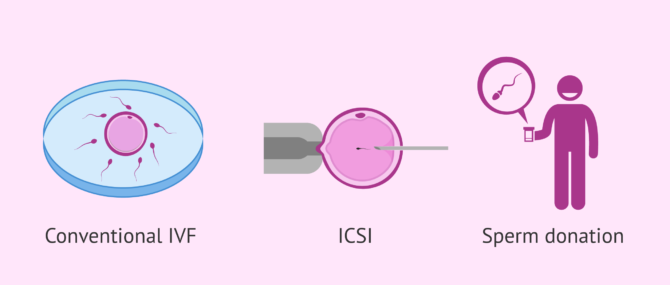
When a man is diagnosed with astenozooaspermia, and his partner does not fall pregnant, in vitro fertilization (IVF) is recommended, by conventional IVF or by ICSI (introcytoplasmic sperm injection.)
Artificial insemination with conjugal sperm (AIH) is not indicated in these cases. With this technique, the sperm must ascend on their own from the uterus to the fallopian tubes and, therefore, a good number of motile sperm is required.
In short, the potential assisted reproduction treatment options available are as follows:
- Conventional IVF
- In cases of mild asthenozoospermia this technique is possible. It is the simplest, version of IVF, placing a large number of sperm in contact with the egg to allow fertilization to occur.
- ICSI
- This is the best option in the most severe cases of asthenozoospermia. In contrast to the conventional version, it is the embryologist who injects the sperm into the egg, so motility is not required.
If these techniques prove to be unsuccessful, an alternative is to turn to donated sperm in order to have children. If this option is pursued, it becomes possible to perform artificial insemination with donor sperm (AID) or in vitro fertilization (IVF).
An interview with Laura Mifsud Elena
In an interview with embryologist Laura Mifsud, we heard that it is crucial to repeat the semen analysis before rendering a definitive diagnosis of asthenozoospermia to a patient.
Diagnosing asthenozoospermia or any other sperm diagnosis with a single sperm analysis is a mistake, since it might be due to a external or environmental factor, or a temporary circumstance of the patient.
For this reason, repeating the sperm test is essential to confirm the diagnosis. Moreover, the time period between semen analyses should be such that that any external factors influencing the results have disappeared.
FAQs from users
What are the possible treatments for asthenozoospermia?
Asthenozoospermia is a decrease in sperm motility. According to the World Health Organization (WHO), a progressive motility of more than 32% (31-34%) is considered normal, while total motility (progressive + non-progressive) is 40% (38-42%).
When in two seminograms performed on a patient with a period of 2-3 months between one and the other a lower motility is found, it is considered asthenozoospermia.
The first line of treatment should be aimed at improving habits and quality of life: not smoking, not drinking alcohol, not taking drugs, exercising, not being overweight, eating a balanced diet, etc.
As for the possible pharmacological treatment, it should always be indicated by a urologist. Androgens, human menopausal hCG/gonadotropin, bromocriptine, alpha-blockers, systemic corticosteroids and magnesium supplements have been shown not to be effective in the treatment of asthenozoospermia. In addition, follicle-stimulating hormone and anti-estrogens in combination with testosterone may be beneficial treatments in selected patients (always under strict medical supervision by a specialist).
The treatment of infertility caused by such asthenozoospermia is the use of assisted reproduction techniques that facilitate the arrival or entry of sperm into the oocyte (egg), such as artificial insemination or in vitro fertilization with or without ICSI.
Can a period of abstinence influence sperm motility?
The male factor has become one of the most relevant aspects of assisted reproduction recently. Different genetic diagnostic techniques have been used to analyze the role that the male plays in achieving a pregnancy.
The period of abstinence is an aspect that has varied over the years, thinking at first that the greater the abstinence, the better the result of both the seminal diagnosis and the embryonic evolution and term pregnancy. Some studies show that a period of frequent ejaculations after a period of abstinence can improve sperm quality.
The period of abstinence differs according to the assisted reproduction unit attended and the standardization of the processes. The recommendations of the World Health Organization is to have sexual abstinence of between 2-7 days. If the abstinence is less than two days, we will find spermatozoa that possibly have less DNA fragmentation, but the count of the number of spermatozoa is lower than in normal conditions. If we have a high abstinence period, it is likely that we will find reduced sperm motility.
In conclusion, it is important to have an optimal period of abstinence according to the recommendations of the assisted reproduction center in order to maximize the chances of success in each case.
Can I conceive naturally with asthenozoospermia, or do we need fertility treatment for my partner to become pregnant?
There are still chances of achieving a natural pregnancy with asthenozoospermia if it is a mild-to-moderate case. However, if sperm motility is severely affected, the only option to become parents would be using a fertility treatment like IVF with ICSI.
What are the symptoms of asthenozoospermia?
Unfortunately, there are no symptoms associated with asthenozoospermia. The only possible way for a patient to suspect that he has this sperm disorder is by doing a semen analysis.
The results of my sperm analysis indicate discrete astenozoospermia, what does this mean?
It means that a percentage greater than 60% of the spermatozoa in the semen sample analyzed are immotile or have motility problems. The qualifier discrete refers to the fact that it is not a very high percentage or well above the reference value.
What can we do in a case of ideopathic asthenozoospermia?
When there is a case of ideopathic asthenozoospermia, i.e. the cause is unknown, pentoxifylline can improve sperm motility and sperm count.
Pentoxifylline can improve sperm motility and can even cause immotile sperm to become motile.
In any case, this type of treatment must be prescribed by a medical specialist.
Is astenozoospermia hereditary?
In some cases, asthenozoospermia is due to a genetic cause, so it can be passed down from from parents to children. This is true for asthenozoospermia caused by Kartagener's syndrome or by microdeletions in the Y chromosome.
However, there are several factors that affect sperm motility such as infections, immunological alterations, varicocele, poor nutrition, etc.
Recommended reading
We have made several references to the semen analysis test in this post. It is the test that allows us to diagnose not only asthenozoospermia, but also other sperm disorders. To learn more about this diagnostic test visit the following link: What Is a Semen Analysis Report? – Purpose, Preparation & Cost.
Finally, if you are interested in, or need to undergo ICSI, the fertility treatment typically used to achieve pregnancy with asthenozoospermia, click here: What Is ICSI Technique? – Process, Success Rates & Cost.
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Aitken RJ, Buckingham DW, Brindle, J, Gomez E, Baker HWG, Irvine DS (1995): Analysis of sperm movement in relation to the oxidative stress created by leukocytes in washed sperm preparations and seminal plasma. Hum Reprod 10:2061–2070.
Blanco AM (1992): El laboratorio en el estudio del factor masculino en infertilidad. In: Guitelman A, Aszpiz SM (Eds). Exploracion Funcional Endocrina. Buenos Aires: Ed. Akadia, 1992.
Bruno Dahlberg (1990) Asthenozoospermia/Teratozoospermia and Infertility, Archives of Andrology, 25:1, 85-87.
Dahlberg B (1988): Sperm motility in fertile men and males in infertile units: In vitro test. Arch Androl 20:31-34.
Reproducción Asistida ORG. Video: Astenozoospermia (Asthenozoospermia), by Laura Mifsud Elena, BSc, MSc, Jul 8, 2015. [See original video in Spanish].
S. M. Curi, J. I. Ariagno, P. H. Chenlo, G. R. Mendeluk, M. N. Pugliese, L. M. Sardi Segovia, H. E. H. Repetto & A. M. Blanco (2003) Asthenozoospermia: analysis of a large population, Archives Of Andrology, 49:5, 343-349.
World Health Organization (1992): WHO Laboratory Manual for the Examination of Human Semen and Sperm–Cervical Mucus Interaction, ed 3. Cambridge,UK: Cambridge University Press.
FAQs from users: 'What are the possible treatments for asthenozoospermia?', 'Can a period of abstinence influence sperm motility?', 'Can I conceive naturally with asthenozoospermia, or do we need fertility treatment for my partner to become pregnant?', 'What are the symptoms of asthenozoospermia?', 'The results of my sperm analysis indicate discrete astenozoospermia, what does this mean?', 'Are there any foods that improve astenozoospermia?', 'What can we do in a case of ideopathic asthenozoospermia?' and 'Is astenozoospermia hereditary?'.
Authors and contributors


More information about Michelle Lorraine Embleton








Hi,
We are Married and TTC for 3 Years. Semen Analysis Results are as Follows:
1. Sperm Count: 54Mil/ml
2. Sperm Motility: 42%
3. Sperm Morphology: 5%
Would like to understand the Chances of Natural Conception and should i need to take any suitable medication to improve the parameters?
Dear Senthil,
Usually it is needed a more extended semen analysis to evaluate it properly. There are several important parameters that would be helpful, like volume, vitality and an analysis of the motility that allows to differentiate between the different types (progressive, non-progressive…).
Even so, the sperm count and the motility are normal and would allow a natural conception. In the case of morphology, it can be analysed with different methodologies that have different reference values. For example, if the morphology has been assessed by the WHO method the cut point is 4% of normal forms or more. In this case, the morphology of your semen analysis would be normal. If it has been assessed by the Kruger method the cut point is at 14%, which would mean that, in your case, that parameter is altered. In order to solve this doubt, you should check the semen analysis report and look for the morphology reference values.
Since the rest of parameters are normal, the morphology is the one that will indicate in your case if natural conception is possible. Since you have been 3 years trying to conceive if morphology is normal you should run other tests in order to determine the infertility causes. If it is altered it might be the cause of the infertility and it is advisable to contact a fertility specialist to extend the fertility study and be assessed about which treatment is the most suitable in your case.
Best wishes.
Hi,
I am 31 years old married male and we are attempting for baby from past 3 years with no success. My problem is with Sperm quality which is as follows;
Sperm Count – 20million per cc
Morphology – Normal -90%
Forward Movement – 60%
Non Linear – 40%
No. of Motile Sperms – 3million per cc
Non Motile-85%
Motile – 15% (Active 10%, Weak-5%)
What I should do for above such condition.
Dear Herald,
Motility problems can have several causes. Your doctor will tell you if you can take some vitamins or complements in order to enhance the sperm quality. If he thinks that those kind of treatments cannot improve quality the only alternative is to go to a fertility specialist in order to undergo a fertility treatment such as artificial insemination or in vitro fertilisation. Depending on your partner’s fertility and age the specialist will recommend one treatment or the other.
I hope I have been able to help.
Hi Doctor,
I am 44 years old. Here is my semen analysis:
Appearance Grey
Liquefaction Time 30mins
Viscosity Viscous
Volume 0.5ml
Fructose Positive
Ph 8.0
Sperm Concentration 56
Total Motility(PR+NP) 35
Progressive Motility(PR) 25
Non Progressive Motility(NP) 10
Immotility(IM) 65
Strict Morphology(normal forms,%) 40
PUS Cells 2-3 /hpf
RBC Nil /hpf
Round Cells 3-4
What is the chance of having a baby naturally? Can ICSI / PGD help?
Thanks
Dear Sandeep,
Your semen analysis shows lower volume and motility than what is expected in a normal sample. This might lead into having some trouble to conceive naturally. Having a baby naturally is not impossible but, since it can be complicated to achieve, I recommend that you visit a fertility specialist.
With your analysis result it is possible to perform FIV or ICSI, and PGD might not be necessary. Therefore, a fertility specialist would recommend some more tests, specially to you your wife, and then decide with all the result which is the technique that suits your case the best.
I hope I have been able to help.
Best of lucks.