Sperm that show low motility or are immobile are not able to reach the egg to fertilize it, so sperm mobility is a fundamental sperm quality parameter to achieve a natural pregnancy.
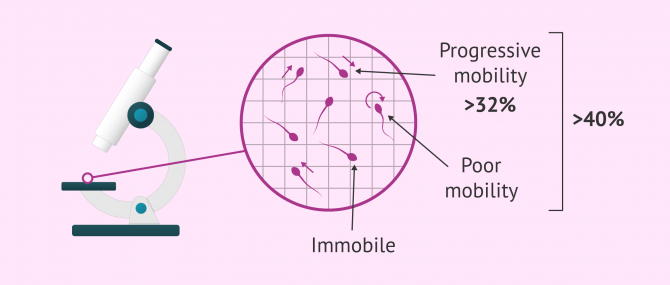
It is analyzed through a semen analysis report and is considered to be altered when the number of progressively motile spermatozoa is less than 32% or the total number of motile spermatozoa in the ejaculate is less than 40%.
Thanks to in vitro fertilization (IVF) treatments, it is possible to achieve pregnancy despite reduced seminal mobility, even in cases where only live, immobile sperm are present.
Provided below is an index with the 9 points we are going to expand on in this article.
- 1.
- 2.
- 3.
- 4.
- 5.
- 6.
- 6.1.
- 6.2.
- 6.3.
- 6.4.
- 6.5.
- 6.6.
- 7.
- 8.
- 9.
Sperm motility analysis
Sperm motility is assessed by a semen analysis called seminogramo semen analysis report. To perform this analysis, the male must provide the andrology laboratory with a semen sample in an approved vial with his name on it. It will be obtained by masturbation after 3-5 days of sexual abstinence.
With this sample, the movement of the sperm will be studied under the microscope by analyzing a small drop in Makler's or Neubauer's camera.
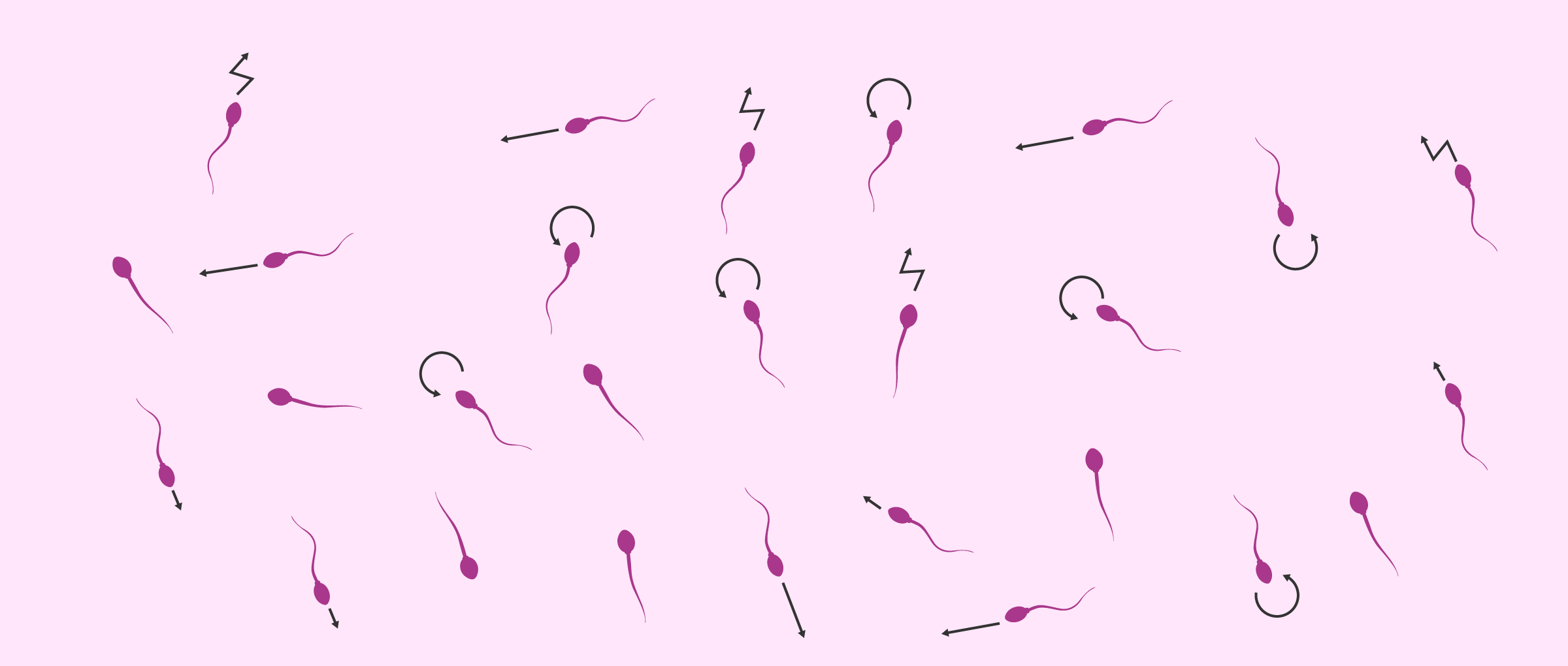
When carrying out this study, it is not only important to know whether they move or not, but also to analyze the way they move. Thus, firstly, the total percentage of mobile and immobile spermatozoa is analyzed and, secondly, the movement of mobile spermatozoa is specified:
- Progressivity
- is analysed whether the mobility is progressive or not. If the sperm do not manage to advance in distance, crossing the female reproductive system to reach the egg will be very complicated.
- Form of movement
- is indicated if the sperm move in a straight line or in a circle or zigzag.
- Speed
- is noted whether the movement is fast or slow.
It is also possible to calculate the total number of viable spermatozoa in the ejaculate, i.e. the living spermatozoa, both mobile and immobile.
It is important to note that not all laboratories perform the seminogram in the same way concerning motility. Some centers only distinguish between mobile and immobile spermatozoa, and others that are more detailed and indicate whether the movement is progressive, rapid, or rectilinear.
Considering undergoing a fertility treatment? By getting your individual Fertility Report your will see different clinics especially selected for you out of the pool of clinics that meet our strict quality criteria. Moreover, it will offer you a comparison between the fees and conditions each clinic offers in order for you to make a well informed choice.
Types of sperm mobility
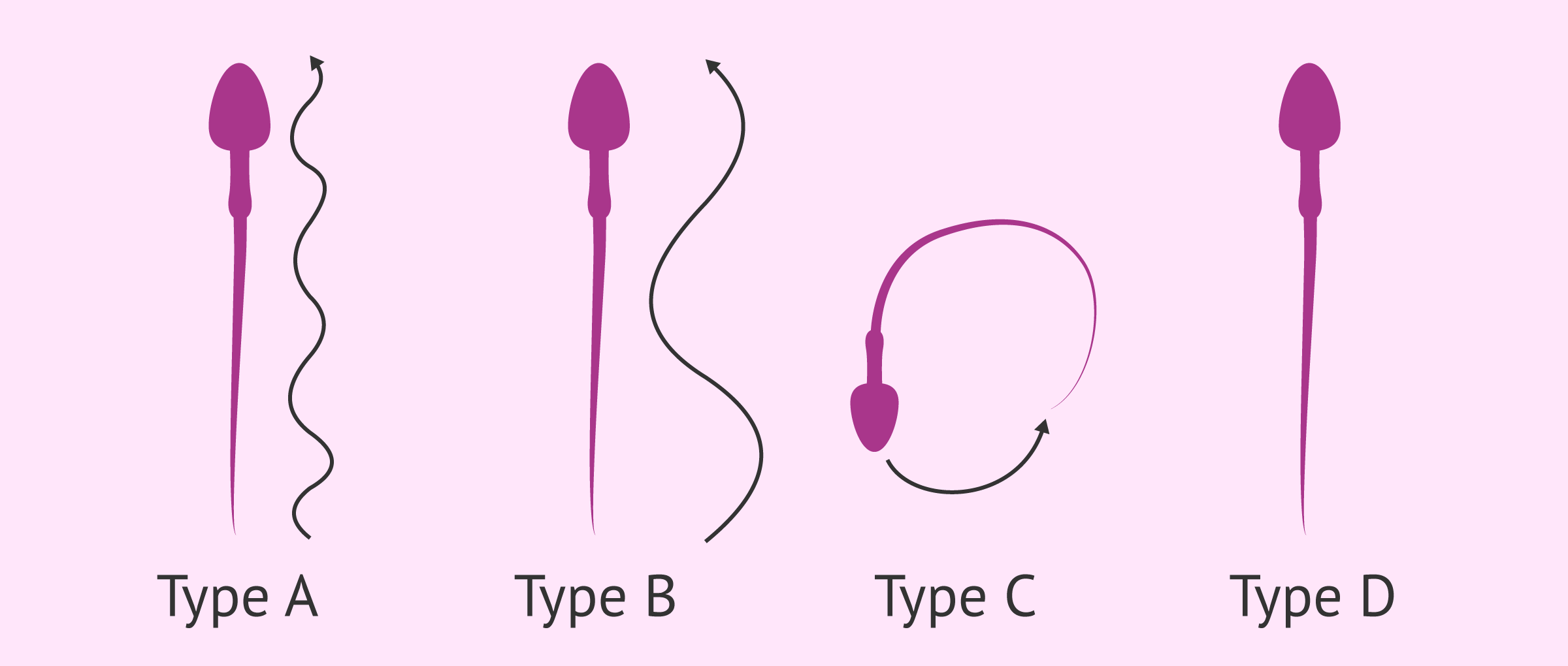
Although not all assisted reproduction centers use it, there is a classification of sperm mobility based on the parameters mentioned above:
- Motility type A or grade 3 (+++)
- group of spermatozoa with progressive, rapid and rectilinear mobility.
- Motility type B or grade 2 (++)
- sperm move progressively but slowly.
- Motility type C or grade 1 (+)
- the motility of the sperm is slow and undisturbed. No progression is observed, but they move over the same position.
- Motility type D or grade 0
- this is the group of static or immobile spermatozoa, both living and dead.
When do you speak of motility problems?
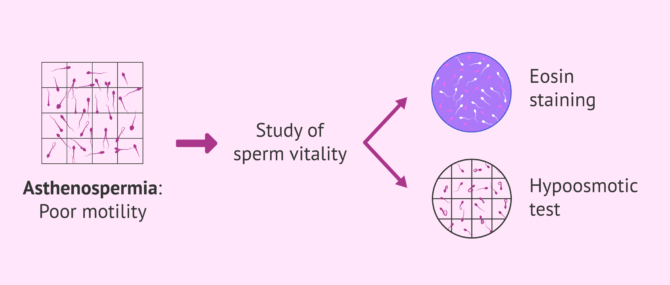
The pathology associated with sperm mobility is called asthenozoospermiaor asthenospermia. It is defined as a sperm alteration characterized by low sperm motility.
Although the World Health Organisation (WHO) has published an update of the Laboratory Manual for Semen Testing and Processing in 2021 (the sixth edition), the most common approach is to continue to follow the criteria of the fifth edition (2010).
According to the reference values of seminal quality established by the WHO (World Health Organization) in 2010, a man suffers from asthenozoospermia when the number of progressively motile spermatozoa (type A + B) is less than 32% and when the total number of motile spermatozoa in the ejaculate (type A+B+C) is less than 40%.
This alteration can be a reason for infertility and is therefore considered a male fertility problem.
There are several alterations that lead to the appearance of sperm motility problems. However, in many cases this pathology is of unknown origin and has no specific treatment.
In these cases, the treatment to improve sperm motility is based on the administration of antioxidants, such as vitamins C and E.
Sperm Vitality and Mobility
As we have mentioned before, mobility is not always related to vitality.
Although dead sperm can't move, not all sperm that don't move are dead. Therefore, there are live, immobile sperm that, although not viable for natural pregnancy, could be used to fertilize eggs by intracytoplasmic sperm injection (ICSI).
Therefore, it is possible to have children even with asthenozoospermia, as long as we find living sperm among the immobile ones.
There are tests, such as the eosin test or the hypo-osmotic test, which detect the vitality of spermatozoa that do not move and allow us to distinguish between those spermatozoa that do not move due to deterioration or failure of their mobility machinery and those that do not show movement because they are dead.
You can learn more about these analyses by accessing the following link: Sperm vitality tests.
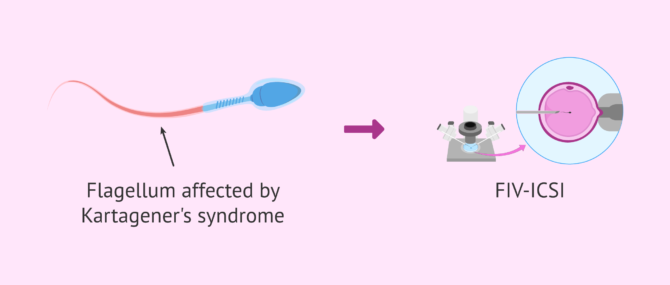
Kartagener's Syndrome
There is a pathology related to sperm mobility called Kartagener's syndrome. This is an unusual disease in which all the sperm are immobile but not all of them are dead.
The lack of mobility is due to an alteration in which the cells do not present ciliary movement, but whoever suffers it suffers its consequences in the respiratory tract so that one is aware of its condition before the search for pregnancy.
Although there is currently no definitive solution for this syndrome, pregnancies have been described using the ICSI technique in cases of patients who suffer from it, so they can be parents.
If you are interested in finding out more about this syndrome, we recommend you read this article: Kartagener Syndrome: Definition, Causes and Symptoms.
FAQs from users
What happens if progressive sperm motility is above 32% but total motility is below 40%?
When performing a basic semen study, sperm motility is an important parameter that can be decisive in the diagnosis and selection of the most appropriate treatment.
In terms of motility, three types of spermatozoa are determined: progressively motile (PM), non-progressively motile (NP) and immotile (IM). MPs are those spermatozoa that move and are mobile. NPs, on the other hand, refer to spermatozoa that are semi-motile, but are not able to move. Finally, immotile spermatozoa neither move nor are able to move.
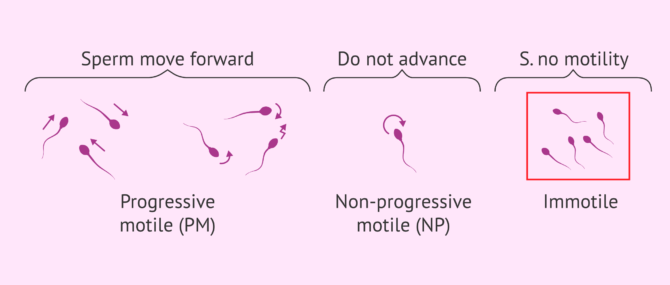
According to the WHO, the MP should be higher than 32% and the sum of MP and NP higher than 40%. Samples with values below the reference values are diagnosed as asthenozoospermia.
Although a priori the motility criteria contemplate, on the one hand, progressive motility and, on the other, the sum of total motility (MP and NP), at the time of diagnosis only MP is taken into account, which must be greater than 32%. Therefore, if the percentage of motile spermatozoa in a sample is higher than 32%, it will be considered as normal motility.
When performing a basic semen study, sperm motility is an important parameter that can be decisive in the diagnosis and selection of the most appropriate treatment.
In terms of motility, three types of spermatozoa are determined: progressively motile (PM), non-progressively motile (NP) and immotile (IM). MPs are those spermatozoa that move and are mobile. NPs, on the other hand, refer to spermatozoa that are semi-motile, but are not able to move. Finally, immotile spermatozoa neither move nor are able to move.
According to the WHO, the MP should be higher than 32% and the sum of MP and NP higher than 40%. Samples with values below the reference values are diagnosed as asthenozoospermia.
Although a priori the motility criteria contemplate, on the one hand, progressive motility and, on the other, the sum of total motility (MP and NP), at the time of diagnosis only MP is taken into account, which must be greater than 32%. Therefore, if the percentage of motile spermatozoa in a sample is higher than 32%, it will be considered as normal motility.
However, it is important to emphasise that, for a correct diagnosis, days of abstinence should be limited to 2-7 days. Prolonged abstinence, longer than 7 days, may have a negative impact on some parameters, such as motility. The percentage of motile spermatozoa decreases as the days of abstinence increase, so it is essential to take this into account.
What happens when there are problems with sperm motility?
When there are mobility problems in the sperm, we speak in medical terms of asthenozoospermia. So, the higher the percentage of immobile or slow spermatozoa, the more difficult it is to achieve a natural pregnancy.
In most cases where there is an alteration in sperm motility, it will be more difficult for the sperm to travel all the way to reach the egg and fertilize it. Therefore, it will be necessary for those patients with asthenozoospermia to resort to some assisted reproduction technique to achieve pregnancy. Specifically, the most appropriate treatment would be in vitro fertilization (IVF).
Read more
Can immobile sperm be alive?
Yes. In fact, even though they are not considered to be of good quality, live immobile sperm can be used to fertilize the eggs through ICSI if there is no motility available.
What is lazy sperm?
Colloquially, we speak of lazy sperm when we refer to those with low motility because they are slow.
In some cases, natural pregnancy can be achieved with lazy sperm, but in others, it may be necessary to resort to assisted reproduction treatments to achieve this, especially if there are few motile sperm.
Does alcohol affect sperm motility?
The relationship between alcohol and infertility is commonly accepted. It is true that it has been quantified or studied more in women, as they are more susceptible to the effect of alcohol as they have a faster gastrointestinal absorption and a slower metabolisation. It has also been studied that alcohol consumption can alter hormonal regulation, cause ovulation problems and its prohibitive consumption during pregnancy is well known. But what about men?
A study was carried out at the University of Southern Denmark in which more than 1000 men took part and assessed their semen quality and hormone values and how and in what quantity they consumed alcohol. The study concluded that the higher the amount of alcohol consumed, the lower the semen quality, especially the sperm concentration. Alcohol consumption can reduce testosterone production and thus the amount of mature sperm, affecting both quality and motility.

The recommendation is to reduce or avoid alcohol intake at least 3 months before trying to conceive or undergoing Assisted Human Reproduction treatment in order to maximise the quality of the gametes. There are genetic and biological factors that we cannot modify to improve our fertility, but there are others, such as leading a healthy life, that we can and that depend solely on us.
Can sperm motility in the ejaculate be improved?
Depending on the reason for the impaired sperm motility, certain recommendations can be applied to reduce the number of spermatozoa.
For example, it is advisable to follow a healthy diet by eating fruits, vegetables, dairy products and avoiding refined foods or trans-fatty acids. Alcohol and tobacco should also be avoided, as well as exposure to certain chemicals.

Getting proper rest and losing weight may also help improve sperm motility, as well as reducing stressful situations.
Suggested for you
As we have mentioned, the alteration of sperm mobility is called asthenozoospermia. In this link you can find more information about this one: Definition, causes and treatment of asthenozoospermia.
Sperm mobility is analysed by means of a spermobiogram. If you want to know more about this test, we recommend that you read the following article:
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Andrade-Rocha FT (2003).Semen analysis in laboratory practice: an overview of routine test. J Clin Lab Anal 2003; 17: 247-258 (View)
Centola GM, Herko R, Andolina E, and Weisensel, S. (1998). Comparison of sperm separation methods: effect on recovery, motility, motion parameters, and hyperactivation. Fertil. Steril., 70 (View)
Guzick DS, Overstreet JW, Factor-Litvak P, Brazil CK, Nakajima ST, Coutifaris C, et al. (2001). Sperm morphology, motility, and concentration in fertile and infertile men. N Engl J Med 2001; 345: 1388-1393 (View)
Kvist U, Björndahl L. ESHRE Monographs: Manual on Basic Semen Analysis. Oxford: Oxford University Press, 2002.
Male infertility best practice policy committee of the American Urological Association (AUA). The optimal evaluation of the infertile male. AUA Best Practice Statement. Revised, 2010 (View)
Sigman M, Zini A. (2009). Semen analysis and sperm function assays: what do they mean? Semin Reprod Med; 27: 115-123 (View)
Sociedad Española de Fertilidad (SEF) (2011). Manual de Andrología. Coordinador: Mario Brassesco. EdikaMed, S.L. ISBN: 978-84-7877 (View)
FAQs from users: 'What happens if progressive sperm motility is above 32% but total motility is below 40%?', 'What happens when there are problems with sperm motility?', 'Can immobile sperm be alive?', 'What is lazy sperm?', 'Does alcohol affect sperm motility?' and 'Can sperm motility in the ejaculate be improved?'.