Normozoospermia or normospermia is the term used by specialists to refer to a normal semen sample, that is, without any alteration that indicates a problem of sperm quality or male infertility.
The concept of normozoospermia can be found in the final result of the seminogram report, the test that evaluates semen quality.
In order for a semen sample to be considered normozoospermic, it must meet the parameters set by the World Health Organization (WHO) in 2010,although there was an update in 2021. When any of the semen parameters are altered, the semen sample cannot be classified as normozoospermic.
Provided below is an index with the 7 points we are going to expand on in this article.
- 1.
- 2.
- 2.1.
- 3.
- 4.
- 4.1.
- 4.2.
- 4.3.
- 4.4.
- 4.5.
- 4.6.
- 4.7.
- 5.
- 6.
- 7.
Basic Spermogram
The semenogram or spermogram is the most important test to assess male fertility. This study consists of evaluating a semen sample obtained by masturbation. Seminal parameters that can be observed with the naked eye are analyzed, as well as others that require the use of a microscope.
First of all, the laboratory staff that collects the sample performs a macroscopic examination of the semen, in which they assess the following parameters:
- Liquefaction.
- Volume.
- Color.
- Viscosity.
- pH.
This is followed by a more thorough microscopic examination, in which all parameters related to spermatozoa or other microscopic cells are determined:
- Sperm count
- Sperm velocity.
- Sperm morphology.
- Vitality of spermatozoa.
- Presence of leukocytes or immature cells.
Each and every one of these parameters will provide information about seminal quality and possible infertility alterations that the male may suffer.
Assisted procreation, as any other medical treatment, requires that you rely on the professionalism of the doctors and staff of the clinic you choose. Obviously, each clinic is different. Get now your Fertility Report, which will select several clinics for you out of the pool of clinics that meet our strict quality criteria. Moreover, it will offer you a comparison between the fees and conditions each clinic offers in order for you to make a well informed choice.
What are the reference values?
Once the results of the spermogram have been obtained, they should be compared with reference values to see if they are within the normal range or not.
Although the World Health Organization (WHO) has published an update of the Laboratory Manual for Semen Examination and Processing in 2021 (the sixth edition), the most common practice is to continue to follow the criteria of the fifth edition (2010).
Specifically, to ensure that the man has normozoospermia and therefore does not have sterility due to a sperm factor, the semen parameters must be equal to or greater than the following values:
- Semen volume
- 1.5 ml.
- Sperm concentration.
- 15 million per ml or 39 million in total per ejaculate.
- Sperm motility.
- 40% motile spermatozoa or 32% progressively motile spermatozoa.
- Sperm Morphology.
- 4% normal sperm.
- Sperm Vitality
- 58% normal sperm.
These indicated values correspond to the lower reference limits (LRI) of the semen parameters. This means that, in order for a male to be considered fertile or normozoospermic, his seminal parameters must be higher.
Other parameters
Although the sperm parameters mentioned in the previous section are the most important for assessing semen quality, there are also other parameters related to semen and its components that can provide relevant information.
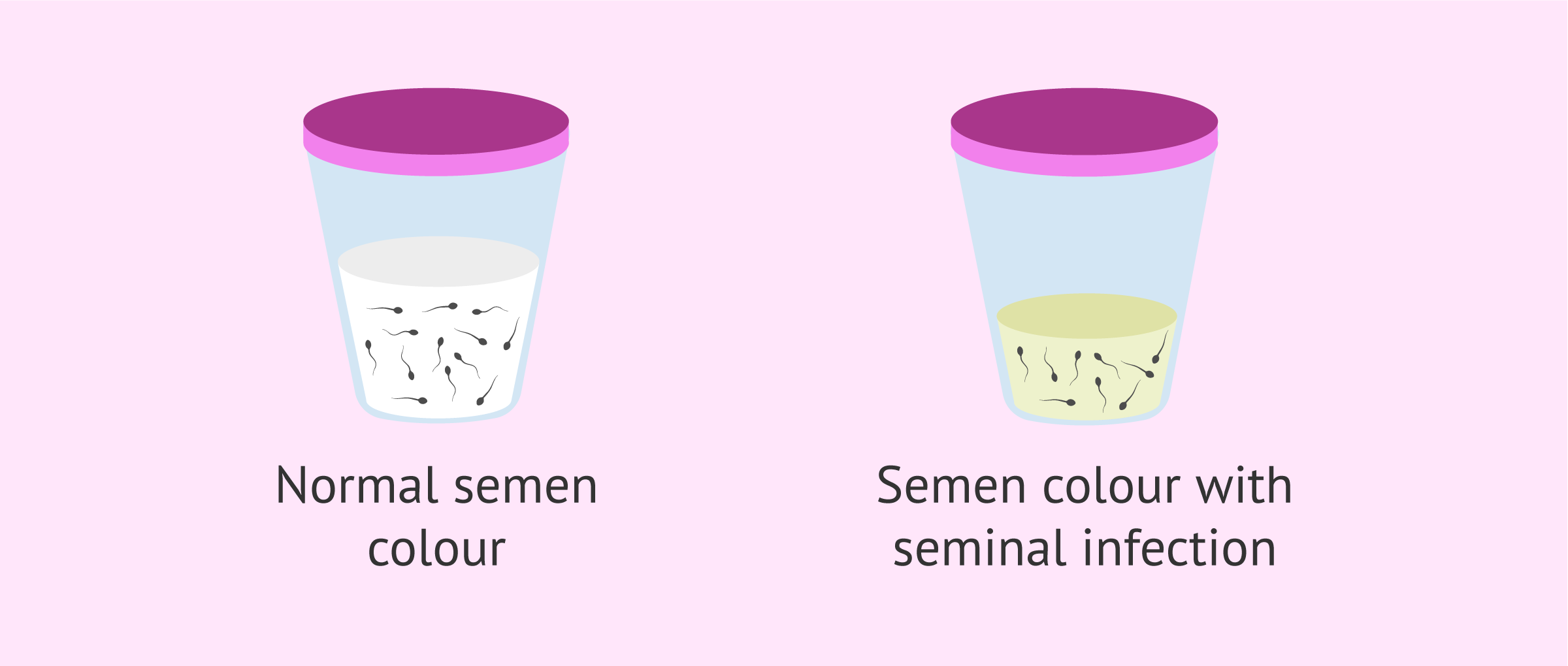
For example, the color of semen must be white-gray to be considered normal. A yellowish semen is related to seminal infection.. In addition, its viscosity should not be too high.
As for the pH of the semen, it should be kept in the 7-8 range. Variation in pH may also indicate infection.
On the other hand, the concentration of leukocytes or round cells in the semen should not be higher than 1 million per ml to rule out problems in spermatogenesis or infections.
Normozoospermia and pregnancy
As has been mentioned throughout the article, those men who present a semen analysis with a result of normozoospermia, do not have any sperm alteration. Therefore, pregnancy in a natural way would be possible.
However, if you have been having sex for more than a year without success, it is best to consult a fertility specialist. It is possible that there is some alteration in the DNA of the spermatozoa and this cannot be detected by a semen analysis. The main consequence of alterations in sperm DNA is usually fertilization failure, but it can also cause embryo implantation failure in the uterus. Therefore, the pregnancy would not go to term.
FAQs from users
Why can't I have a baby if my semen analysis results are normal?
In order to have a child, many factors are involved, in addition to the spermatozoa. In order to achieve pregnancy, it is necessary to have a good ovarian reserve and a correct ovulatory process. There must also be a correct anatomical structure of the female reproductive system, which after all is where fertilization and the development of the pregnancy will take place.
On the other hand, it is important that a spermiogram evaluates aspects of the semen, but not all of them. There are specific cases that require special sperm studies, which are requested on a case-by-case basis.
For the reasons mentioned above, it is very important to perform a complete study on both members of a couple. This should include the necessary tests to determine the cause or causes capable of producing difficulties in the reproductive process, since having a clear diagnosis of the problem will indicate the most appropriate treatment to solve the problem or problems and thus offer the best chance of success, which is none other than having a healthy baby, which is the ultimate goal of every couple seeking advice when they have difficulty conceiving.
Despite normozoospermia we aren't able to get pregnant. Which other tests could we get done?
As stated in the Manual of Andrology of the Spanish Society of Fertility: "although the results of semen analysis can give us information about problems in the function of the male genital organs, they do not allow us to determine with certainty whether an individual is fertile or not". So, if the semen analysis is normal, should other tests be performed? In the initial assessment of a couple with reproductive dysfunction, no. The seminogram is more a tool to guide treatment than to reach a diagnosis.
It is true that there are other complementary tests that can help to study the semen in greater depth, such as the study of the double-stranded DNA fragmentation of the spermatozoa. This type of test promises to advance in the evaluation of the male but even so, we insist, they are not indicated in the initial study of a couple with reproductive dysfunction. Even if you have normozoospermia.
Read more
Can I have a male fertility problem if I have been diagnosed with normozoospermia?
The diagnosis of normozoospermia refers to semen that meets the parameters defined by the WHO in the seminogram. It is an observer-dependent, variable test (as men do not always have the same number of spermatozoa or motility at all times in their lives) and is really old and not very technological.
To date, we have few tools for a more in-depth assessment of the male factor. However, in recent years, male factor research has made great advances, such as sperm DNA fragmentation, sperm apoptosis, altered sperm DNA protonation and FISH in spermatozoa.
There are also many known cases of couples with sperm-attributable failures in which the sperm values of all tests performed were normal, but in which success was only achieved after sperm donation therapy (these are rare cases in which all known tests and therapies have been tried beforehand).
The alterations in all the parameters and tests mentioned above could explain male fertility problems that could occur with a normal sperm count.
Read more
Can oligozoospermia go away on its own and result in normozoospermia?
Yes. Sperm quality varies quite often and is dependent on lifestyle factors. It is likely that stress or the flu affect spermatogenesis, and the results of a semen analysis report appear altered, including problems of oligozoospermia, asthenozoospermia, etc.
The good news is that a man can recover his fertility within 3 months if the cause of infertility is improved or disappears. A balanced diet, doing sports, and quitting toxic habits can contribute to improving sperm quality to a large extent.
Is normozoospermia possible with increased viscosity levels?
Viscosity is more related to the composition of the semen than with spermatozoa themselves. Even though high viscosity levels rarely cause male infertility, it might be associated with sperm motility issues. For this reason, it should be taken into account when performing a semen analysis.
Moreover, too high viscosity levels are associated with prostate complications
Can I get my wife pregnant with normozoospermia?
In principle, yes. As explained above, normozoospermia means normal sperm, which is considered the ideal scenario to conceive according to the WHO's guidelines.
A man with good sperm quality is someone whose sperm are able to travel through the female reproductive tract and reach the egg.
In spite of that, it is possible for sperm to carry DNA abnormalities that cannot be detected through a basic semen analysis. In that case, in spite of being normozoospermic, fertilization or implantation failure could take place.
Can I have normozoospermia if I have hypospermia?
No. Normozoospermia is the term used to refer to semen samples that have all parameters within the normal range.
However, hypospermia is a sperm disorder characterised by a low ejaculate volume. If the rest of the sperm parameters are within normal, the diagnosis would only be hypospermia.
Suggested for you
If you have just had a semen analysis and you are not very clear about the values you have obtained, we recommend that you continue reading here: Sperm Test Results Explained - Interpretation & Normal Values.
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Bartoov B, Eltes F, Pansky M, Lederman H, Caspi E, Soffer Y. Estimating fertility potential via semen analysis data. Hum Reprod 1993;8:65 – 70 (View)
Check JH, Bollendorf A, Press M, Blue T. Standard sperm morphology as a predictor of male fertility potential. Arch Androl 1992;28:39 – 41.
Chia SE, Tay SK, Lim ST. What constitutes a normal seminal analysis? Semen parameters of 243 fertile men. Hum Reprod 1998;13:3394–3398 (View)
Coetzee K, Kruger TF, Lombard CJ. Predictive value of normal sperm morphology: a structured literature review. Hum Reprod Update 1998; 4:73 – 82 (View)
Guzick DS, Overstreet JW, Factor-Litvak P, Brazil CK, Nakajima S, Coutifaris C, Carson SA, Cisneros P, Steinkampf MP, Hill JA et al. Sperm morphology, motility, and concentration in fertile and infertile men. N Engl J Med 2001;345:1388 – 1393 (View)
Jorge Cuadros Fernández; Lara Andrés Criado; María Morales Morales; María Villa Martínez; José Luis Gómez Palomares; Elisabetta Ricciarelli. Clínica FIVMadrid. Utilización de la cámara microfluídica fertile en casos de fragmentación de la cadena doble del adn de los espermatozoides. Comunicación presentada en el 10º Congreso ASEBIR, Cáceres, 2019.
Lluís Bassas. Seminograma. En: Manual de Andrología (2011). Sociedad Española de Fertilidad.
MacLeod J, Wang Y. Male fertility potential in terms of semen quality: a review of the past, a study of the present. Fertil Steril 1979;31: 103 – 116 (Ver)
Macomber D, Sanders MD. The spermatozoa count: its value in the diagnosis, prognosis and concentration in fertile and infertile men. N Engl J Med 1929;200:981 – 984.
Trevor G. Cooper, et al. World Health Organization reference values for human semen characteristics. Human Reproduction Update, Vol.16, No.3 pp. 231–245, 2010 (View)
FAQs from users: 'Why can't I have a baby if my semen analysis results are normal?', 'Despite normozoospermia we aren't able to get pregnant. Which other tests could we get done?', 'Can I have a male fertility problem if I have been diagnosed with normozoospermia?', 'Can oligozoospermia go away on its own and result in normozoospermia?', 'Is normozoospermia possible with increased viscosity levels?', 'Can I get my wife pregnant with normozoospermia?' and 'Can I have normozoospermia if I have hypospermia?'.