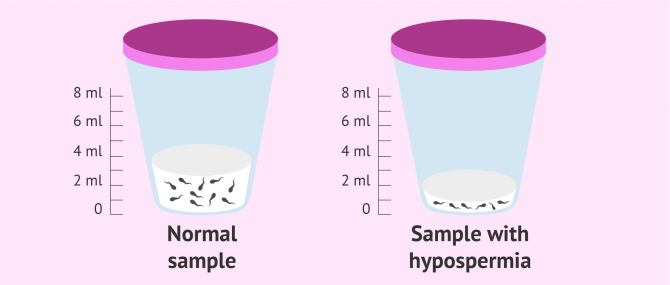
Hypospermia is an alteration in the male semen due to poor ejaculation. The seminal parameter affected in this case is the semen volume, which has a value below 1.5 milliliters (ml).
This alteration in semen volume can be a cause of male infertility if there is difficulty in achieving pregnancy. This is not always the case, since, if the concentration and quality of the spermatozoa are good, the male will be able to conceive and have children without any problem.
Provided below is an index with the 7 points we are going to expand on in this article.
- 1.
- 2.
- 3.
- 3.1.
- 3.2.
- 4.
- 4.1.
- 4.2.
- 4.3.
- 4.4.
- 4.5.
- 5.
- 6.
- 7.
What is hypospermia?
Hypospermia is defined as low volume of ejaculated semen. Taking into account the reference values of the World Health Organization (WHO), hypospermia is diagnosed when the male has a seminal volume of less than 1.5 ml. The test performed to determine the semen volume and diagnose if there is hypospermia or any other semen quality problem is the seminogram or spermiogram.
Sperm volume is considered normal when it ranges between 1.5 and 6 ml according to the reference values published by the World Health Organization (WHO).
However, when the ejaculate volume is too low, that is, when there is almost no semen in the ejaculate, it may be a case of anejaculation (inability to ejaculate in males). It is often caused by a blockage or retrograde ejaculation.
Get more info by clicking the following link: Post-Testicular Factors of Male Infertility - Causes & Treatment.
Causes of low seminal volume
The decrease in semen production in the male is usually related to two main organs: the vesicles and the prostate. In addition, it should be noted that the volume of semen decreases gradually over the years due to the aging of the male. This is a natural process and is not associated with any disease or ailment.
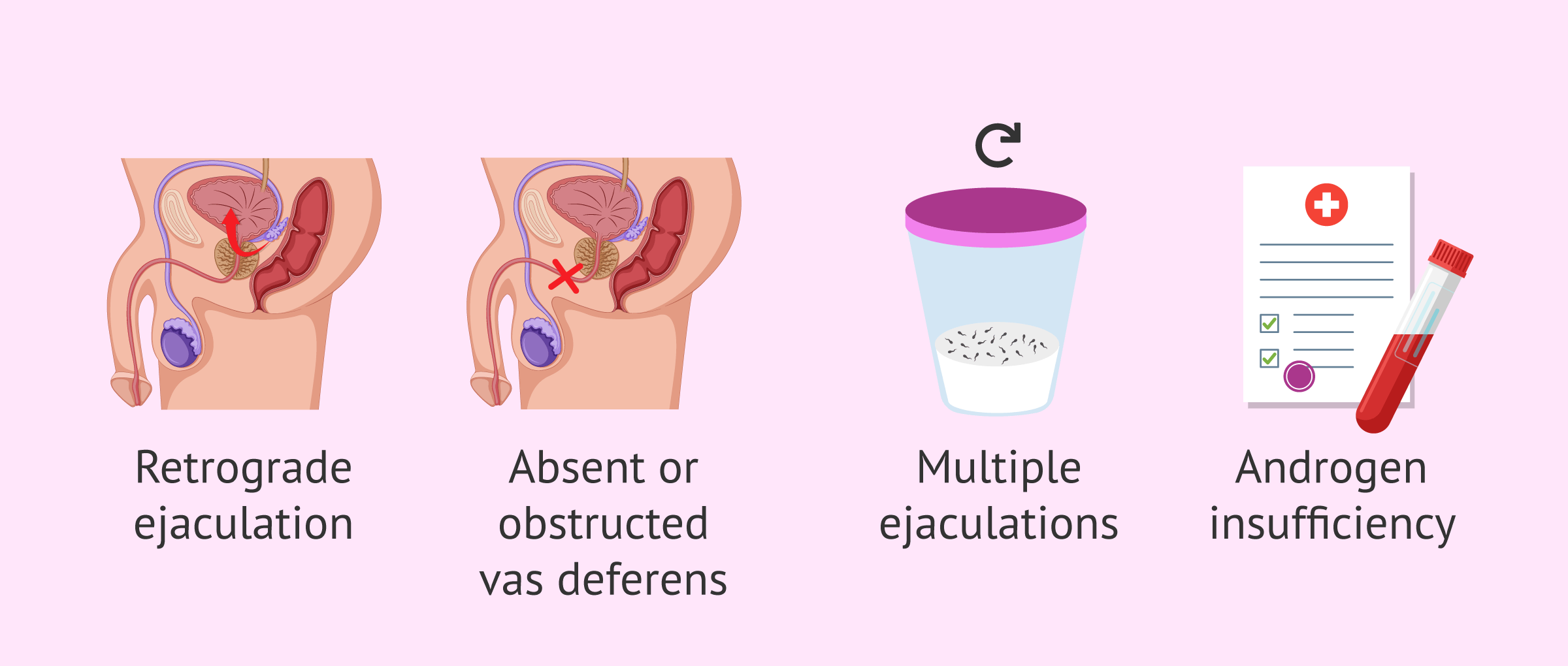
On the other hand, hypospermia can be caused by the following factors:
- Partial retrograde ejaculation
- Sperm travel toward the bladder when the man ejaculates. It can be caused by congenital anomalies of the male urethra or medications to treat prostatic hyperplasia. It has been associated with prostate surgery as well.
- Vasa deferentia and seminal vesicle agenesis
- As a consequence of a congenital anomaly of the male genital organs.
- Ejaculatory Duct Obstruction (EDO)
- Due to an inflammation or infection in the ejaculatory ducts, like prostatitis or varicocele.
- Androgen Insensitivity Syndrome (AIS)
- It occurs when a person who is genetically male is resistant to male hormones (i.e. androgens), either partially or totally.
- Neurologic erectile dysfunction
- Loss of the nerve impulses that travel through the penis.
- Ejaculating too much
- Repeated ejaculation result in lower sperm volume.
- Bladder Neck Incision (BNI)
- In men with problems passing urine.
Some studies have shown that men who smoke or have overweight problems may have a lower amount of ejaculate as well.
In any case, your urologist should examine your case in detail in order to detect the presence of other severe conditions that may be going unnoticed.
Hypospermia and fertility
To assess semen quality in a semen analysis it is necessary that the patient comes with a sexual abstinence between 3 and 5 days. If ejaculation occurs before this time and the semen volume is lower than normal, it is possible that the hypospermia is due to this and not to major problems.
Nevertheless, having hypospermia does not necessarily mean that there is a sterility problem. If the man has a poor ejaculation, the total amount of sperm in the ejaculate is likely to be lower than that of another man without hypospermia. However, the sperm count per milliliter may be good and the sperm may show adequate morphology and motility.
In the opposite case, a man with a larger ejaculate volume but poor sperm motility and/or morphology may have the same chances of achieving pregnancy as a man with hypospermia but whose sperm are better and with high fertilizing capacity.
Although hypospermia is most often related to oligospermia or low sperm concentration, this is not always the case.
If, when seeking pregnancy, hypospermia delays or prevents this goal, the following solutions can be tried:
Are there medical treatments?
There is no definitive treatment that favors the production of more semen. There are only different commercial pills or dietary supplements that can help improve the level of semen.
If the lack of semen volume is caused by a condition in the seminal vesicle or prostate, a surgical intervention could be performed to solve the problem, although it is not always possible to increase the final volume of semen.
Hypospermia and assisted reproduction
If any other problem besides hypospermia is diagnosed in the semen analysis, such as low motility (asthenospermia) or morphological alterations (teratospermia), the probability of achieving pregnancy will be severely diminished.
Therefore, it will be necessary to resort to assisted reproductive techniques such as artificial insemination (AI) or in vitro fertilization (IVF) depending on the parameters obtained.
Assisted procreation, as any other medical treatment, requires that you rely on the professionalism of the doctors and staff of the clinic you choose. Obviously, each clinic is different. Get now your Fertility Report, which will select several clinics for you out of the pool of clinics that meet our strict quality criteria. Moreover, it will offer you a comparison between the fees and conditions each clinic offers in order for you to make a well informed choice.
If there is aspermia or total absence of ejaculate, special techniques for sperm collection prior to fertility treatment, such as epididymal aspiration or testicular biopsy should be used.
FAQs from users
Is treatment for hypospermia necessary?
Hypospermia is defined as a decrease in ejaculate volume below 2.5 ml. According to the World Health Organization (WHO), the regular volume of normal semen ejaculated by a healthy man should be between 1.5 and 6 ml of the total ejaculated fluid.
Treatment is based primarily on the specific cause that is causing the hypospermia, so it is essential to first find the cause. It may require restorative surgery, lifestyle changes or a change in medication.
Could the low ejaculation be due to previous ejaculation?
Yes, this is one of the causes of hypospermia. Therefore, it is not recommended to have sexual intercourse several times a day if you are looking for pregnancy. In order to correctly assess the semen volume, the man must remain sexually abstinent for 3 days.
What are the symptoms of retrograde ejaculation?
Retrograde ejaculation occurs when the opening of the bladder does not close and sperm is directed there instead of being expelled from the penis. Symptoms are low ejaculate volume and cloudy urine after orgasm.
Is teratozoospermia related to hypospermia?
Generally no, Hypospermia refers to a low semen volume, less than 1.5 ml total. Therefore, hypospermia is related to oligospermia, that is, a low number of spermatozoa in the ejaculate.
However, a male who presents both alterations, hypospermia and teratospermia, will have a much higher degree of infertility and the possibility of achieving a natural pregnancy will be very limited.
What is the difference between hypospermia, aspermia and azoospermia?
These three terms refer to different seminal alterations. First, hypospermia is characterized by a low semen volume in the male, specifically, less than 1.5 mL. However, it is possible that the rest of the semen parameters are within the normal range.
Secondly, aspermia is the total absence of ejaculation in the male. Therefore, it is also known as anejaculation.
Finally, azoospermia refers to the absence of sperm in the ejaculate. The male is able to ejaculate a normal volume of semen, but it is not possible to find any sperm. Therefore, pregnancy would not be possible in a natural way.
Suggested readings
As briefly explained above, a seminogram or semen analysis is a diagnostic test used to detect potential sperm disorders, including hypospermia or low semen volume. You can learn all the details about this common test here: What Is a Semen Analysis Report? – Purpose, Preparation & Cost.
There exist many other sperm disorders that can come along with hypospermia, or even be the cause behind low sperm production. The following post may provide you with a much deeper insight: Sperm Disorders that Cause Male Infertility.
Sperm agglutination is another sperm disorder that can be detected through a semen analysis and can cause a man's sperm to be sticky. Check out this for information: What Is Agglutination in Sperm? – Causes, Symptoms & Treatment.
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
E B BANK. The possibilities of artificial insemination in sterility caused by oligospermia and hypospermia. Z Urol. 1964 Jul;57:517-20.
G Robin, F Marcelli, V Mitchell, C Marchetti, L Lemaitre, D Dewailly, M Leroy-Billiard, J-M Rigot. Why and how to assess hypospermia? Gynecol Obstet Fertil. 2008 Oct;36(10):1035-42. doi: 10.1016/j.gyobfe.2008.04.021.
J D Stephenson, E J O'Shaughnessy. Hypospermia and its relationship to varicocele and intrascrotal temperature. Fertil Steril. Jan-Feb 1968;19(1):110-7. doi: 10.1016/s0015-0282(16)36550-5.
L Coppens. Diagnosis and treatment of obstructive seminal vesicle pathology. Acta Urol Belg. 1997 Jun;65(2):11-9.
R Abid. Hypospermia and the post-coital test. Tunis Med
. 1987 Feb;65(2):109-14.
FAQs from users: 'Is treatment for hypospermia necessary?', 'Does small amount of ejaculate mean low sperm count?', 'Could the low ejaculation be due to previous ejaculation?', 'Does vasectomy affect ejaculate volume?', 'Is having low ejaculate volume a sign of prostate cancer?', 'What are the symptoms of retrograde ejaculation?', 'Can anabolic steroids lead to low sperm volume?', 'Is teratozoospermia related to hypospermia?', 'Does low ejaculate volume mean low testosterone?' and 'What is the difference between hypospermia, aspermia and azoospermia?'.
Authors and contributors
More information about Cristina Algarra Goosman






Hello, with by wife we want to have a baby but pregnancy never shows up… I think my sperm volume is too low, is it because we have sex too often or what’s going on with us?
Dear Patrick Blue,
Ejaculating too much is a common cause of hypospermia, but not the most concerning one. My advice is that you refrain from intercourse for 3-5 days and then undergo a semen analysis to check if everything is okay with the remaining sperm parameters.
I hope this helps,
Best wishes