Sperm microinjection(ICSI) is a widely used assisted reproduction technique. To perform it, the embryologist introduces a spermatozoon directly into the egg in the laboratory, with the help of a microinjector. In this case, the sperm to be microinjected is selected at 400x magnification, according to its motility and morphology.
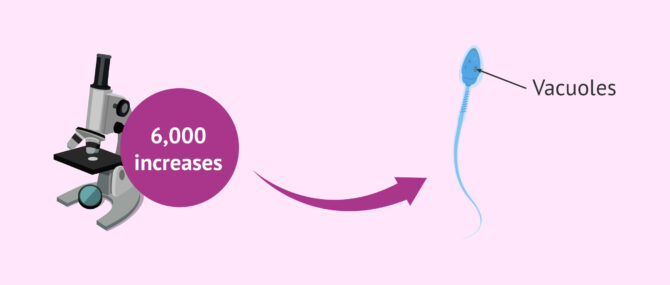
However, it is possible to perform a morphological assessment of the spermatozoa at high magnification (over 6000x) prior to ICSI. This allows a more accurate assessment of sperm morphology and better visualization of the vacuoles in the sperm head. This modified ICSI is called IMSI, which stands for intracytoplasmic morphologically selected sperm injection.
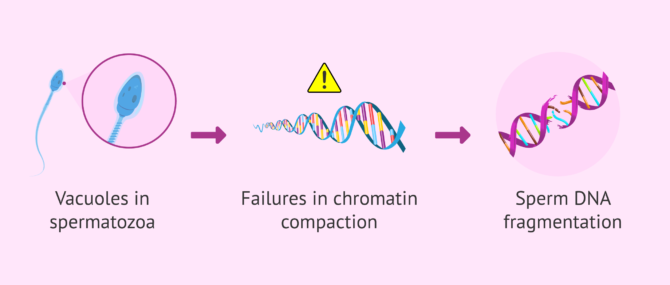
Vacuoles have been associated with defects in sperm chromatin condensation. For this reason, high magnification selection of sperm without vacuoles and IMSI could improve reproductive outcomes.
Provided below is an index with the 6 points we are going to expand on in this article.
What are sperm vacuoles?
Vacuoles in spermatozoa are physiological structures that form during the process of sperm formation and maturation. However, the causes that lead to its appearance are not clear.
These nuclear vacuoles are seen as concavities in the head of the spermatozoon. They are formed from cytoplasm and cell organelles that are not needed, but have not been removed during the sperm formation process. Their importance lies in the fact that these sperm vacuoles have been related to failures in chromatin condensation.
In any case, these vacuoles can only be detected when a morphological selection of spermatozoa is performed at high magnification. Therefore, sperm vacuoles are accurately assessed when IMSI is performed, allowing vacuolated sperm to be ruled out.
Classification
One of the most commonly used criteria for the classification of spermatozoa when performing morphological evaluation at high magnification is the following (Vanderzwalmen criteria):
- Grade I: absence of vacuoles.
- Grade II: two small vacuoles at most.
- Grade III: more than two small vacuoles or at least one large vacuole.
- Grade IV: large vacuoles and associated with other abnormalities.
Thus, as the degree increases, the morphological alterations of the sperm increase.
Implications
The presence of vacuoles in spermatozoa has been related to defects in chromatin condensation. This means that this non-condensed chromatin is "unprotected" and therefore more susceptible to sperm DNA damage. Thus, spermatozoa with vacuoles have been associated with a higher rate of sperm DNA fragmentation.
Thus, if these spermatozoa with vacuoles and chromatin condensation failures are not selected, it has been suggested that they could improve reproductive outcomes. With IMSI there could be an improvement in embryo development to blastocyst, implantation and clinical pregnancy rate and a reduction in miscarriage rate.
However, the superiority of IMSI over ICSI is not very clear in terms of improving these outcomes, which makes IMSI not a routine procedure in current practice in assisted reproduction clinics.
FAQs from users
What are the advantages of IMSI?
Selection of individual sperm under high magnification microscope, (intracytoplasmic morphologically selected sperm injection or IMSI), allows the use of the most apparantly optimal sperm according to shape (morphology) in men with the most severe male factor.
IMSI is considered for patients with recurrent implantation failure or spontaneous miscarriages (Lo Monte et al. 2013) due to the opinion the pregnancy failures were due to a sperm defect. However, recent studies have opposed this view by showing IMSI does not improve outcomes for men undergoing multiple IVF cycles. (Oliveira et al. 2011, Gatimel et al. 2016).
What types of semen anatomical abnormalities exist?
Potential defects or anomalies that can be found in sperm include:
- Head defects
- too small, too large, double-headed, balloon-shaped, with too large vacuoles...
- Midpiece defects
- too thin, too thick, too short, too long, bent, without neck...
- Tail defects
- too short, too long, duplicate tails, coiled, detached tail...
A single spermatozoon can have just one anomaly or, conversely, multiple defects.
In any case, with just an abnormality in one part, the sperm cell is considered an abnormal one.
What test is done to see if there are vacuoles in the sperm?
Vacuoles in the sperm head are detectable when spermatozoa are evaluated at high magnification, known as MSOME. In this case, spermatozoa are observed at more than 6000 magnification, which allows a very accurate assessment of their morphology.
When MSOME is performed to morphologically select the sperm to be microinjected in an ICSI, this modified ICSI is called IMSI.
Suggested for you
If you want to read more information about IMSI, we recommend you to access the following link: What is IMSI - Indications, advantages and disadvantages.
On the other hand, if you want to know more about ICSI, you can do it in this article: What is ICSI and what is its cost?
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Bendayan M, Caceres L, Saïs E, Swierkowski-Blanchard N, Alter L, Bonnet-Garnier A, Boitrelle F. Human Sperm Morphology as a Marker of Its Nuclear Quality and Epigenetic Pattern. Cells. 2022 May 30;11(11):1788. doi: 10.3390/cells11111788. PMID: 35681482; PMCID: PMC9180039. (View)
Berkovitz A, Eltes F, Ellenbogen A, Peer S, Feldberg D, Bartoov B. Does the presence of nuclear vacuoles in human sperm selected for ICSI affect pregnancy outcome? Hum Reprod. 2006 Jul;21(7):1787-90. doi: 10.1093/humrep/del049. Epub 2006 Feb 23. PMID: 16497697. (View)
Ghazali S, Talebi AR, Khalili MA, Aflatoonian A, Esfandiari N. Large nuclear vacuoles in spermatozoa negatively affect pregnancy rate in IVF cycles. Iran J Reprod Med. 2015 Jul;13(7):425-32. PMID: 26494990; PMCID: PMC4609322. (View)
Lukaszuk K, Jakiel G, Wocławek Potocka I, Kiewisz J, Olszewska J, Sieg W, Podolak A, Pastuszek E, Wdowiak A. IMSI-Guidelines for Sperm Quality Assessment. Diagnostics (Basel). 2022 Jan 13;12(1):192. doi: 10.3390/diagnostics12010192. PMID: 35054359; PMCID: PMC8774575. (View)
Mangoli E, Khalili MA. The Beneficial Role of Intra Cytoplasmic Morphologically Selected Sperm Injection (IMSI) in Assisted Reproduction. J Reprod Infertil. 2020 Jan-Mar;21(1):3-10. PMID: 32175260; PMCID: PMC7048693. (View)
Nixon B, Schjenken JE, Burke ND, Skerrett-Byrne DA, Hart HM, De Iuliis GN, Martin JH, Lord T, Bromfield EG. New horizons in human sperm selection for assisted reproduction. Front Endocrinol (Lausanne). 2023 Feb 22;14:1145533. doi: 10.3389/fendo.2023.1145533. PMID: 36909306; PMCID: PMC9992892. (View)
Omidi M, Faramarzi A, Agharahimi A, Khalili MA. Noninvasive imaging systems for gametes and embryo selection in IVF programs: a review. J Microsc. 2017 Sep;267(3):253-264. doi: 10.1111/jmi.12573. Epub 2017 May 4. PMID: 28470749. (View)
Pastuszek E, Kiewisz J, Skowronska P, Liss J, Lukaszuk M, Bruszczynska A, Jakiel G, Lukaszuk K. An investigation of the potential effect of sperm nuclear vacuoles in human spermatozoa on DNA fragmentation using a neutral and alkaline Comet assay. Andrology. 2017 Mar;5(2):392-398. doi: 10.1111/andr.12324. PMID: 28297560. (View)
Simopoulou M, Gkoles L, Bakas P, Giannelou P, Kalampokas T, Pantos K, Koutsilieris M. Improving ICSI: A review from the spermatozoon perspective. Syst Biol Reprod Med. 2016 Dec;62(6):359-371. doi: 10.1080/19396368.2016.1229365. Epub 2016 Sep 20. PMID: 27646677. (View)
Teixeira DM, Hadyme Miyague A, Barbosa MA, Navarro PA, Raine-Fenning N, Nastri CO, Martins WP. Regular (ICSI) versus ultra-high magnification (IMSI) sperm selection for assisted reproduction. Cochrane Database Syst Rev. 2020 Feb 21;2(2):CD010167. doi: 10.1002/14651858.CD010167.pub3. PMID: 32083321; PMCID: PMC7033651. (View)
Vanderzwalmen P, Hiemer A, Rubner P, Bach M, Neyer A, Stecher A, Uher P, Zintz M, Lejeune B, Vanderzwalmen S, Cassuto G, Zech NH. Blastocyst development after sperm selection at high magnification is associated with size and number of nuclear vacuoles. Reprod Biomed Online. 2008 Nov;17(5):617-27. doi: 10.1016/s1472-6483(10)60308-2. PMID: 18983745. (View)
FAQs from users: 'What are the advantages of IMSI?', 'What types of semen anatomical abnormalities exist?' and 'What test is done to see if there are vacuoles in the sperm?'.