The ovarian reserve can be studied using various different tests. Among them, the most common tests to measure the ovarian reserve are:
- Antral follicle count by ultrasound (AFC).
- The assessment of endocrine markers such as AMH, FSH, estradiol or Inhibin B.
In this way, specialists can estimate a woman's ovarian reserve, i.e. the number of eggs still contained in her ovaries at a given time in her reproductive life.
Provided below is an index with the 10 points we are going to expand on in this article.
- 1.
- 1.1.
- 2.
- 2.1.
- 2.2.
- 2.3.
- 3.
- 4.
- 4.1.
- 5.
- 6.
- 7.
- 7.1.
- 7.2.
- 7.3.
- 7.4.
- 7.5.
- 7.6.
- 7.7.
- 8.
- 9.
- 10.
Antral follicle count by ultrasonography (AFC)
Follicles are the ovarian structures where the eggs mature. In each menstrual cycle, a set of follicles begin the maturation process, but only one of them will be able to reach the final stage and release a mature egg in what is known as ovulation. This follicle is called the dominant follicle.
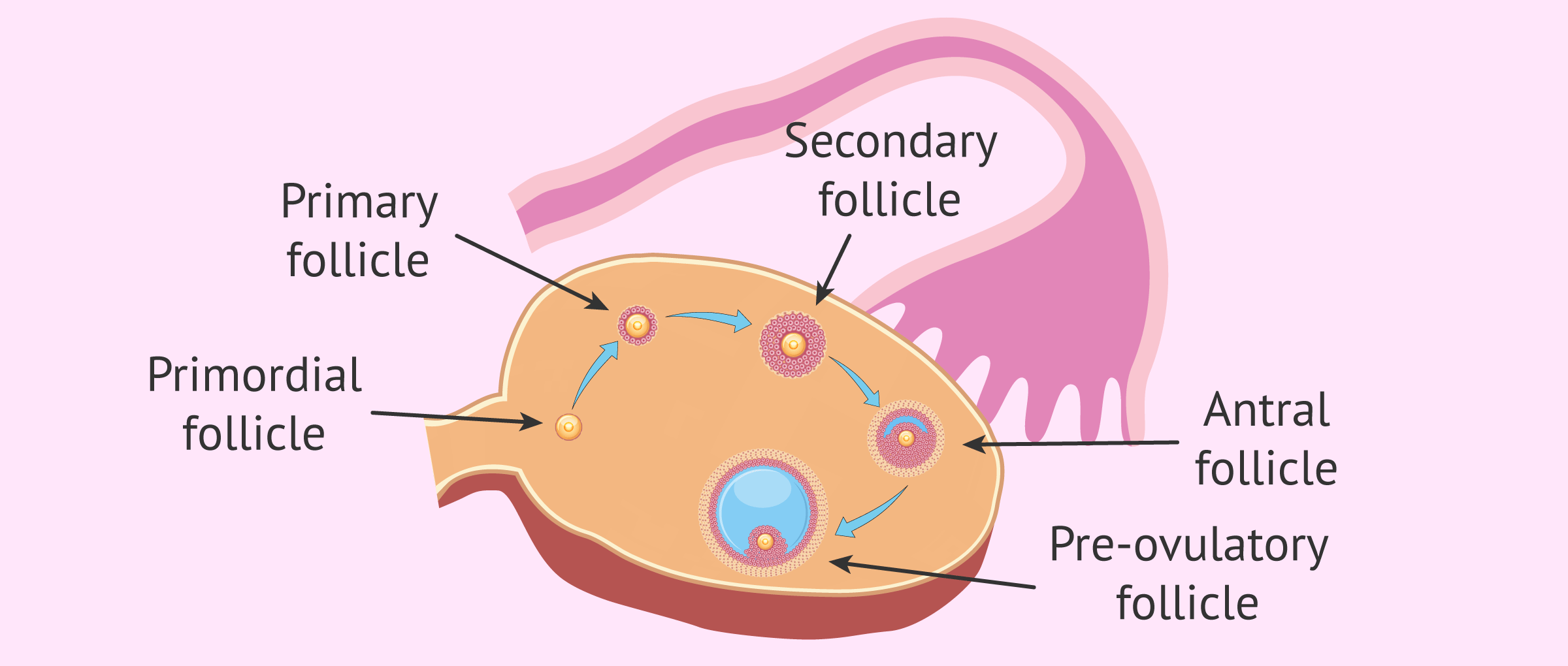
The different stages through which an ovarian follicle passes until it reaches full development are:
- Primordial follicle
- Primary follicle
- Secondary or preantral follicle.
- Tertiary or antral follicle.
- Preovulatory follicle or Graff's follicle.
Antral follicles are characterized by the development of the antrum, a structure formed by the accumulation of fluid in the follicular interior. The antrum allows visualization of these follicles by ultrasound when they have a diameter of about 2 mm.
In this way, by means of transvaginal ultrasound, the specialist can count the number of antral follicles.
What are the normal values in the AFC?
The AFC is widely used to evaluate a woman's ovarian reserve, as it provides valuable information in a non-invasive and painless manner. In fact, the AFC is one of the most widely accepted methods for estimating ovarian reserve in assisted reproduction, together with the determination of anti-Müllerian hormone (AMH), which we will see below.
To make a good assessment of ovarian reserve by AFC, it is advisable to perform this test in the early follicular phase of the woman's menstrual cycle. This means that the AFC should be carried out between the 2nd and 4th day of the cycle.
The menstrual cycle is considered to begin on the first day of the menstrual period.
If the gynecologist counts between 5 to 10 antral follicles in each ovary, the ovarian reserve is considered normal. Conversely, values below 5 or above 10 antral follicles (per ovary) will be interpreted as a low or high ovarian reserve, respectively.
You can read more in-depth about this test at the following link: What is the antral follicle count and what is it for?
Hormonal markers of ovarian reserve
A woman's menstrual cycle is controlled by hormones. Therefore, the analysis of certain hormone values can be helpful in assessing ovarian reserve and in studying a woman's fertility.
Antimüllerian hormone (AMH)
AMH is a hormone produced by the granulosa cells of developing follicles, from secondary follicle to early antral follicle. Therefore, AMH is an indicator of the number of follicles that are growing.
Granulosa cells surround the oocyte and form part of the ovarian follicle.
As ovarian reserve declines with age, so does the number of early antral follicles that produce AMH and thus AMH levels. In this way, the values of this hormone can be related to the number of eggs still remaining in the ovary.
AMH can be measured at any time during the menstrual cycle, although there may be a variation of up to 20% in its levels depending on the day of the cycle on which the test is performed. However, AMH is usually assessed at the beginning of the cycle, at the same time as other hormones.
Considering undergoing a fertility treatment? By getting your individual Fertility Report your will see different clinics especially selected for you out of the pool of clinics that meet our strict quality criteria. Moreover, it will offer you a comparison between the fees and conditions each clinic offers in order for you to make a well informed choice.
Normal values
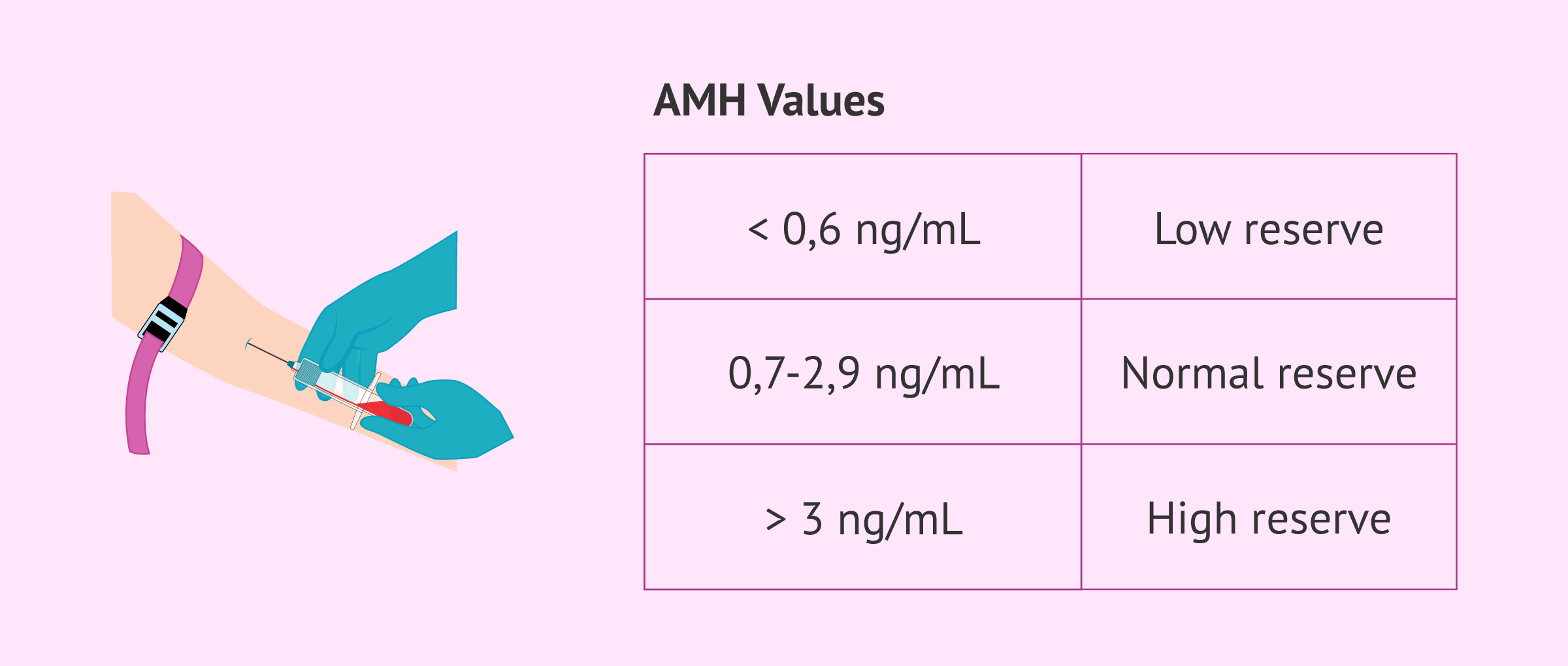
Generally speaking, although there may be some differences between laboratories, reference values for AMH can be established as follows:
- AMH less than 0.6 ng/ml: low ovarian reserve.
- AMH between 0.7 and 2.9 ng/ml: normal ovarian reserve. If AMH is between 0.7-0.9 ng/ml, ovarian reserve has begun to decline, although it is still considered normal.
- AMH greater than 3 ng/ml: good ovarian reserve. If AMH levels are greater than 6 ng/ml, there may be an increased risk of ovarian hyperstimulation syndrome (OHSS) in ovarian stimulation treatments.
Additionally, it is important to note that patients with polycystic ovaries may have higher AMH levels.
If you want to read more information about this widely used ovarian reserve marker, you can read the following article: Antimüllerian hormone: usefulness for studying fertility
Follicle stimulating hormone (FSH)
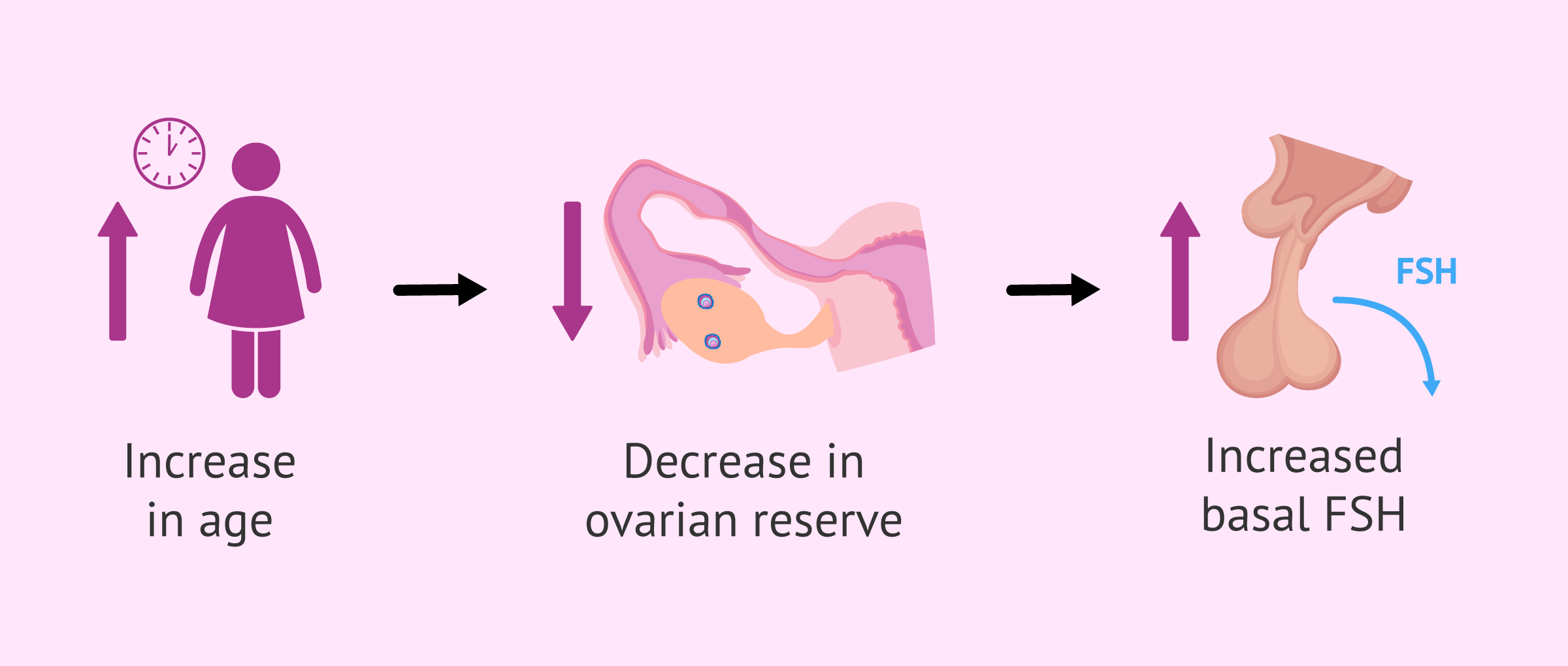
As the age of the woman increases and the ovarian reserve decreases, the base levels of FSH (follicle-stimulating hormone) increase. This is because there is less production of hormones that inhibit ovarian activity, which in turn allows FSH levels to increase.
FSH levels should be measured between the 2nd and 4th day of the menstrual cycle. In addition, this test is often performed in conjunction with measurements of estradiol.
Generally speaking, a basal FSH level above 10 mIU/ml would indicate a low ovarian reserve. Baseline FSH values above 20 mIU/ml are found closer to menopause. On the other hand, normal estradiol values at the beginning of the menstrual cycle are less than 40 pg/ml.
You can read much more about follicle-stimulating hormone in this article: FSH hormone: what are its functions and normal values?
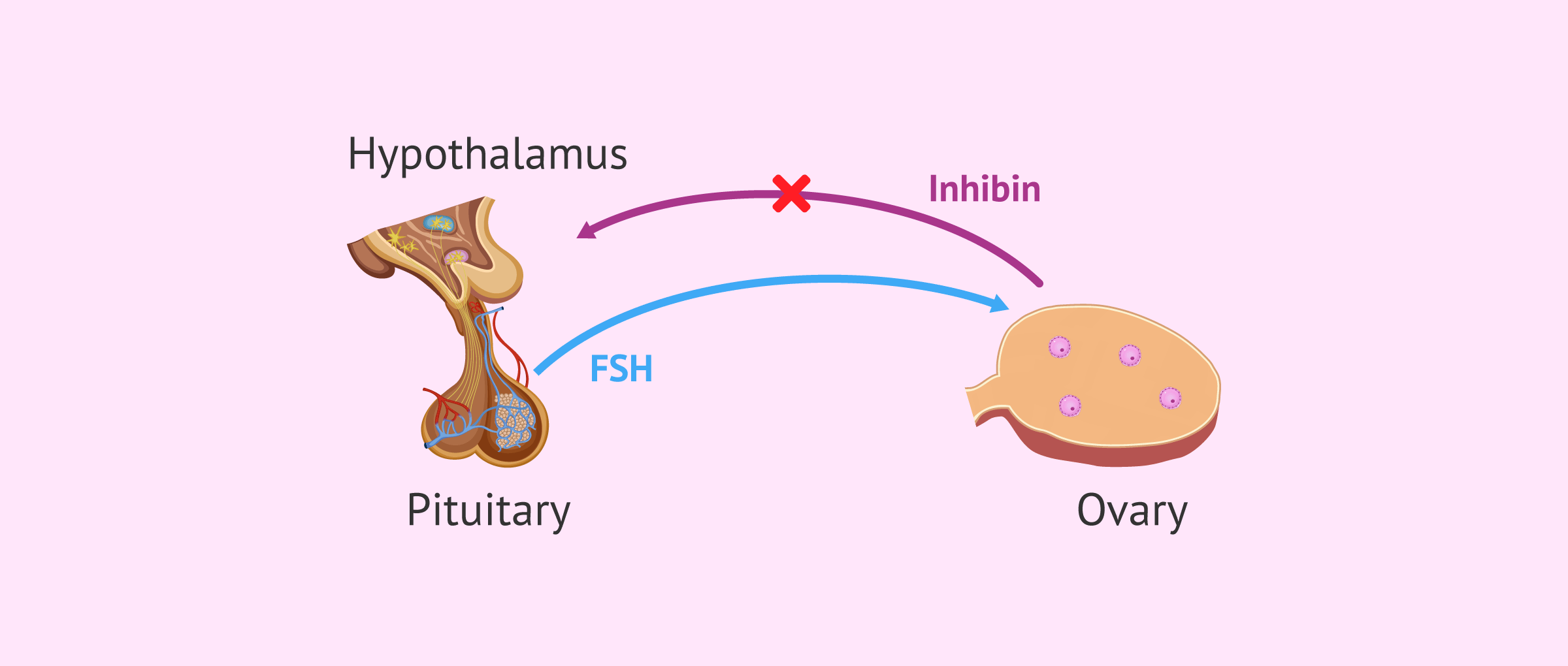
Inhibin B
Inhibin B is a glycoprotein also produced by the granulosa cells of ovarian follicles. Inhibin B concentration is inversely proportional to FSH values since inhibin B suppresses FSH secretion.
Thus, when inhibin B decreases due to the woman's age, the loss of this inhibitory effect allows FSH levels to increase.
Thus, an inhibin B value of less than 35-45 pg/ml is an indicator of poor prognosis, as it may mean alterations in the ovarian reserve.
Dynamic tests
This type of test evaluates the response of the ovary to the stimulus of certain drugs such as clomiphene citrate (CC).
The clomiphene citrate test(CCCT) consists of stimulating the ovary with this drug for 5 days, usually starting on the fifth day of the menstrual cycle. To assess the ovarian response, the FSH hormone is determined before and after the test.
An abnormal test result, such as very high FSH, would indicate low ovarian reserve. However, this type of dynamic test is not widely used at present, as it is more invasive and more susceptible to adverse effects due to the need to administer a drug.
Ovarian reserve and fertility
One of the main causes of female infertility is age, since ovarian reserve decreases as a woman's age increases, especially after 35-40 years of age.
However, it is possible for a young woman to have a low ovarian reserve. For this reason, it is important for a woman to undergo a study to know her ovarian reserve when she is still young and even if she is not seeking motherhood at that time.
Thus, knowing the status of her ovarian reserve can help a woman make reproductive decisions to avoid possible complications. Thus, a young woman with a low reserve may opt for early pursuit of pregnancy or fertility preservation. This technique will allow the woman to try to achieve pregnancy when she wishes to do so in the future, with her own eggs, through assisted reproduction.
If you are interested in learning more about fertility preservation, you can read on in this article: Fertility preservation in young women
Ovarian reserve and assisted reproduction
When a woman attends an assisted reproduction clinic, the fertility study will include the assessment of ovarian reserve.
Knowing the patient's ovarian reserve is not only important to be able to indicate the best fertility treatment, but also because it can help to make a prognosis of the probabilities of success.
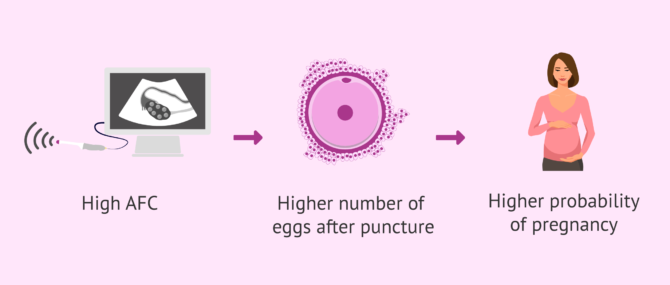
Currently, the most commonly used markers in assisted reproduction to evaluate a woman's ovarian reserve are the AFC and the determination of AMH.
For example, if the AFC is good, it can be estimated that a good number of oocytes will be obtained in the follicular puncture of an in vitro fertilization (IVF) treatment. This will increase the chances of obtaining a viable embryo that will result in pregnancy.
However, it must be taken into account that not only the quantity but also the quality of the oocytes obtained is important. When the ovarian reserve test shows a very low quantity of eggs, associated with a decrease in quality, for example, due to advanced maternal age, it may be advisable to resort to egg donation to achieve pregnancy.
In this link, you can find detailed information about this technique: What is ovodonation, and what is the price of the treatment?
What is the price of ovarian reserve analysis?
The cost of a female fertility study is around $250 - $500, depending on the tests included.
In the most basic studies, a transvaginal ultrasound is performed (to assess the ovarian reserve and observe the uterus) and a hormone analysis (to assess the functioning of the ovary and possible imbalances in the menstrual cycle). On the other hand, the most complete fertility studies also include the determination of anti-Müllerian hormone.
However, AMH analysis can be performed as a separate test. Its price will depend on the clinic or laboratory where it is performed, but usually ranges between $80 - $120.
Video on the different ovarian reserve tests
Michelle Lorraine Embleton, biochemist at inviTRA, talks to us in this video about the different studies to assess a woman's ovarian reserve:
FAQs from users
Is it possible to have a high AMH and a low AFC?
In principle, this would not be possible. Nevertheless, it can happen and you should be guided by what is visualized in the ultrasound to determine the state of the ovarian reserve.
Read more
Is there a relation between ovarian reserve and egg quality?
Ovarian reserve is a measure of the quantity and quality of the eggs; it is best measured by a combination of chronological age, antral follicle count (AFR) on ultrasound, and anti-mullerian hormone (AMH).
An AFR of less than 11 reflects diminished ovarian reserve and less than 6 is severe. AMH levels below 1.6 have been shown to reduce the number of eggs retrieved with IVF and may predict pregnancy outcome. Levels below 0.4 are severe.
Read more
How is the study of ovarian reserve performed?
Through a blood test where the value of the antimullerian hormone (AMH) is determined together with an ultrasound control to assess the number of antral follicles, it is possible to study the ovarian reserve activity of the woman at a given time.
Read more
Is anti-Müllerian hormone (AMH) or antral follicle count (AFC) more reliable for assessing ovarian reserve?
There is no one test to assess ovarian reserve better than another, there are several methods. In addition, there are no tests to predict the pregnancy rate as such.
Read more
Is there a relationship between antimüllerian hormone and antral follicle count?
Yes, the truth is that nowadays, the antimullerian test and the antral follicle count are the most widely used and most reliable tests of ovarian reserve. There is a good correlation between them.
Can I become a mother with low ovarian reserve?
Yes, it may be difficult to achieve a natural pregnancy, but assisted reproduction offers several solutions. Among them, we find in vitro fertilization with a previous cycle of ovarian stimulation.
On the other hand, in the most serious cases in which the ovarian reserve is very low, egg donation is perhaps the most appropriate reproductive solution.
Is artificial insemination recommended if my ovarian reserve is low?
Artificial insemination is generally not recommended when a woman has a low number of eggs, as the chances of success are low. It is usual to perform an IVF, although it will depend on the results obtained in the evaluation of the ovarian reserve of each case.
Recommended reading
If you would like to know more about other hormones related to female fertility and their normal values, we recommend reading article: Hormone analysis in women: what are the normal levels?
As we have seen, the ovarian reserve test is one of the main tests to analyze a woman's fertility. However, there are other tests that can complement the study. Do you want to know what they are? Find out here: What are fertility tests for women and what do they consist of?
Finally, the following article contains more information about ovarian reserve and its influence on fertility: What is an ovarian reserve and how does it affect fertility?
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Bedenk J, Vrtačnik-Bokal E, Virant-Klun I. The role of anti-Müllerian hormone (AMH) in ovarian disease and infertility. J Assist Reprod Genet. 2020 Jan;37(1):89-100. (view)
Bhide P, Pundir J, Homburg R, Acharya G. Biomarkers of ovarian reserve in childhood and adolescence: A systematic review. Acta Obstet Gynecol Scand. 2019 May;98(5):563-572. (view)
Iliodromiti S, Nelson SM. Biomarkers of ovarian reserve. Biomark Med. 2013 Feb;7(1):147-58. (view)
La Marca A, Sunkara SK. Individualization of controlled ovarian stimulation in IVF using ovarian reserve markers: from theory to practice. Hum Reprod Update. 2014 Jan-Feb;20(1):124-40. (view)
Moolhuijsen LME, Visser JA. Anti-Müllerian Hormone and Ovarian Reserve: Update on Assessing Ovarian Function. J Clin Endocrinol Metab. 2020 Nov 1;105(11):3361–73. (view)
Steiner AZ. Biomarkers of ovarian reserve as predictors of reproductive potential. Semin Reprod Med. 2013 Nov;31(6):437-42. (view)
Tal R, Seifer DB. Ovarian reserve testing: a user's guide. Am J Obstet Gynecol. 2017 Aug;217(2):129-140. (view)
Wen J, Huang K, Du X, Zhang H, Ding T, Zhang C, Ma W, Zhong Y, Qu W, Liu Y, Li Z, Deng S, Luo A, Jin Y, Zhang J, Wang S. Can Inhibin B Reflect Ovarian Reserve of Healthy Reproductive Age Women Effectively? Front Endocrinol (Lausanne). 2021 Apr 14;12:626534. (view)
FAQs from users: 'Is it possible to have a high AMH and a low AFC?', 'Is there a relation between ovarian reserve and egg quality?', 'How is the study of ovarian reserve performed?', 'What do I have to do to know my ovarian reserve?', 'Is anti-Müllerian hormone (AMH) or antral follicle count (AFC) more reliable for assessing ovarian reserve?', 'Is there a relationship between antimüllerian hormone and antral follicle count?', 'Can I become a mother with low ovarian reserve?' and 'Is artificial insemination recommended if my ovarian reserve is low?'.
Authors and contributors


More information about Michelle Lorraine Embleton








is it possible to improve ones low egg count?
Hello Cynthia,
At the moment of embryonic development, when the future woman is only a fetus in her mother’s womb, the formation of oocytes begins. This period ends before the birth of the woman, and as far as it is known today, it is not possible to prolong it. This means that the woman is born with a certain number of oocytes (millions of them.
When she reaches puberty, regular ovulations begin. Similar as happens with sperm, only one egg is good enough to be fertilized in the fallopian tube, that means the rest of the eggs on their way to the tube will irrevocably be lost. Shortly said, with every ovulation until menopause, a woman loses eggs compromising her ovarian reserve which can consequently not be improved.
So in order to get pregnant with an already low egg count, the patient would need to opt for a fertility treatment.
Hope I could solve your question,
Best regards
Hello
I’m 36 years old, I’ve been trying for a baby for two years. I’ve had my hormone tests done and they didn’t come back very hopeful.
AMH : 0.3 ng/ml
FSH : 4.56
LH: 3’83
Oestradiol: 102.2
I’d like you to tell me if there’ s a chance of success with these results.
Thank you in advance.
Hi Cindy,
The antimullerian hormone (AMH) score is low, indicating a low ovarian reserve. However, you can achieve a pregnancy with IVF treatment.
The pregnancy rate of an IVF-ICSI in women of 39 years is about 26%.
If you are not successful, you will have to resort to egg donation in order to become a mother. I leave you the following article that may be of interest to you: IVF treatment with egg donation.
I also recommend you to have a look at this tool: Fertility Report. In this way, we can recommend the clinics that best suit you. In addition, we will also give you some advice about when it is time to visit the clinics.
I hope I have helped you.