The Antimüllerian hormone (AMH) is a marker used to evaluate a woman's ovarian reserve and thus assess her fertility status at a specific moment.
High AMH values indicate that the ovarian reserve is optimal. However, as the age of the woman increases, these values decrease until ovarian depletion occurs.
The analysis of the AMH levels also provides information on the most appropriate assisted reproduction treatment to achieve a pregnancy: artificial insemination (AI), in vitro fertilization (IVF) or the need to resort to egg donation.
Provided below is an index with the 9 points we are going to expand on in this article.
- 1.
- 2.
- 2.1.
- 2.2.
- 2.3.
- 2.4.
- 3.
- 4.
- 5.
- 6.
- 6.1.
- 6.2.
- 6.3.
- 6.4.
- 6.5.
- 6.6.
- 6.7.
- 7.
- 8.
- 9.
What is the Anti-müllerian hormone?
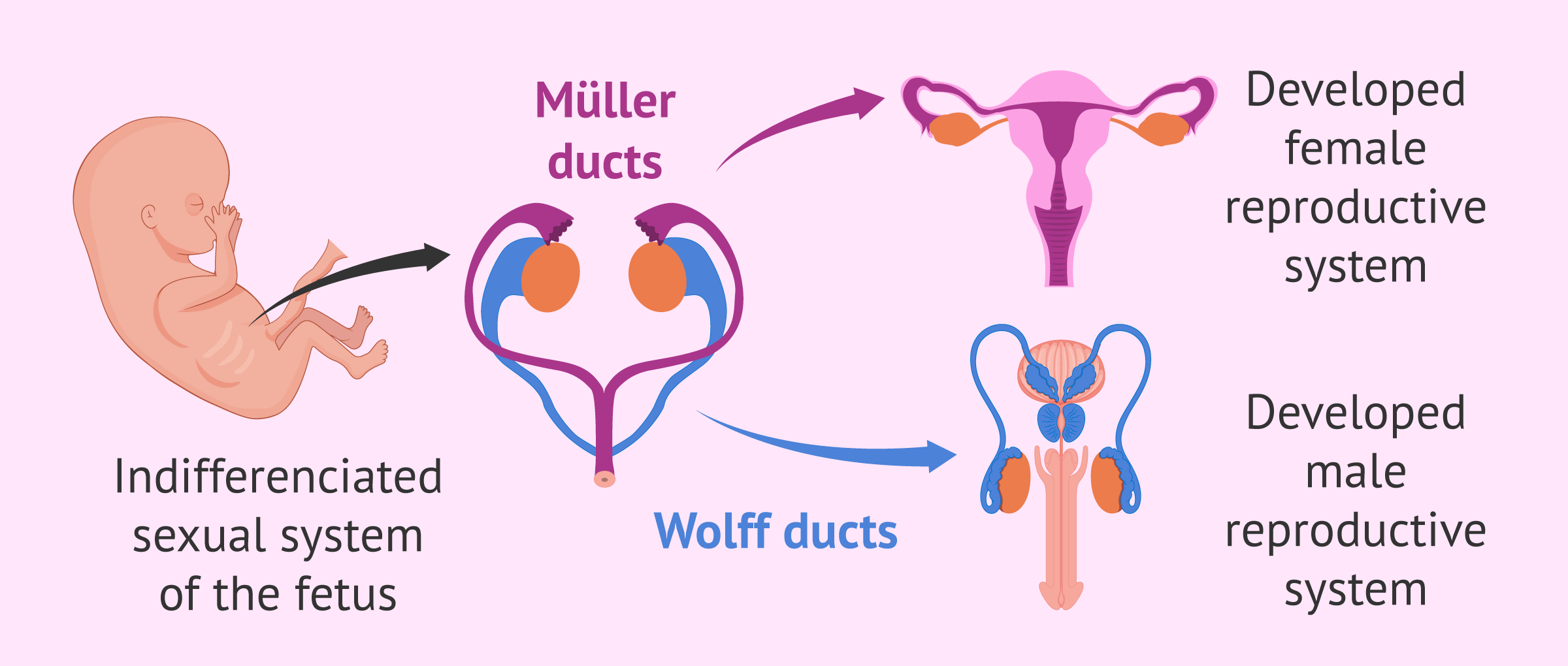
AMH is a protein present in both men and women, but with different functions and locations. Its main role occurs during pregnancy, as it is responsible for the sexual differentiation of the fetus.
In the following section, we will explain the mechanism of action of AMH in relation to the sex of the fetus:
- Male sex
- AMH is produced by the testes around weeks 8 and 9 of fetal development in order to prevent the development of the Müllerian ducts, structures that lead to the uterus and Fallopian tubes.
- Female sex
- the absence of AMH allows the female reproductive system to form in the fetus. However, AMH will begin to be expressed a few weeks later, when ovarian follicles are already present.
After birth, AMH levels remain high in males until adolescence, but in adulthood, they are low.
In women, however, the Anti-Müllerian hormone begins to become important from puberty onwards, as it is produced by the ovarian follicles where the eggs develop.
AMH in women
Anti-müllerian hormone is produced by the preantral and antral follicles of the ovaries throughout a woman's reproductive life, i.e. from puberty to menopause.
Specifically, it is the granulosa cells that surround the egg that is responsible for synthesizing it. Therefore, the measurement of the AMH in the blood indicates approximately the number of eggs a woman has, i.e. her ovarian reserve.
AMH is present in all follicles of both ovaries equally and is, therefore, a biological marker of fertility.
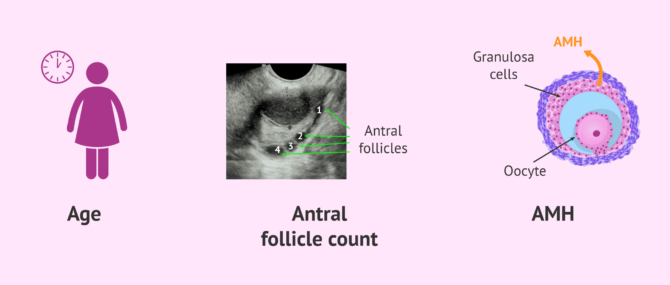
To evaluate female fertility, other analyses will also be taken into account: FSH and LH hormone values, antral follicle count by transvaginal ultrasound, etc.
Find more information about this topic here: What Can Ovarian Reserve & AMH Tests Tell Us?
When to perform an analysis?
As we have said, the antimüllerian hormone is synthesized by the antral and preantral follicles of the ovary. These are growing basal follicles, which have not yet been selected to mature into dominant follicles.
The importance of this is that AMH values do not vary with the menstrual cycle. The blood test can, therefore, be done on any day of the cycle without influencing the results. It is also not necessary to fast before the test.
However, it should be borne in mind that this hormones is usually studied in conjunction with other female hormones when assessing fertility, such as FSH and estradiol, especially before undergoing assisted reproduction treatment.
For all this, it is more practical to perform a single hormonal blood test in the basal state, which are the first days of the cycle: 3-5 days after the start of menstruation.
AMH values
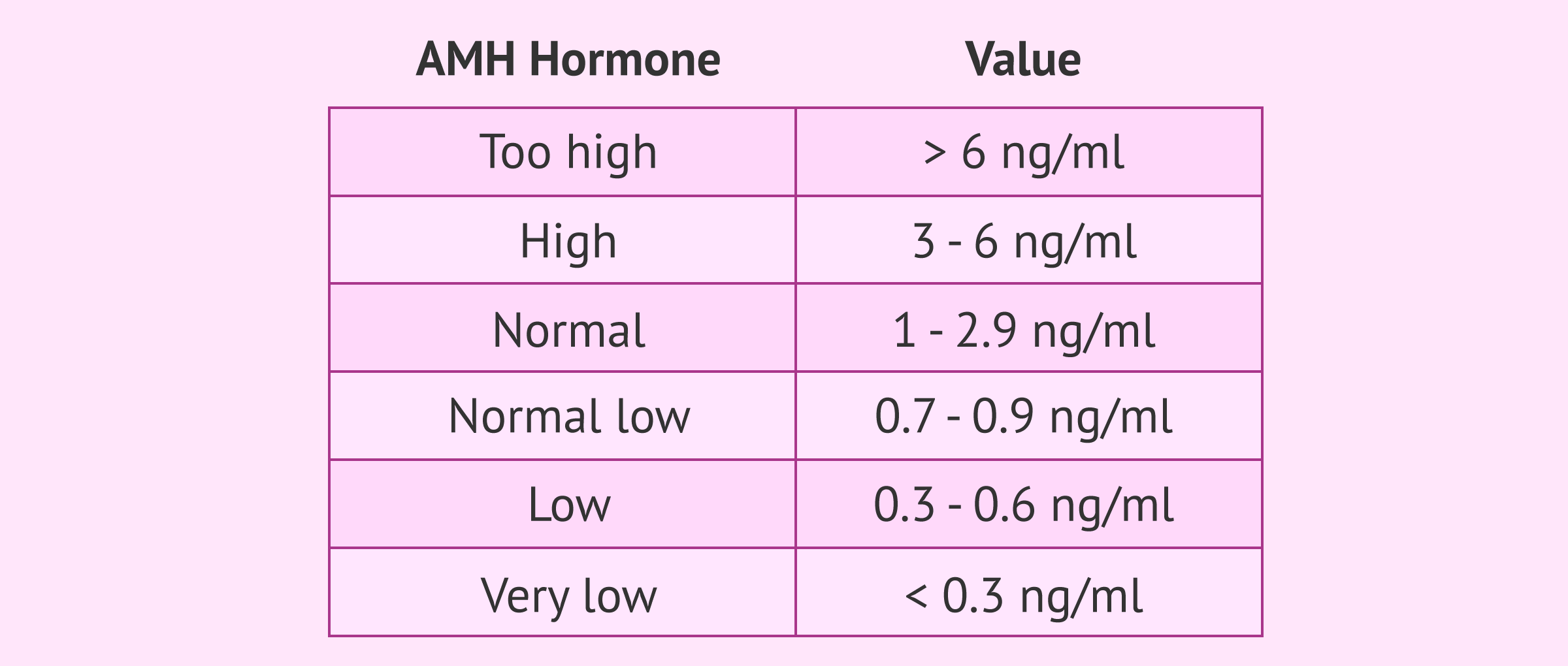
The AMH reference values are well defined and allow us to know more or less what the woman's fertility status is at the time of the analysis.
However, since there are several methods for detecting AMH, it is difficult to compare the levels obtained between different techniques. It is best to interpret each patient's results according to the cut-off values of each test.
We will now establish the reference ranges of the technique most commonly used in laboratories, although there may be slight differences.
- Very high AMH
- niveles mayores de 6 ng/ml. They indicate that there may be a risk of ovarian hyperstimulation syndrome when administering hormonal medication in an IVF.
- High AMH
- between 3 and 6 ng/ml. The ovarian reserve is good.
- Normal AMH
- between 1 and 2,9 ng/ml. The ovarian reserve is good.
- Normal low AMH
- between 0,7 and 0,9 ng/ml. The ovarian reserve has begun to decrease, although it is still within normal range
- Low AMH
- between 0,3 and 0,6 ng/ml. Suggest a low ovarian reserve and, as a consequence, the patient is likely to have a low response to hormone stimulation.
- Very low AMH
- levels lower than 0.3 ng/ml The ovarian reserve is almost exhausted and the woman is close to menopause. Egg donation is most likely needed to have children.
In other hormone analyses, it is possible to find the AMH values in the units of pmol/l.
Finally, it is worth mentioning that women with polycystic ovaries have the highest antimullerian hormone and that it decreases more slowly with increasing age. This implies that these women have more delayed ovarian aging.
Anti-Mullerian Hormone by Age
As a woman's age increases, her ovarian reserve decreases and, consequently, so does her AMH level.
The most drastic drop takes place from the age of 36, but there are some women who have a low reserve even earlier. This would be the case with early menopause.
Knowing the state of fertility and the ovarian reserve can help women to better plan their motherhood and make decisions like the following:
- Preservation of fertility if she wants to become a mother in the future, i.e. freezing the eggs for later use.
- Bringing motherhood forward to the near future in the case of a normal-low reserve.
- Undergoing an assisted reproduction treatment if AMH has resulted in a low value.
Since the analysis of the anti-Müllerian hormone can be expensive, it is also possible to assess the ovarian reserve with an ultrasound and the FSH level.
The value of AMH is directly proportional to the number of antral follicles in the ovary and, therefore, to the ovarian reserve.
In contrast, FSH values vary in reverse: the lower the ovarian reserve, the higher the FSH hormone.
AMH and assisted reproduction
Another of the advantages of this hormonal determination is that it is very useful for assisted reproduction professionals, as they can decide which treatment is most suitable for each patient, as well as the pattern of hormonal medication required.
It has been shown that there is a correlation between the values of AMH and the degree of ovarian response to ovarian stimulation. Thus, patients with high AMH may be at risk of hyperstimulation, while patients with low AMH are more likely to have a low response.
The latter, therefore, will need higher doses of gonadotropins to achieve multiple follicular development.
AMH can be useful to better predict the success of assisted reproduction treatments and to be able to make a more accurate indication of the appropriate technique for each patient.
In addition to all this, the anti-Mullerian hormone also allows a better study of fertility physiology, since its levels have also been related to the quality of the eggs. It is said that only healthy follicles, which will give rise to a high-quality oocyte, are capable of producing AMH.
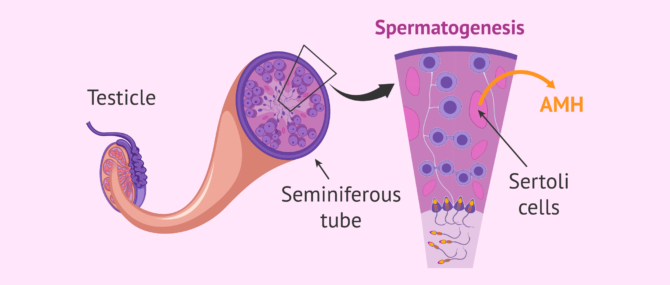
AMH in men
Although this test is not as widely used in men, AMH is a good marker of testicular function.
In particular, AMH is synthesized in Sertoli cells, where sperm formation (spermatogenesis) also occurs.
Analysis of AMH in men can be performed at diagnosis of azoospermia (absence of sperm in the ejaculate). In this case, AMH helps to determine whether or not there are sperm in the testicle.
These could be removed by biopsy and used in an intracytoplasmic sperm injection (ICSI) to fertilize the woman's eggs.
However, AMH in men is a predictor that is not as effective as in women and, ultimately, better results are obtained through FSH analysis.
AMH test costs
The determination of AMH in blood is a test that can be performed within the female fertility testing or separately. Prices can vary greatly depending on the clinic and laboratory where it is done.
In assisted reproduction, like any medical treatment, it is necessary for you to trust the professionalism of the doctors and the clinic you choose.
This Tool generates you a personalized report with all information necessary about the treatment you will need. Besides, there is a list of clinics in your area which we have chosen based on our selection criteria with their budget plan included. Last but not least, you will find a series of useful tips for your first clinic visit.
In general, female fertility studies cost $150-$500 and include pelvic ultrasound. Apart from this, fertility-related blood tests are charged between $200-$400 and the most expensive ones include AMH testing.
If only the AMH test is performed, the price is about $100.
Video on anti-Müllerian hormone
Michelle Emblenton, biochemist at inviTRA, talks to us in this video about anti-Müllerian hormone:
Anti-mullerian hormone or AMH is a protein that is present in both men and women, although it plays different roles in different locations.
FAQs from users
Can AMH values increase from one test to the next?
Antimullerian hormone (AMH) is a hormone whose value can be determined in a blood test to assess a woman's ovarian reserve. This hormone is produced by the antral follicles, so it is proportional to the antral follicle count and the number of eggs that can be obtained in an ovarian stimulation.
In general, AMH is considered to be the most reliable parameter for assessing ovarian reserve. However, sometimes we find that the values differ from one retrieval to another, and we can even find increases in its value over time. This increase is not related to an increase in ovarian reserve, as this decreases over time.
AMH can be highly variable due to factors such as seasonal changes, timing of the cycle, smoking or certain diseases. A study that assessed the variability of AMH on different days of the cycle found an average variation of up to 20%, being higher in women with low AMH levels.
Therefore, the information given by AMH should always be contrasted with an ultrasound of antral follicle count, and caution should be exercised when interpreting a single AMH determination, especially in the case of women with low ovarian reserve.
I am 23 years old and my antimullerian hormone value is 1.2 ng/mL. Do I have good ovarian reserve?
Antimullerian hormone is only one of several factors used to measure ovarian reserve. We will have to take into account age, ultrasound (antral follicle count) and AMH (antimullerian hormone) along with other hormones that also guide us (FSH, LH estradiol). Therefore, the value of antimullerian hormone alone is not sufficient to define the ovarian reserve of a patient.
Between 1.2ng/mL and 3 ng/mL is considered a normal AMH. However, it is somewhat low for 23 years. For this reason, I would recommend you to extend the study and, if in doubt, to vitrify oocytes (freeze eggs) if you wish to postpone your maternity, in case the hormone value decreases later on.
At what age should AMH be examined?
Anti-Müllerian hormone is produced by the ovary, and its blood levels are an indicator of a woman's ovarian reserve.
To ensure everything works as expected, we recommend that the first measurement is done from age 20 and not later than age 30. By doing this, if a woman has a diminished ovarian reserve at a young age, she would have time to decide whether she wants to have a baby now or cryopreserve some eggs to become a mother in the future.
What information does the Anti-Müllerian hormone analysis provide?
Anti-Müllerian hormone is produced by the preantral and antral follicles of the ovaries throughout a woman's reproductive life.
Specifically, responsible for synthesizing it are the granulosa cells that surround the egg. The measurement of AMH in blood indicates approximately the quantity or number of eggs a woman has, i.e. her ovarian reserve. To complete the information on the ovarian reserve it is necessary to perform a transvaginal ultrasound with an antral follicle count.
It is important to remember that both the AMH and the antral follicle count are quantitative markers and do not provide us with information about egg quality. The parameter that best correlates with the quality of the oocytes is the woman's age.
Can I get pregnant naturally with a low AMH level?
Low AMH values are an indication of a low ovarian reserve. However, it is only reported that the chances of pregnancy are reduced, not impossible. It depends on the exact value obtained and other factors such as the quality of the partner's semen, the permeability of the fallopian tubes, endometrial receptivity, etc.
Why can't I get pregnant even though my AMH level is high?
A high AMH level indicates that the egg reserve is good. However, there may be other changes that affect your fertility. In these cases, it is best to have a full fertility check-up to analyze which factors can prevent you from getting pregnant.
Can you improve low AMH levels?
Basically not. AMH is an indirect measure of the number of eggs in a woman's ovarian reserve and there is no treatment to increase egg production. However, some women experience a slight improvement in their AMH levels by living a healthier lifestyle.

Quitting smoking, eating a healthy diet or losing weight are habits that can improve the quality of the eggs, which could be reflected in the AMH level.
Recommended reading
To learn more about the ovarian reserve, we recommend that you read on here: What is the Ovarian Reserve and How Does It Affect Fertility?
To read more about the AMH test and other important examinations, you can read the following article: Can a Women's Egg Count be Measured with a Blood Test?
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
A La Marca, G Sighinolfi, D Radi, C Argento, E Baraldi, A Carducci Artenisio, G Stabile, A Volpe. Anti-Mullerian hormone (AMH) as a predictive marker in assisted reproductive technology (ART). Hum Reprod Update. Mar-Apr 2010;16(2):113-30. doi: 10.1093/humupd/dmp036 (View)
G Ozzola. Anti-Müllerian hormone: A brief review of the literature. Clin Ter. Jan-Feb 2017;168(1):e14-e22. doi: 10.7417/CT.2017.1976 (View)
Hui-Yu Xu, Hong-Xian Zhang, Zhen Xiao, Jie Qiao, Rong Li. Regulation of anti-Müllerian hormone (AMH) in males and the associations of serum AMH with the disorders of male fertility. Asian J Androl. Mar-Apr 2019;21(2):109-114. doi: 10.4103/aja.aja_83_18 (View)
Jure Bedenk, Eda Vrtačnik-Bokal, Irma Virant-Klun. The role of anti-Müllerian hormone (AMH) in ovarian disease and infertility. J Assist Reprod Genet. 2020 Jan;37(1):89-100. doi: 10.1007/s10815-019-01622-7 (View)
Leah Hawkins Bressler, Anne Steiner. Anti-Müllerian hormone as a predictor of reproductive potential. Curr Opin Endocrinol Diabetes Obes. 2018 Dec;25(6):385-390 (View)
Loes M E Moolhuijsen, Jenny A Visser. Anti-Müllerian Hormone and Ovarian Reserve: Update on Assessing Ovarian Function. J Clin Endocrinol Metab. 2020 Nov 1;105(11):3361-3373. doi: 10.1210/clinem/dgaa513 (View)
Mathilde Victoria, Julie Labrosse, Fabien Krief, Isabelle Cédrin-Durnerin, Marjorie Comtet, Michaël Grynberg. Anti Müllerian Hormone: More than a biomarker of female reproductive function. J Gynecol Obstet Hum Reprod. 2019 Jan;48(1):19-24. doi: 10.1016/j.jogoh.2018.10.015 (View)
Zehra Jamil, Syeda Sadia Fatima, Khalid Ahmed, Rabia Malik. Anti-Mullerian Hormone: Above and Beyond Conventional Ovarian Reserve Markers. Dis Markers. 2016;2016:5246217. doi: 10.1155/2016/5246217 (View)
FAQs from users: 'Can AMH values increase from one test to the next?', 'I am 23 years old and my antimullerian hormone value is 1.2 ng/mL. Do I have good ovarian reserve?', 'At what age should AMH be examined?', 'What information does the Anti-Müllerian hormone analysis provide?', 'Can I get pregnant naturally with a low AMH level?', 'What is anti-mullerian hormone (AMH)?', 'Why can't I get pregnant even though my AMH level is high?', 'Why measure anti-mullerian (AMH) levels in women?', 'Can you improve low AMH levels?', 'What do male anti-mullerian (AMH) levels indicate?', 'How much do anti-mullerian (AMH) tests cost?', 'At what age should I get my anti-mullerian (AMH) levels tested?' and 'My anti-mullerian (AMH) is high, why can't I get pregnant?'.
Authors and contributors




More information about Michelle Lorraine Embleton





Good afternoon. The AMH results show 3.9. But I want to know if with this result there’s any likelihood that I’ll have anovulation?
Last week I took the test to measure my anti-Mullerian hormone, I was 5 days past my period and the result was 0.999. I am 30 years old and I was not thinking about having children at the moment. I wanted to know if this result is very serious since I have to take vissane to be able to control my endometriosis issue.
Would visanne affect the result of my anti-bullet hormone more?
Thank you for your answer.
Hello, I’m very confused. I was given a value of 3.65 ng/ml today. Is it possible to get pregnant naturally like this? I haven’t taken anticonceptives for over a year and I don’t know anymore.
Hi, I’d like to check on my ovarian reserve. I had the AMH test done and I got 5.80 ug/ml, but I don’t understand if it’s good or not.
Hi!
I got myself tested and my AMHlevel is ng/ml 1.12. I’m 29. Is this a good value or not?