Gonadotropins, also known as gonadotrophins, are a group of hormones consisting of luteinizing hormone (LH), follicle stimulating hormone (FSH) and chorionic gonadotropin (hCG).
Both men and women produce gonadotropins and, in both cases, they are responsible for regulating processes related to reproduction. Because of this, gonadotropins are administered in assisted reproduction treatments to control ovarian follicular development and ovulation in women, thus improving the chances of success of these treatments.
Provided below is an index with the 6 points we are going to expand on in this article.
- 1.
- 1.1.
- 2.
- 2.1.
- 2.2.
- 2.3.
- 3.
- 3.1.
- 3.2.
- 3.3.
- 3.4.
- 3.5.
- 4.
- 5.
- 6.
What are gonadotropins?
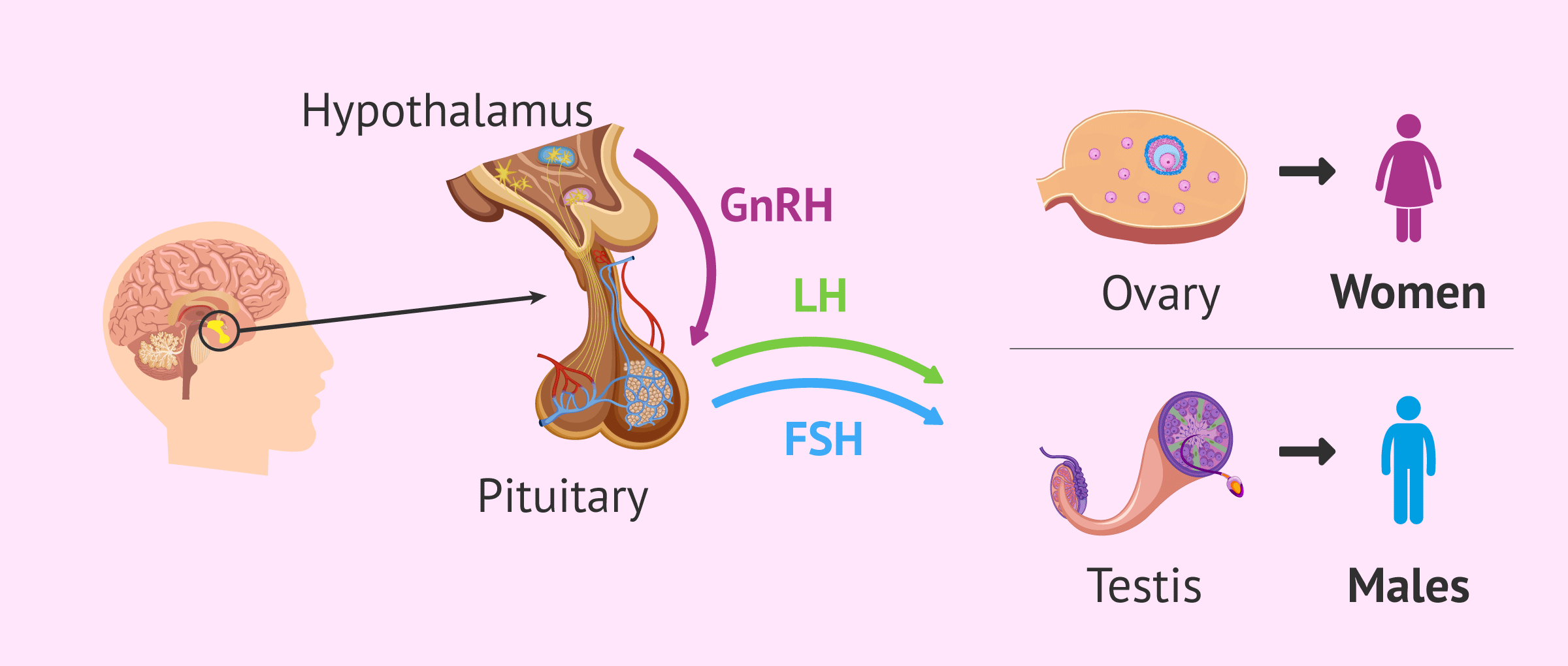
Gonadotropins are hormones that will exert their main function in the gonads, that is, in the ovaries and testes. Therefore, gonadotropins are important for the regulation and proper functioning of processes related to female and male reproduction.
In terms of their structure, gonadotropins are glycoproteins consisting of two subunits: alpha and beta. The alpha subunit is common to all types of gonadotropins (FSH, LH, and hCG); whereas the beta subunit is specific for each of them.
Where are they produced?
FSH and LH are synthesized in the pituitary gland in response to gonadotropin-releasing hormone or GnRH. GnRH is produced in the hypothalamus in a pulsatile manner and stimulates the release of the gonadotropins FSH and LH by the pituitary gland. For this reason, the hormonal regulation of reproductive processes is carried out by the so-called hypothalamus-pituitary-gonad axis.
For its part, hCG is known to be the "pregnancy hormone" because it is produced by the embryo.
Types of gonadotropins
There are several hormones that fall under the term gonadotropins. Each of them is described below.
FSH
Follicle-stimulating hormone is named for the function it exerts in women by stimulating the growth of ovarian follicles. However, FSH has other important functions in women such as the production of estrogens from androgens in ovarian granulosa cells.
This hormone allows the development of a follicular cohort, of which only one follicle will give rise to a mature egg in each menstrual cycle. Selection occurs because, approximately 5-7 days after the onset of the menstrual cycle, a drop in FSH levels occurs. This means that only the dominant follicle can continue to develop, while the rest of the follicles degenerate.
In the male, FSH regulates spermatogenesis through its action on Sertoli cells.
On the other hand, FSH is administered during the controlled stimulation of assisted reproduction treatments in order to increase the number of follicles that will reach full maturation.
Assisted procreation, as any other medical treatment, requires that you rely on the professionalism of the doctors and staff of the clinic you choose. Obviously, each clinic is different. Get now your Fertility Report, which will select several clinics for you out of the pool of clinics that meet our strict quality criteria. Moreover, it will offer you a comparison between the fees and conditions each clinic offers in order for you to make a well informed choice.
You can learn more about the FSH hormone in this article: FSH hormone: what are its functions and normal values?
LH
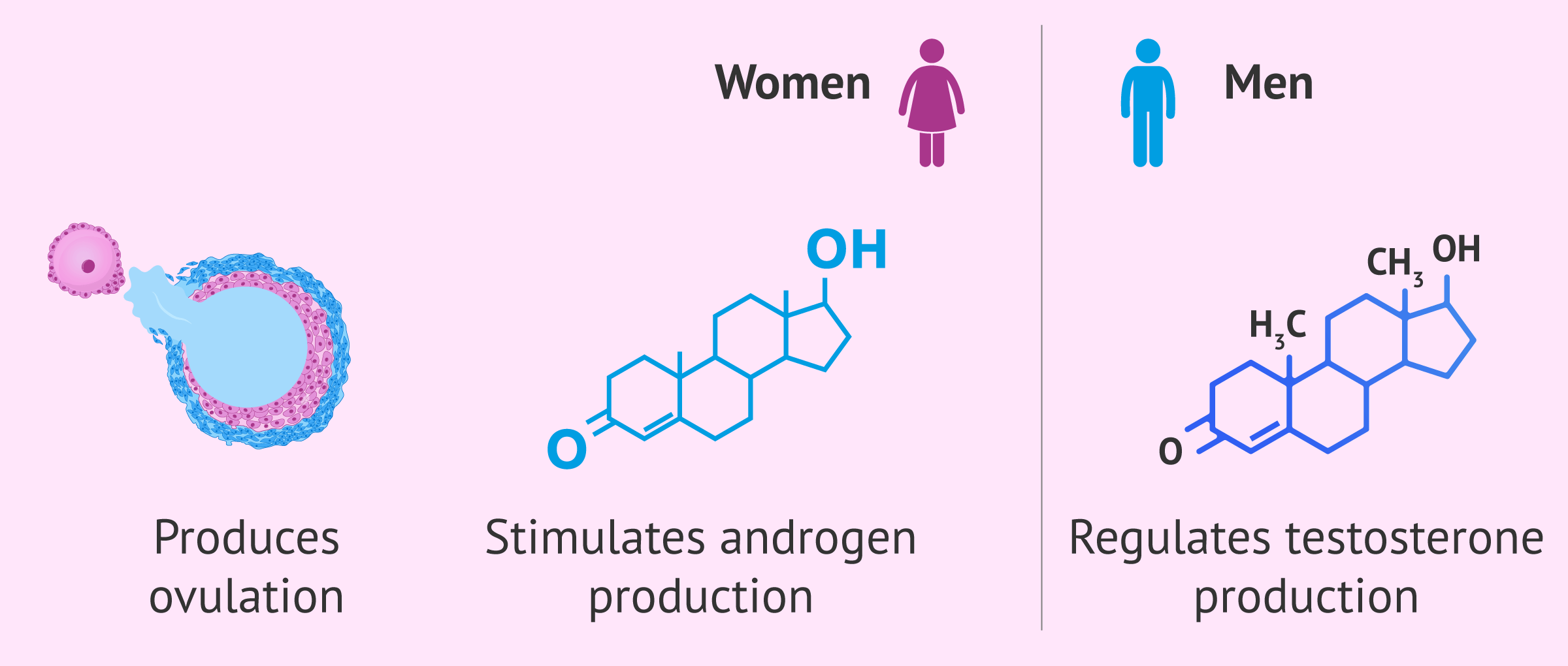
Luteinizing hormone is responsible for producing ovulation in women. In response to the estrogen surge produced by the dominant follicle, a spike in LH levels occurs midway through the menstrual cycle that triggers the final maturation of the egg and its release into the fallopian tubes by ovulation.
After ovulation, luteinization of the follicle occurs in the ovary. This process leads to the appearance of the corpus luteum, which will begin to secrete progesterone to prepare the endometrium for possible embryo implantation.
On the other hand, LH also has the function of stimulating androgen production in ovarian theca cells. These androgens may be converted to estrogens in the granulosa cells. Both types of cells (theca and granulosa) are found surrounding the egg and are part of the ovarian follicles.
In the male, LH will act on the Leydig cells to regulate testosterone production.
If you want to continue reading about the LH hormone, you can click here: LH hormone: what are its functions in the reproductive cycle?
hCG
HCG is a gonadotropin that is initially produced by the embryo and has a fundamental role in pregnancy, as it acts on the corpus luteum for the production of progesterone. However, hCG is well known for its use in pregnancy tests. In addition, this hormone is also widely used in assisted reproduction techniques.
HCG levels increase rapidly in gestation. Because of this, pregnancy tests performed on urine or blood are based on detecting the hCG hormone. However, there is an important difference between the two tests: urine tests are qualitative tests (they determine the presence or absence of the hormone), while blood tests are generally quantitative and indicate the amount of hCG hormone present. In addition, blood tests are more sensitive, i.e., they can detect a lower amount of hCG.
On the other hand, the hCG concentration varies throughout pregnancy and can provide information about the weeks of gestation or about the existence of a problem in the pregnancy if hCG levels do not vary at the expected rate. Typically, hCG values usually double every 48-72 hours during the first 12 weeks of gestation.
For assisted reproduction treatments, the hCG hormone is administered prior to ovarian puncture to trigger ovulation. This is due to its structural and biological similarity to LH. In addition, hCG can be used for luteal phase support. However, in this case, it is more common to use progesterone, as this avoids the inconvenience of the risk of ovarian hyperstimulation syndrome (OHSS) related to hCG.
You can continue reading more in-depth about hCG at this link: The hCG hormone (Human Chorionic Gonadotropin)
FAQs from users
What are the advantages of using gonadotropins over clomiphene in assisted reproduction?
The use of gonadotropins in ovarian stimulation allows a better dose adjustment than clomiphene citrate. In addition, a higher gestation rate is achieved since it does not have an anti-estrogenic effect on the endometrium.
On the other hand, the side effects of gonadotropins are minimal and there is no limit to the number of cycles to be performed.
Read more
What are the most commonly used gonadotropins in assisted reproduction?
Gonadotropins are the hormones that are secreted by the pituitary under natural conditions for the regulation of the reproductive system.
In assisted reproduction treatments we use them for controlled ovarian stimulation. There are 5 types of gonadotropins according to their origin:
- Human menopausal gonadotropins (HMG).
- Highly purified human menopausal gonadotropins.
- Highly purified urinary gonadotropins.
- Recombinant gonadotropins alone or in combination.
- Recombinant long-acting gonadotropins.
The ones that are used more frequently are the recombinant ones and also the human menopausal ones. The choice of type and dose of gonadotropins will depend on the clinical history of each patient, their age and ovarian reserve.
When are gonadotropins administered?
Gonadotropins are hormones that are used primarily to stimulate the ovaries, and eventually to stimulate sperm production in males.
In women who need to undergo assisted reproduction treatment to become pregnant, either artificial insemination or in vitro fertilization, gonadotropins are needed to stimulate the growth of eggs.
Gonadotropins are hormones that are administered by subcutaneous injections and are administered by the patient herself with the help of very easy-to-use devices. Depending on the treatment and the particular case, the physician will choose the appropriate doses of gonadotropins.
The side effects of these hormones are usually emotional lability and mood swings, headache and in the last days of the treatments abdominal distension and menstrual-like sensations.
It is very important to use gonadotropins only under medical prescription, with ultrasound controls to evaluate the response of follicles in the ovaries and to indicate the days to be administered and the dose.
When should gonadotropin blood levels be measured?
Because gonadotropin levels vary throughout the menstrual cycle, it is most usual to test gonadotropin levels at basal conditions, i.e. in the first days of the menstrual cycle (day 1-4 of the cycle).
Why are gonadotropins used for ovarian stimulation in assisted reproduction techniques?
Gonadotropins are used for ovarian stimulation in assisted reproduction because they are essential hormones in the regulation of the woman's natural menstrual cycle.
Because of this, administering gonadotropins exogenously to the patient will allow the specialist to better control the cycle, the maturation of a greater number of follicles and to determine the moment when ovulation will occur. All this contributes to increase the probability of success of assisted reproduction treatments.
Recommended readings
If you are interested in the subject, we recommend you to read the following article on GnRH: What is GnRH - Characteristics, effects, and medications.
If, on the other hand, you wish to obtain more information on ovarian stimulation for assisted reproduction treatments, you can visit the following link: What is ovarian stimulation - Process, medications, and symptoms
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Choi J, Smitz J. Luteinizing hormone and human chorionic gonadotropin: origins of difference. Mol Cell Endocrinol. 2014 Mar 5;383(1-2):203-13.
Herbison AE. The Gonadotropin-Releasing Hormone Pulse Generator. Endocrinology. 2018 Nov 1;159(11):3723-3736.
Montagnana M, Trenti T, Aloe R, Cervellin G, Lippi G. Human chorionic gonadotropin in pregnancy diagnostics. Clin Chim Acta. 2011 Aug 17;412(17-18):1515-20.
Stamatiades GA, Kaiser UB. Gonadotropin regulation by pulsatile GnRH: Signaling and gene expression. Mol Cell Endocrinol. 2018 Mar 5;463:131-141.
Szymańska K, Kałafut J, Rivero-Müller A. The gonadotropin system, lessons from animal models and clinical cases. Minerva Ginecol. 2018 Oct;70(5):561-587.
Theofanakis C, Drakakis P, Besharat A, Loutradis D. Human Chorionic Gonadotropin: The Pregnancy Hormone and More. Int J Mol Sci. 2017 May 14;18(5):1059.
FAQs from users: 'What are the advantages of using gonadotropins over clomiphene in assisted reproduction?', 'What are the most commonly used gonadotropins in assisted reproduction?', 'When are gonadotropins administered?', 'When should gonadotropin blood levels be measured?' and 'Why are gonadotropins used for ovarian stimulation in assisted reproduction techniques?'.
Authors and contributors
More information about Cristina Algarra Goosman







Is there a natural way to increase LH levels?
Hello Jennifer,
Generally, LH levels fluctuate throughout the menstrual cycle, it is usually measured on the third day of the period as this is the time in the cycle when it will give a truer value compared to baseline levels.
It is important that if any deficiency is identified it is treated. Naturally, it is not possible to increase this hormone specifically as both a low LH concentration and an excess of LH can be detrimental to fertility.
Drugs can be used to control the values and keep them within the recommended levels. Always being controlled and supervised by a professional.
I recommend you to read this article: What are the functions of the LH hormone in the reproductive cycle?
I hope I have helped you.
Best regards.
Hello, so these hormones are detected in blood and urine no?
Hello Noemish_,
Indeed, all these hormones have two ways to measure them, blood test and urine test.
The test performed by blood is more reliable as it can give a quantitative result and does not need to have a threshold to be detected.
It is more common to find pregnancy tests (which detect hCG) and ovulation tests (which detect LH) by urine. Keep in mind that with these tests it is important when they are performed as this will influence the result.
I hope I have helped you.
Best regards.