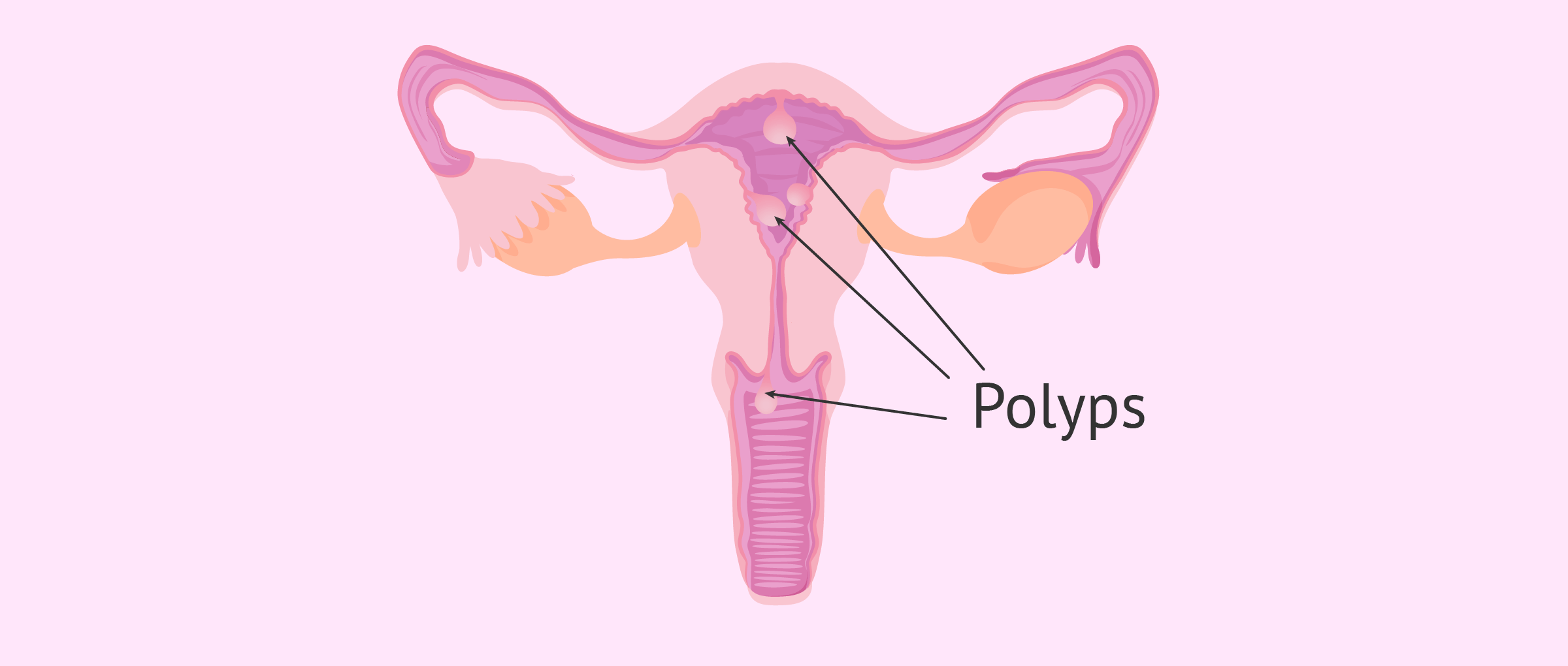
Uterine polyps, also called endometrial polyps, occur because a portion of the endometrial tissue protrudes into the uterine cavity endometrial polyps uterine polyps, occur because a portion of endometrial tissue protrudes into the uterine cavity. The most common symptom of a uterine polyp is bleeding, although sometimes they are asymptomatic.
Most endometrial polyps are benign, but some of them can cause cancer. In addition, polyps can also make it difficult to achieve pregnancy. Therefore, it is important to consult a gynecologist in the presence of any symptoms.
In terms of treatment, the most common option is the removal of the polyp by surgical hysteroscopy, since complications associated with this technique are not common.
Provided below is an index with the 10 points we are going to expand on in this article.
- 1.
- 1.1.
- 2.
- 3.
- 4.
- 5.
- 6.
- 6.1.
- 7.
- 7.1.
- 7.2.
- 7.3.
- 7.4.
- 7.5.
- 7.6.
- 7.7.
- 7.8.
- 8.
- 9.
- 10.
Definition of endometrial polyp
Endometrial polyps appear when an area of the basal layer of the endometrium, which is not changed by the hormones of the menstrual cycle and is not shed at each menstruation, proliferates.
The outer endometrial layer (the functional endometrium) is shed at each menstrual period. Thus, the endometrial basal layer with the polyp remains in the uterus and continues to grow and individualize.
Although several mechanisms have been proposed for the formation of polyps, the exact causes are not known. However, it is known that polyps tend to grow when blood estrogen levels are elevated.
Risk and protective factors
As mentioned above, the exact cause for the development of uterine polyps is not known. However, there are a number of factors that can increase the risk of having a uterine polyp. All of them are listed below:
- Elevated estrogen concentration.
- Chronic anovulation, that is, having menstrual cycles without ovulation.
- Luteal insufficiency or insufficient production of progesterone by the corpus luteum.
- Age of the woman, since there is a higher risk of developing endometrial polyps, especially between 40 and 65 years of age.
- Use of tamoxifen, a drug used in the treatment of breast cancer.
- Chronic uterine inflammation.
- Hormonal treatments in postmenopausal women.
- Obesity and arterial hypertension.
- Some rare genetic diseases, such as Lynch syndrome or Cowden syndrome.
It should be noted that the presence of any of the characteristics mentioned above does not imply that the woman will have endometrial polyps. It only means that the chances of developing a uterine polyp are higher compared to other women who do not have these factors.
On the other hand, there also appear to be a number of protective factors that may decrease the likelihood of polyps developing due to their anti-estrogenic effect on the endometrium. This is the case with hormonal contraceptives and pure progestogens.
Types of polyps
Uterine polyps can be classified into different types according to their appearance and composition:
- Functional, functional or typical
- have an appearance similar to normal endometrium. They may present proliferative or secretory changes. Depending on what predominates in their composition (glandular or stromal component), they are subdivided into glandular, fibroglandular, and fibrous.
- Cystic
- arise from the quistification of glandular polyps.
- Hyperplastic
- have changes similar to those of endometrial hyperplasia. Hyperplastic endometrial polyps without atypia are benign. If they present atypia, they are considered precancerous.
- Atrophic
- are those frequently found in menopausal patients.
- Evil
- the polyp cells undergo a malignant process and become cancerous.
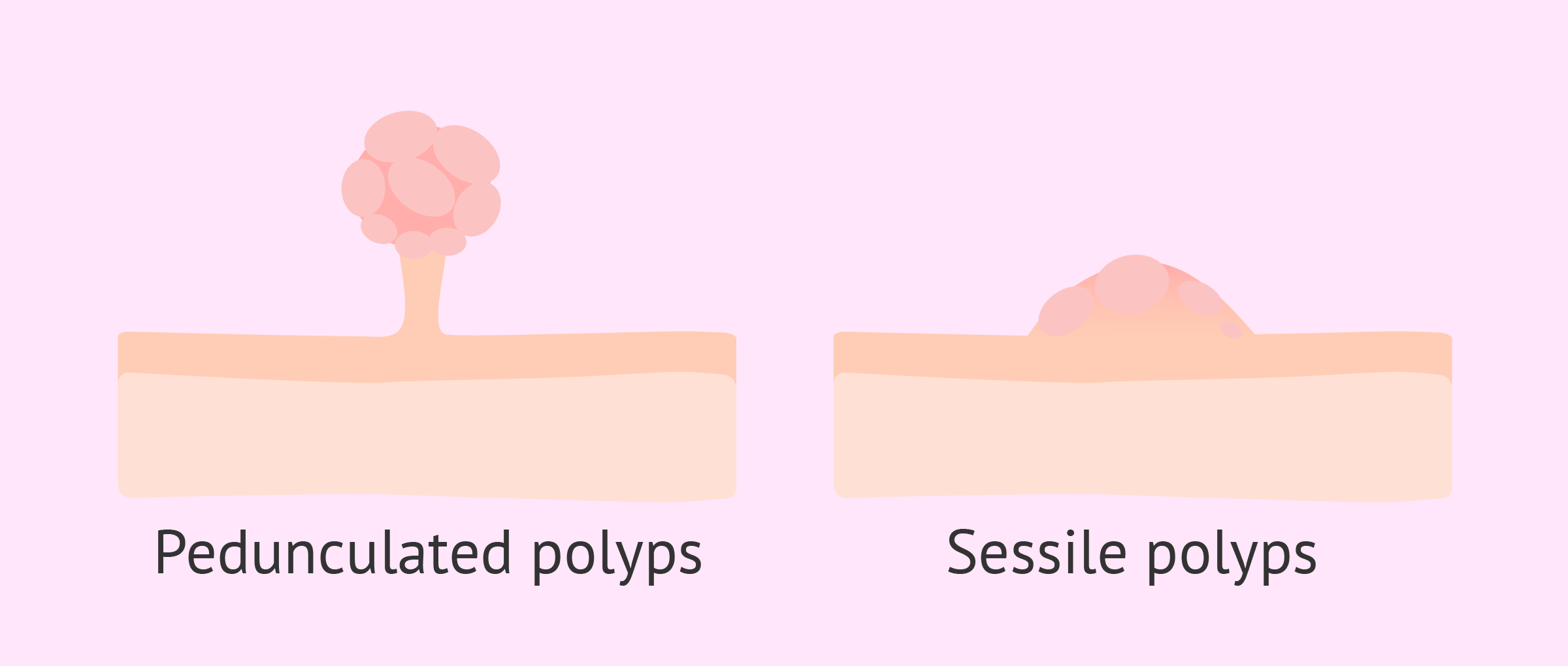
Two classes of polyps are also distinguished according to their shape, i.e., whether they are flatter or have relief.
On the one hand, there are pedunculated polyps that have a narrower stalk of implantation. In contrast, sessile polyps have a wider implantation base and are therefore flatter polyps than pedunculated polyps.
What symptoms do polyps cause?
Normally, small polyps are asymptomatic and the woman is not aware that she has them. This is what happens in 50% of patients.
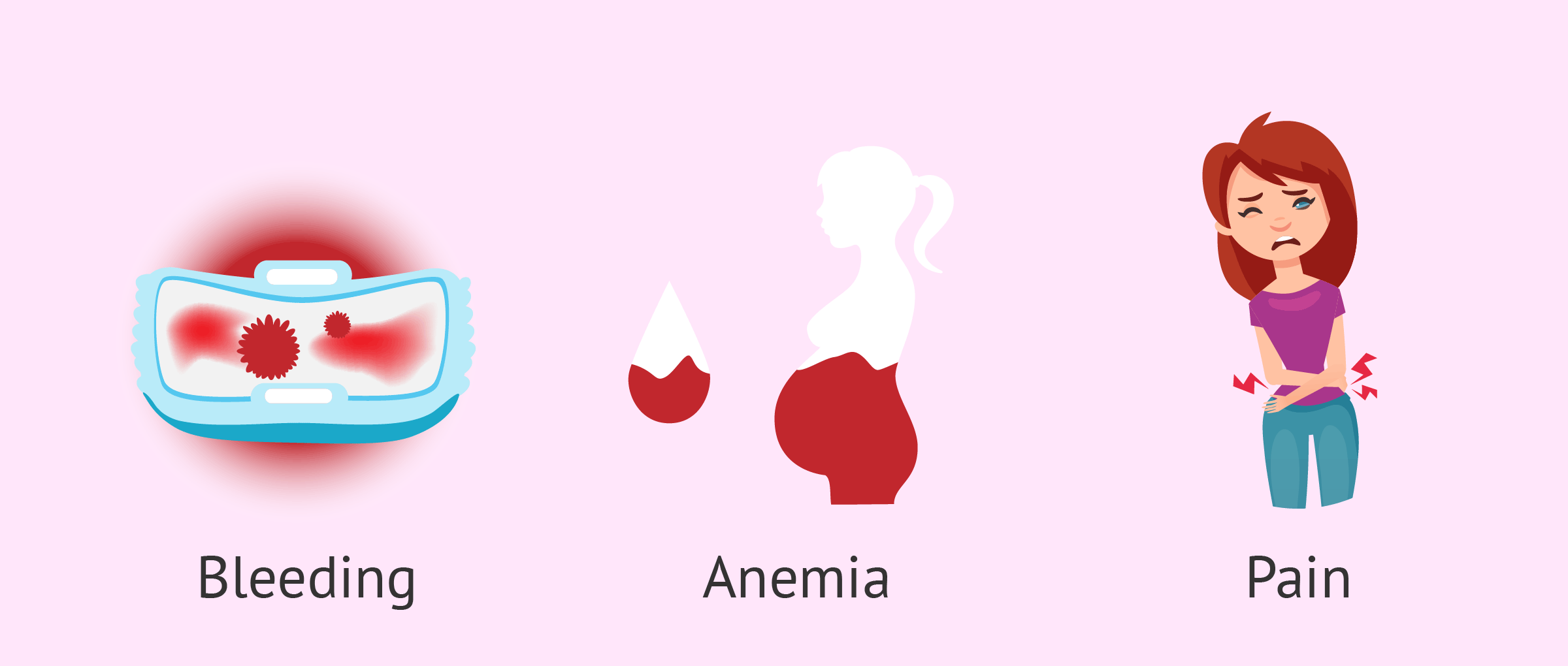
However, when the polyp grows and bleeds, its most characteristic symptom appears heavy bleeding during menstruation (hypermenorrhea).
Bleeding between menses (metrorrhagia) is also a common symptom of endometrial polyps and even bleeding after sexual intercourse. It is believed that 10-30% of irregular bleeding is related to the presence of endometrial polyps. In fact, they are the main cause of the stage close to menopause.
Another symptom that women may present is anemia due to the frequent and abundant hemorrhages caused by the polyps, as well as pain due to cervical dilatation.
In addition, the existence of uterine polyps can affect fertility, as they are associated with problems in achieving and maintaining pregnancy.
Diagnosis of uterine polyps
Polyps are usually found by the gynecologist in routine check-ups by transvaginal ultrasound. However, to confirm the presence of polyps in the uterus, the specialist may request the following complementary techniques:
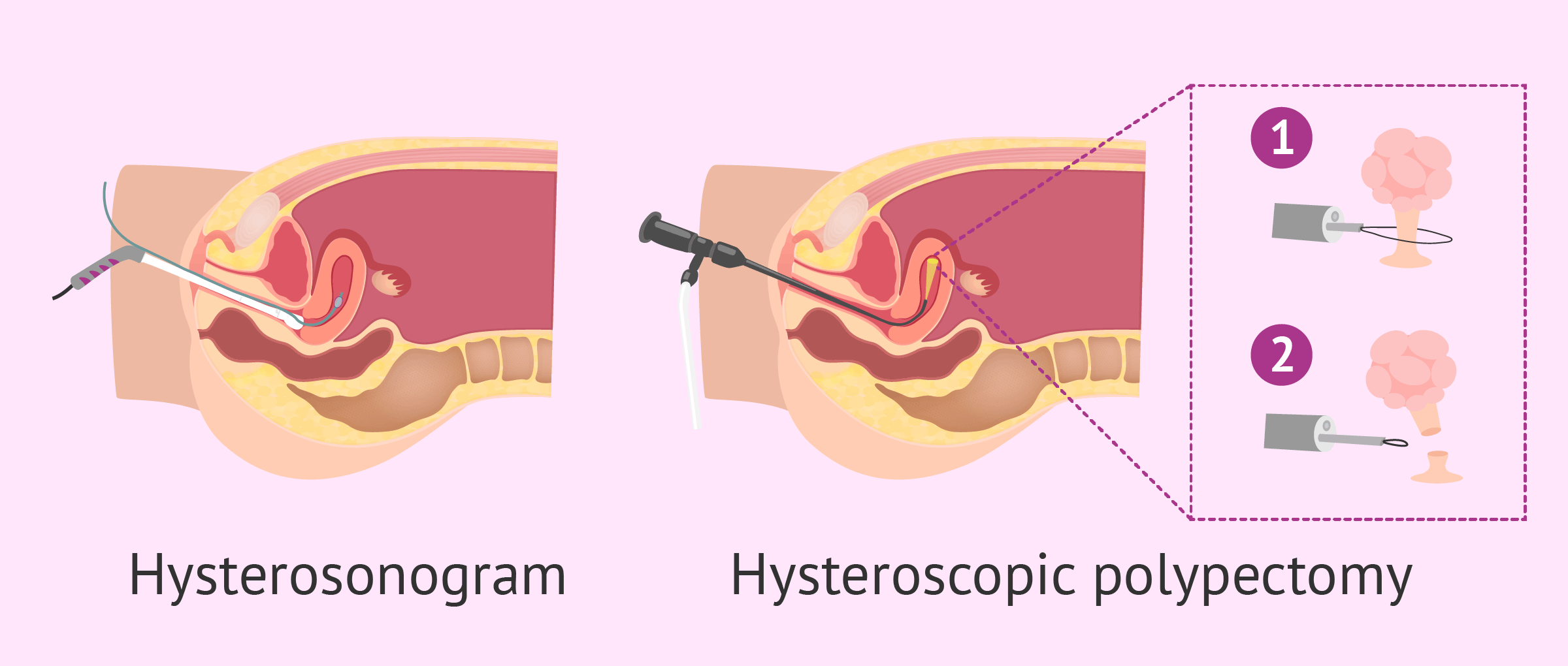
- Hysterosonography (or hydrosonography)
- consists of performing a transvaginal ultrasound by adding a sterile saline solution or serum via the vagina to detach the internal walls of the uterus and get a better view of the polyp.
- Hysteroscopy
- minor ambulatory surgery consisting of introducing an endoscope, which has a small material to operate, along with a light and a small camera into the uterine cavity. In this way, we obtain a digital image of the interior of the cavity. It can be performed with or without local anesthesia.
The method of choice to confirm the diagnosis is a hysteroscopy, which in turn allows a biopsy of the polyp, or its removal or resection (polypectomy by surgical hysteroscopy).
Do uterine polyps affect fertility?
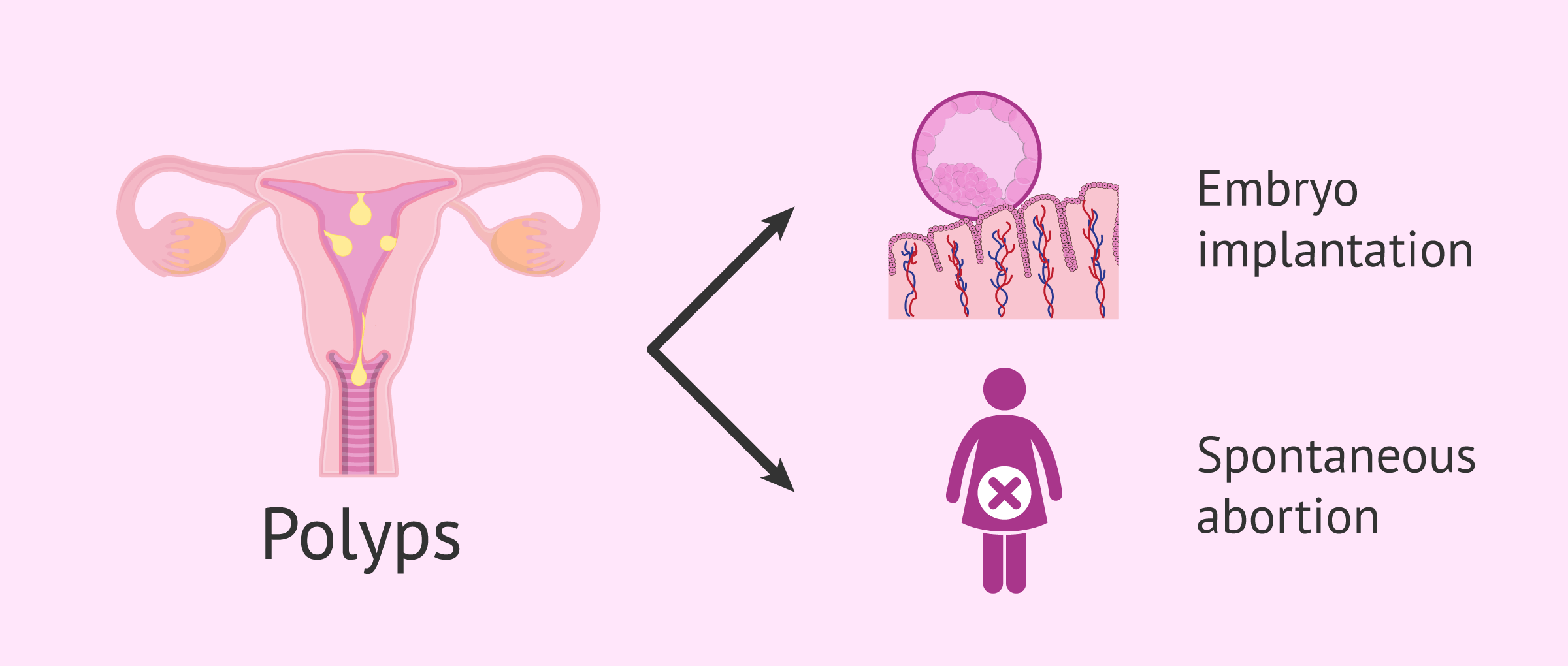
Polyps can be a cause of sterility and infertility in women, preventing embryo implantation or causing miscarriages.
The exact mechanism by which uterine polyps cause these problems in conceiving is not known. It is suspected that polyps affect endometrial development by causing bleeding and creating an inappropriate environment for embryo implantation to occur, thus affecting endometrial receptivity.
It has also been found that patients with polyps have increased a protein that inhibits the union between the egg and the sperm: glycodelin. Therefore, another step that may be altered is fertilization.
Between 15% and 32% of women with infertility problems have polyps in their uterus. Small polyps, less than 2 cm, do not decrease pregnancy rates in in vitro fertilization (IVF) treatment patients, but they do triple miscarriage rates. Therefore, restoration of a normal uterine cavity may be an important factor in increasing the likelihood of success of these techniques.
How are uterine polyps treated?
When endometrial polyps appear in premenopausal women and are totally asymptomatic, it is usually decided to perform ultrasound controls to assess the growth of the polyp.
Polypectomy is used for any endometrial polyp that presents symptoms and it is advisable to remove them when they are larger than 1 cm, even if the patient does not describe any symptoms. The main reason for opting for this alternative is that this type of polyps can become cancerous.
Usually, uterine polyp removal is performed by hysteroscopy. However, there are other forms of therapy for endometrial polyps.
In the case of small polyps, a scraping of the uterine cavity, called curettage, can be applied uterine curettage. However, this method is less effective. If complete resection of the base is not performed, there may be recurrences, that is, recurrent polyps that reappear.
Regardless of the treatment used, once the polyp is removed, a small portion of the polyp is sent to the pathology laboratory for analysis to confirm that it is a benign polyp.
Endometrial polyps and assisted reproduction
In all women who are going to undergo assisted reproduction treatment, it is advisable to remove the polyp before starting the treatment.
Fortunately, the diagnosis of polyps in these patients is usually rapid, as one of the first tests performed before starting fertility treatment is a transvaginal ultrasound, where the presence of polyps can be suspected and, if so, the patient can be referred for hysteroscopy.
In the case of a diagnosis, once the treatment has started, it will be decided what to do in each case on an individual basis: to perform the transfer or to freeze the embryos and cancel it in order to treat the polyp.
Assisted procreation, as any other medical treatment, requires that you rely on the professionalism of the doctors and staff of the clinic you choose. Obviously, each clinic is different. Get now your Fertility Report, which will select several clinics for you out of the pool of clinics that meet our strict quality criteria. Moreover, it will offer you a comparison between the fees and conditions each clinic offers in order for you to make a well informed choice.
FAQs from users
Does the type of endometrial polyp affect the chances of getting pregnant?
Endometrial polyp is a benign tumour within the uterine cavity and, depending on its size, may affect embryo implantation.
Are all polyps removed before starting assisted reproduction treatment?
Endometrial or uterine polyps are usually glands in the endometrial tissue that, for some reason, grow abnormally. This abnormal growth can be complicated by the hormone therapy required for a stimulation cycle in assisted reproductive treatment.
It should be understood that in the first phase of the menstrual cycle there is the secretion of estrogens that cause proliferation of the endometrial glands. However, in the second phase of the cycle, after ovulation, progesterone is the predominant hormone that causes endometrial atrophy and consequently the menstrual outcome if pregnancy does not occur.
For this reason, sometimes menstruation itself is responsible for eliminating the polyps, but if they persist, surgical removal is necessary prior to assisted reproduction treatment. The vast majority of endometrial polyps are benign, but in perimenopausal women may be the expression of endometrial cancer, which makes histological evaluation of the endometrium necessary.
Can young women also present endometrial polyps?
Yes, although it is less common for this type of patient to develop polyps, it may occur that this alteration appears. As in the other cases, it will be decided whether or not to remove them depending on the patient's medical history, the size of the polyps and the probability that they may be cancerous.
Can uterine polyps go away on their own?
Yes, some small polyps disappear or shrink on their own even if they are left untreated. If the patient presents no symptoms that complicate her normal lifestyle, polyps can be left alone and watched to see if they resolve by themselves. Sometimes, they are treated with medications that make polyps dissolve and disappear eventually.
Is an endometrial polyp the same as a submucosal uterine myoma?
No, although both are abnormal growths in the uterus and can sometimes appear very similar on hysteroscopy.
A submucosal myoma is a tumor formed by muscle tissue growing from the myometrium into the uterine cavity. Unlike most polyps, its superficial vascularization is striking.
However, fibroglandular polyps are highly vascularized and are of greater consistency, which can be mistaken for fibroglandular myomas.
Are uterine polyps contagious?
No. There are certain risk factors that may increase the likelihood of developing polyps, but there is no human-to-human transmission.
Do uterine polyps cause cancer?
Endometrial polyps, since they involve an abnormal growth of uterine tissue cells, are considered tumors. However, most uterine polyps are benign and do not cause serious problems. Only less than 5%, approximately, become cancerous or precancerous.
The chance of a polyp turning into a malignancy is greater if you are post-menopausal, take tamoxifen, or have heavy or irregular periods.
Can acupuncture help with uterine polyps?
Acupuncture, as well as other remedies such as Ayurveda and certain herbal treatments, are commonly believed to help with endometrial polyps. However, there is no scientific evidence of this and patients can turn to these treatments voluntarily.
It is often said that certain foods, such as ginger, cinnamon, or mustard seeds can make polyps disappear on their own. As a method for preventing their appearance, a balanced diet, rich in antioxidants, along with a healthy lifestyle can be beneficial, but there is no scientific evidence to date either.
The safest methods to deal with uterine polyps are the ones described through this article. Keeping in mind that polyps can turn into cancer, we do not recommend that you take unnecessary risks.
Recommended readings
As mentioned above, some of these polyps can become malignant. If you want to know more about this type of polyps, you will find more information in this article: Types, symptoms, and treatments of malignant uterine polyps.
On the other hand, if you are interested in learning more about the differences between uterine fibroids and uterine polyps, we recommend that you access the following link: What are fibroids and what are their symptoms?
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Lina Adomaitiene, Ruta Nadisauskiene, Mahshid Nickkho-Amiry, Arvydas Cizauskas, Jolita Palubinskiene, Cathrine Holland, Mourad W Seif. Tumor Suppression in Asymptomatic Postmenopausal Endometrial Polyps. Anticancer Res. 2020 Feb;40(2):789-794. doi: 10.21873/anticanres.14010.
Lolwa Mohammed Alansari, Peter Wardle. Endometrial polyps and subfertility. Hum Fertil (Camb). 2012 Sep;15(3):129-33. doi: 10.3109/14647273.2012.711499.
Luyan Guo, Fang Gu, Jinfeng Tan, Lu Luo, Jun Gao, Canquan Zhou. Multiple endometrial polyps is associated with higher risk of chronic endometritis in reproductive-aged women. J Obstet Gynaecol Res. 2021 Jan;47(1):389-396. doi: 10.1111/jog.14541. Epub 2020 Dec 9.
Malcolm G Munro. Uterine polyps, adenomyosis, leiomyomas, and endometrial receptivity. Fertil Steril. 2019 Apr;111(4):629-640. doi: 10.1016/j.fertnstert.2019.02.008.
Morris Wortman. "See-and-Treat" Hysteroscopy in the Management of Endometrial Polyps. Surg Technol Int. 2016 Apr;28:177-84.
Semra Yuksel, Guray Tuna, Hale Goksever Celik, Suleyman Salman. Endometrial polyps: Is the prediction of spontaneous regression possible? Obstet Gynecol Sci. 2021 Jan;64(1):114-121. doi: 10.5468/ogs.20242. Epub 2020 Dec 16.
Simone R de Rijk, Marlie E Steenbergen, Theodoor E Nieboer, Sjors F Coppus. Atypical Endometrial Polyps and Concurrent Endometrial Cancer: A Systematic Review. Obstet Gynecol. 2016 Sep;128(3):519-525. doi: 10.1097/AOG.0000000000001566.
S Salim, H Won, E Nesbitt-Hawes, N Campbell, J Abbott. Diagnosis and management of endometrial polyps: a critical review of the literature. J Minim Invasive Gynecol. Sep-Oct 2011;18(5):569-81. doi: 10.1016/j.jmig.2011.05.018.
T Justin Clark, Helen Stevenson. Endometrial Polyps and Abnormal Uterine Bleeding (AUB-P): What is the relationship, how are they diagnosed and how are they treated? Best Pract Res Clin Obstet Gynaecol. 2017 Apr;40:89-104.
FAQs from users: 'Does the type of endometrial polyp affect the chances of getting pregnant?', 'Are all polyps removed before starting assisted reproduction treatment?', 'How much does hysteroscopy for uterine polyp removal cost?', 'Do uterine polyps need to be removed?', 'Can young women also present endometrial polyps?', 'Can uterine polyps go away on their own?', 'Is an endometrial polyp the same as a submucosal uterine myoma?', 'Do uterine polyps cause cramps?', 'Do uterine polyps cause weight gain?', 'Are uterine polyps contagious?', 'Do uterine polyps come back?', 'How fast do uterine polyps grow back?', 'Do uterine polyps cause cancer?', 'Can uterine polyps prevent pregnancy?', 'Do uterine polyps go away after menopause?', 'Where do uterine polyps come from?', 'Can uterine polyps rupture?', 'Can endometriosis cause uterine polyps?' and 'Can acupuncture help with uterine polyps?'.
Authors and contributors

More information about Cristina Algarra Goosman






Hello, I’m 35 years old and I was detected an uterine polyp of 1 cm in June, 2015 as well as pelvic inflammatory disease. My doctor told me I had to take antibiotics and they worked, but I continued bleeding constantly until I started taking birth control pills during a week. Now I’m 5 weeks pregnant 🙂 So happy!!
Congratulations!