The cervix is the lower part of the uterus, which connects the vagina to the uterine cavity.
Its main function is to act as an initial barrier against the entry of spermatozoa into the female reproductive tract during sexual intercourse. The cervix is also the exit channel for blood during menstruation.
A woman may experience infertility due to cervical factor, for example, if the cervical mucus is too dense, which impedes the movement of the spermatozoa. However,this is not the only cause of cervical factor sterility in women.
Provided below is an index with the 8 points we are going to expand on in this article.
- 1.
- 1.1.
- 2.
- 2.1.
- 2.2.
- 3.
- 4.
- 4.1.
- 4.2.
- 4.3.
- 4.4.
- 5.
- 5.1.
- 5.2.
- 5.3.
- 5.4.
- 5.5.
- 6.
- 7.
- 8.
What is infertility of cervical origin?
The cervix is the canal that connects the vagina to the uterus. It measures approximately 3 cm and has two important functions in relation to fertility:
- It is the place where sperm cells enter on their way to fertilize the egg
- It is the channel through which the baby is born after 40 weeks of gestation during vaginal delivery.
Any alteration in the neck of the uterus may lead to a sterility problem. However, only 5-10% of couples with difficulty in achieving pregnancy have infertility caused by cervical factor.
In addition to the structure of the cervix itself, inside the cervix, we find a key component for female fertility: cervical mucus. We will now discuss their functions and features.
Cervical mucus
Cervical mucus or discharge is a mucous substance released by the cervix, whose appearance and consistency vary depending on the time of the woman's menstrual cycle due to the effect of sex hormones.
The main functions of cervical mucus are as follows:
- Change in consistency from thicker to more watery to allow the passage of spermatozoa at the time of ovulation
- Protect sperm from the vaginal environment
- Select the most suitable spermatozoa for fertilization, leaving behind those that are defective and with impaired motility
- Semen capacitation: nutrition of spermatozoa and separation of sperm components
In short, cervical mucus acts as the first filter for sperm to enter the uterus.
In the days close to ovulation, the cervical mucus is liquid and abundant due to the influence of estrogens. After the fertile days, this mucus becomes less, viscous, and thick as the release of progesterone begins.
If you want to learn more about cervical discharge and how it indicates a woman's fertile period, you can continue reading in the following post: What does the cervical mucus look like during the fertile period?
Cervical alterations
Cervical alterations that can lead to sterility due to a cervical factor can be differentiated into anatomical or functional.
In both cases, the correct migration of spermatozoa to the uterus and fallopian tubes is affected.
Anatomical alterations
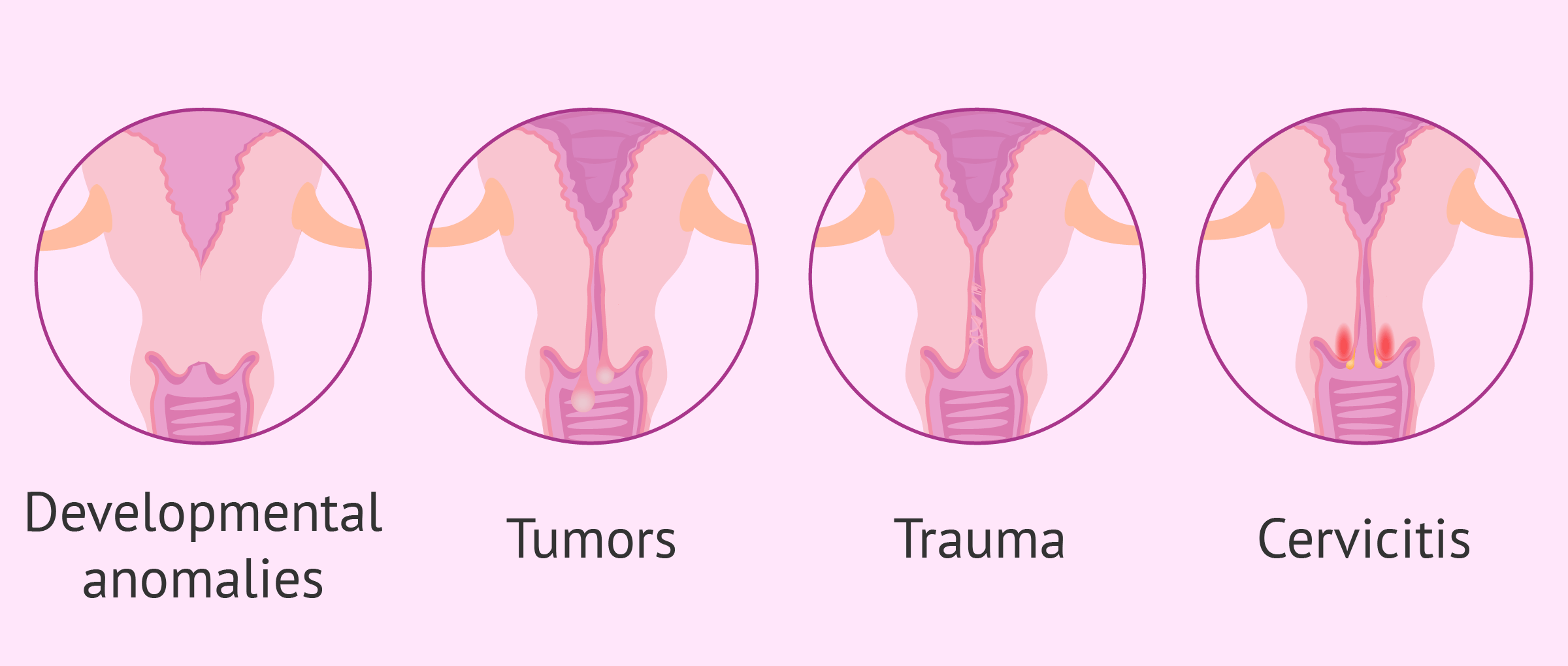
As a consequence of these pathologies, an obstruction of the cervix usually occurs. These are discussed below:
- Developmental abnormalities
- occur from birth as a result of defects in the fusion of the Müllerian ducts. For example, cervical duplication, cervical agenesis or cervical hypoplasia.
- Tumors
- such as polyps, fibroids or cysts. They are usually benign in origin and can be removed by surgery. The most serious case would be cervical cancer, which can be caused by human papillomavirus (HPV) infection.
- Trauma
- can be produced by surgery or appear occasionally. For example, tears, perforations, fistulas or incontinence of the internal and external orifices.
- Cervicitis
- acute or chronic inflammation of the cervix. It is usually caused by microbial infections such as chlamydia, Trichomonas vaginalis, candida or mycoplasma.
There are other alterations at the cervix level. However, their impact on women's fertility is minimal or with a very low incidence.
Functional alterations
This refers to the variation in the characteristics of cervical mucus, such as its consistency, quantity, acidity, etc.
Any alteration in the cervical flow can prevent sperm from entering the uterine cavity and, therefore, cause infertility.
The causes that provoke alterations in cervical mucus are the following:
- Insufficient estrogen release
- if during the follicular phase of the menstrual cycle an inadequate amount of estrogen is produced by the ovary, the cervical mucus becomes thicker and does not allow the passage of sperm when ovulation takes place.
- Medications
- clomiphene citrate has an anti-estrogenic effect on the ovaries.
- Infections
- the invasion of microorganisms into the cervix also causes an alteration of the mucus, as well as inflammation of the cervical walls.
- Antispermatozoa antibodies
- their presence in cervical mucus is also a consequence of infection.
If you want to know more about the role of estrogens in the female menstrual cycle, we recommend you read the following post: Estrogens.
What are the diagnostic tests for cervical factor?
Usually, cervical factor studies are not routinely performed in women with infertility problems. However, if the woman has symptoms or suspects that she may have some alteration of the cervix, it is possible to perform the following tests:
- Postcoital test (PCT or Sims-Huhner test)
- the presence or absence of motile spermatozoa in the cervical mucus after sexual intercourse is studied.
- Microbiological cultures
- to confirm if there is any bacterial infection.
- Cervical permeability test
- a cannula is inserted to check if it passes easily or if there is any obstruction.
- In vitro immunological test
- the mucus-semen interaction are evaluated, along with the characteristics, the ability of the sperm to pass through the cervical mucus and the presence of antisperm antibodies in both fluids.
- Hysteroscopy
- the inside of the cervix is studied with the introduction of a camera.
Prior to these tests, the gynecologist performs a physical examination and an ultrasound on all women who attend a check-up. In some cases, certain cervical abnormalities can already be detected in this initial examination.
How is cervical factor treated?
The treatment of cervical factor depends on the specific cause that is causing the infertility. In the following section, we will discuss the most frequent treatments currently available:
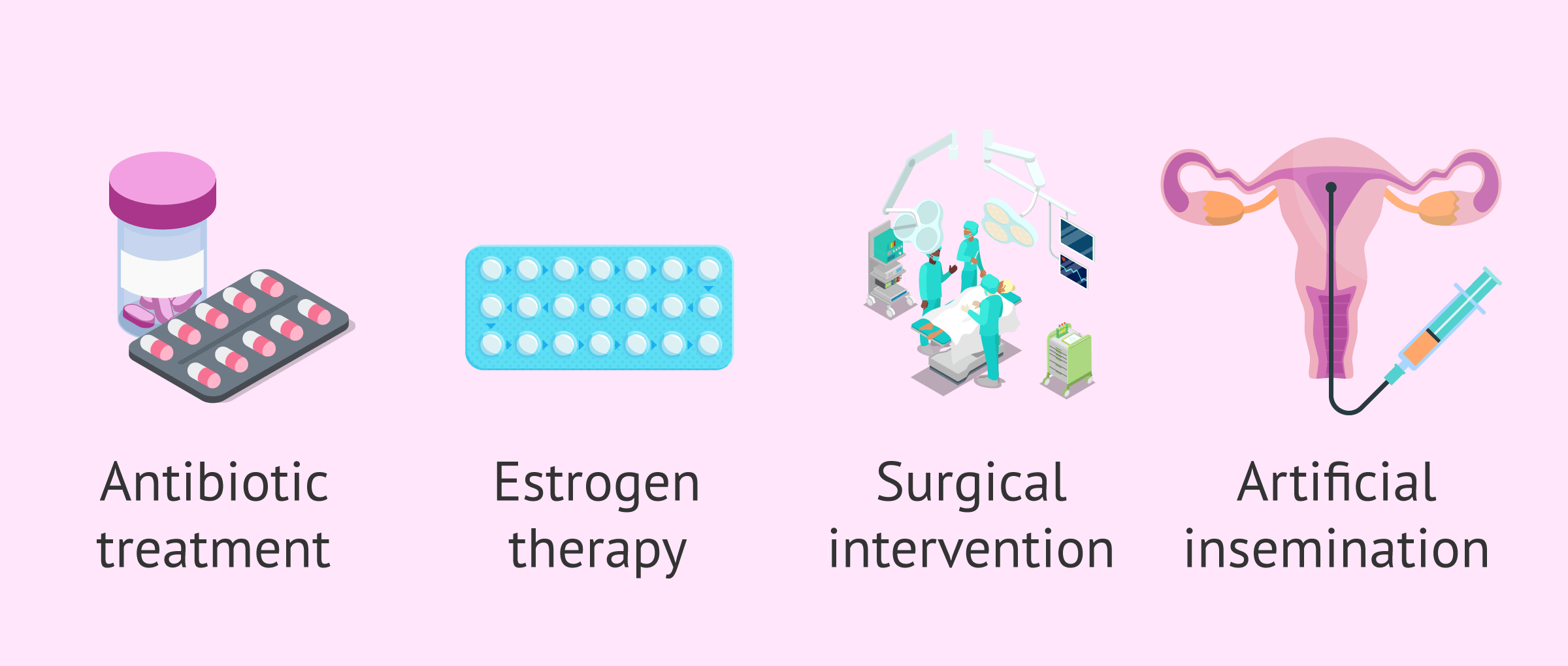
Antibiotics to treat cervical factor
Antibiotic medication is used in cases of vaginal infections or acute cervicitis.
First of all, it is necessary to identify the microorganism causing the infection in order to choose the appropriate type of antibiotic.
In the case of chronic cervicitis, the option of combining antibiotic treatment and surgery should be considered.
Estrogen therapy
In cases of insufficient or inadequate cervical mucus, administration of exogenous estrogens may result in an improvement in the quantity and quality of cervical mucus.
Estrogens should be taken during the first phase of the menstrual cycle, from approximately day 5 to day 13.
Surgical intervention
This is the appropriate method when there is a tumor that must be removed, as well as when there are anomalies in the development of the cervix. Cervical trauma should also be surgically repaired.
Finally, cauterization of the cervix is the most appropriate method to eliminate malignant cells or infectious agents.
For more information, you can continue reading with the following article: Cauterization of the cervix.
Artificial insemination (AI)
This assisted reproduction treatment is often advisable for couples or women with cervical factors who wish to have a child.
Artificial insemination is a very simple procedure that consists of introducing previously capacitated sperm inside the uterine cavity with an insemination cannula.
Therby, avoiding the barrier formed by the cervix and increasing the chances of pregnancy.
Did you know that we can help you to choose a fertility clinic for your IUI cycle? All you have to do is get your Fertility Report now. It is an easy-to-use tool that is capable of filtering the best clinics and tailor an individual report exclusively for you with useful tips that will help you make a well informed decision.
FAQs from users
Can alterations in the cervical mucus lead to female infertility?
Yes, alterations in the cervical mucus can are a common cause of female infertility. The cervical mucus is a secretion produced before ovulation and it disappears after the woman ovulates. It has a sticky texture, and its mission is to pave the way for sperm. It is, in fact, a good indicator of female fertility.
What is the cause of chronic inflammation of the cervix?
Inflammation of the cervix, also called cervicitis, can be acute or chronic. Although the causes of both types can be highly variable, they are usually due to infection by microorganisms such as for example, chlamydia, trichomoniasis, gonorrhea, herpes virus, and human papillomavirus.
Cervicitis can prevent pregnancy and cause infertility, as well as other discomforts such as leucorrhea, dysmenorrhea, pain during sexual intercourse, etc.
How is it possible to make an early detection of cervical alterations?
Normally, alterations affecting the cervix are detected in a routine gynecological examination with ultrasound or cytology. If it is not very clear or there is a cause of infertility that could be due to cervical factor, further tests can be performed, such as those explained in this article.
What is the difference between an endometrial polyp and an endocervical polyp?
Endometrial polyps are those that appear inside the uterine cavity. Alternatively, there are also cervical polyps, which form at the edge of the cervix, and endocervical polyps, that are found inside the cervical canal.
Polyps that form in the cervix can grow to protrude into the vagina.

You can find more information on this uterine pathology in the following link: What is an endometrial or uterine polyp? - Symptoms and treatment
What symptoms are caused by cervical factor infertility?
A possible symptom of cervical factor infertility could be problems related to cervical mucus. Those women with thick cervical mucus, mucus that does not change consistency during ovulation and/or have antibodies against sperm, will not be able to achieve pregnancy.
In addition, inflammation of the cervix or cervicitis can also cause female infertility. This usually causes discomfort during urination and a yellowish discharge.
Recommended reading
Cervicitis is a cause of female infertility due to a cervical factor. If you want to know in detail what this pathology consists of, we recommend you to read the following post: Cervicitis.
Artificial insemination is the appropriate technique to achieve pregnancy when there is sterility due to a cervical factor. You can find more information and a step-by-step process in the following article: Artificial insemination.
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Hartmann D, Rohkohl J, Merbach S, Heilkenbrinker T, Klindworth HP, Schoon HA, Hoedemaker M. Prevalence of cervicitis in dairy cows and its effect on reproduction. Theriogenology. 2016 Jan 15;85(2):247-53. doi: 10.1016/j.theriogenology.2015.09.029. Epub 2015 Sep 25 (show)
Jennifer M Oliveto, Lyudmila Muinov. Cystic Cervicitis: A Case Report and Literature Review of Cystic Cervical Lesions. J Comput Assist Tomogr. Jul-Aug 2016;40(4):564-6 (show)
M Josephine Lusk, Frances L Garden, Robert G Cumming, William D Rawlinson, Zin W Naing, Pam Konecny. Cervicitis: a prospective observational study of empiric azithromycin treatment in women with cervicitis and non-specific cervicitis. Int J STD AIDS. 2017 Feb;28(2):120-126. doi: 10.1177/0956462416628319. Epub 2016 Jul 10 (show)
M Lemert, L Mastroianni Jr. Cervical factors in infertility. Clin Obstet Gynecol. 1974 Dec;17(4):29-43. doi: 10.1097/00003081-197412000-00003.
Oliveto J, Muinov L, Cystic Cervicitis: A Case Report and Literature Review of Cystic Cervical Lesions. J Comput Assist Tomogr. Jul-Aug 2016;40(4):564-6. doi: 10.1097/RCT.0000000000000451
Shawn K Mattson, Julia P Polk, Paul Nyirjesy. Chronic Cervicitis: Presenting Features and Response to Therapy. J Low Genit Tract Dis. 2016 Jul;20(3):e30-3. doi: 10.1097/LGT.0000000000000225.
W D Rosenfeld, J Clark. Vulvovaginitis and cervicitis. Pediatr Clin North Am. 1989 Jun;36(3):489-511. doi: 10.1016/s0031-3955(16)36682-2 (show)
FAQs from users: 'Can alterations in the cervical mucus lead to female infertility?', 'What is the cause of chronic inflammation of the cervix?', 'How is it possible to make an early detection of cervical alterations?', 'What is the difference between an endometrial polyp and an endocervical polyp?' and 'What symptoms are caused by cervical factor infertility?'.
Authors and contributors
More information about Cristina Algarra Goosman

More information about Michelle Lorraine Embleton







Possibly I have an infection in the cervix, the doctor has told me that he has to do a culture but I don’t know what it is, it is painful? I don’t know what to expect…
Hello Patrishia,
Obtaining a sample of your cervix and analyzing it under the microscope will allow the gynecologist to identify what type of infection you have and therefore how to treat it.
To do this he will insert the speculum into the vaginal canal and with a small brush, the sample will be collected. It is uncomfortable but not painful, it can be done on an outpatient basis and no further treatment is necessary.
I hope I have helped you,
May everything go well!
Hello, I had a trauma due to a car accident and I have the cervical area affected, what treatment options do I have?
Hello lilylight,
Cervical factors due to trauma must be repaired by surgery, this intervention will be more or less invasive and complex based on the type of trauma and the state of the cervix.
I recommend that you go to your doctor so that he/she can assess and decide which is the best treatment for your particular situation.
I hope I have helped you.
Best regards.
How could I improve the quality of my vaginal discharge? In my case, I produce too many anti-sperm antibodies, so it literally kills sperm.
Dear margaret,
Firstly, let me explain you what are the characteristics you should look for in your vaginal discharge in order to determine whether you produce fertile cervical mucus or not:
1. Thick and watery consistency or stretchiness
2. Clear color, either a white or yellow tint
3. pH above 7
4. Possibly sweeter scent
To improve consistency, the most important thing to do is staying hydrated, just like should be done for improving your lips and skin. There are some herbal remedies like taking evening primrose oil, but there is no scientific proof that they actually work.
As for improving cervical mucus quality, the main thing to keep in mind is following an overall healthy TTC diet. By doing this, women usually get their body functioning as best it can as a whole. For instance, avoiding foods containing too much sugar, as well as processed foods, would be a good start.