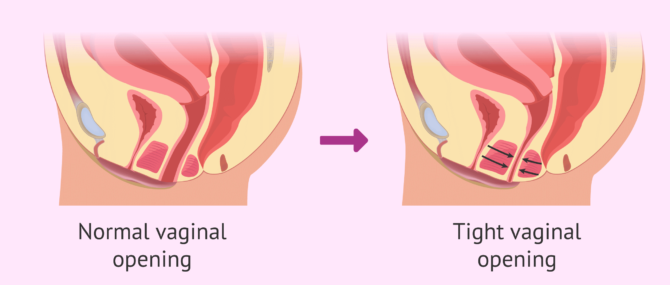
Vaginismus, also known as vaginism, is the involuntary contraction of the peri-vaginal muscles (lower third of the vagina) and the burning pain of the vagina during intercourse, a condition that prevents or makes vaginal penetration painful or even impossible.
It is a sexual dysfunction that affects a small group of female population, but it can be fixed after a treatment forged upon Sexology and Gynecology. Once fixed, it may improve female sexual well-being and tear down the barrier that was preventing the woman to fulfill her wish to be on motherhood.
Provided below is an index with the 11 points we are going to expand on in this article.
- 1.
- 1.1.
- 2.
- 3.
- 3.1.
- 3.2.
- 4.
- 4.1.
- 4.2.
- 5.
- 6.
- 7.
- 8.
- 8.1.
- 8.2.
- 8.3.
- 8.4.
- 8.5.
- 8.6.
- 8.7.
- 9.
- 10.
- 11.
Definition
Vaginismus or vaginism is the medical term for vaginal tightness and the resulting burning pain of the vagina during sexual relationships. It results from the involuntary tightening of the pelvic floor muscles, particularly the PC (pubococcygeus) muscle group, which causes painful spasmodic contractions in the vagina. Tightness is therefore the reflex action of the vaginal muscles. Some experts suggest the involvement of other muscles, like the bulbocavernosus, levator ani, perivaginal muscles, circumvaginal (CVM)...
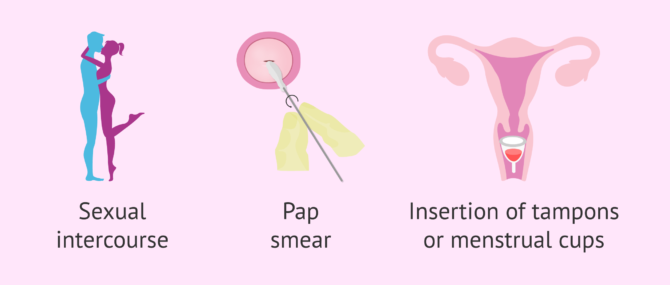
As a consequence, vaginismus affects a woman's ability to engage in vaginal penetration, including any form of penetration—from sexual intercourse to manual penetration, as well as the insertion of menstrual cups, tampons, vaginal capsules or "vagina eggs", etc.
Also, it is difficult for women affected by vaginism to undergo gynecological examinations or pap tests, as they involve manual penetration by the gynecologist. In short, vaginismus makes any kind of penetration painful or even impossible.
It should be clear that a woman affected by vaginismus does not consciously control the vaginal muscle spasm that occurs when any kind of penetration is attempted. It can be compared to the reflex of the eyes that is triggered by the sight of an approaching object.
Commonly confused words
The term vaginismus is often confused with other terms related to conditions of the vulvar region such as vulvar vestibulitis and vulvodynia. At times, it is confused with its most common symptom, dyspareunia, perhaps because they both are medical terms that often come hand in hand with one another. But one should know that they cannot be used interchangeably.
Firstly, women affected by vaginismus experience an involuntary contraction of the vaginal muscles that causes them to feel a sharp pain (i.e. dyspareunia) when attempting any form of vaginal penetration. On the other hand, dyspareunia is a symptom of both vaginismus and vulvar vestibulitis, as it is defined as painful sexual intercourse.
So, briefly, these are the definitions of each term:
- Vaginismus
- Tightening of the vagina.
- Vulvodynia
- Chronic pain around the vulvar region.
- Vulvar vestibulitis
- Chronic pain that appears when touching the vestibule or entrance of the vagina.
- Dyspareunia
- When sexual intercourse is painful. Pain can be localized on the external surface of the genitalia or deeper in the pelvis.
As a matter of fact, Vulvar Vestibulitis Syndrome or VVS, also known as vestibulodynia or simply vulvar vestibulitis, is a type of vulvodynia, that is, a chronic pain syndrome that affects the vulvar area.
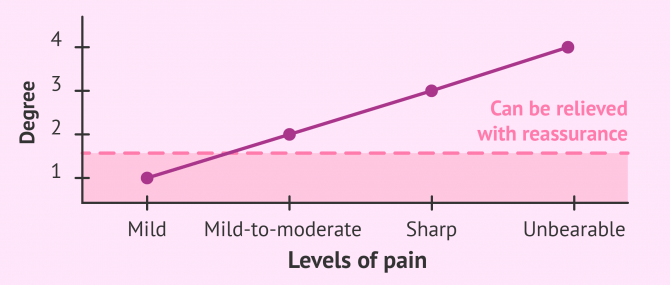
Degrees of severity
Vaginismus or vaginism has been classified into four degrees by Lamont (1978) in accordance with the severity of the condition. This classification is the one that continues to be used today.
- First degree
- Patients affected by grade 1 vaginismus experience mild symptoms and the pain they experience is likely to be relieved with just reassurance. It often appears in the form of mild discomfort that may diminish during intercourse.
- Second degree
- This is a mild-to-moderate form of vaginismus in which discomfort, which includes burning and tightness, is present and maintained throughout the pelvis even with reassurance.
- Third degree
- The patient experiences a sharp pain and unconsciously tends to elevate the buttocks to avoid being touched. Entry and movement are very difficult and extremely painful.
- Fourth degree
- It is the most severe form of vaginismus, in which the woman elevates the buttocks and even closes the thighs closely to avoid any kind of approach. Penetration is impossible and entry comes in the form of an unbearable pain.
Some authors have expanded this classification to a fifth type in which the patient experiences symptoms such as sweating, palpitations, nausea, shaking, hyperventilation, losing consciousness, etc.
Types
We can classify the types of vaginismus into two groups, primary and secondary vaginismus, depending on the moment of a woman's life at which it develops:
Primary vaginismus
Primary vaginismus is the inability to experience vaginal penetration without pain. It is often discovered in adolescence or in the woman's early 20s, as it is usually the time period when women engage into sexual intercourse for the first time, start using tampons, or undergo their firs gynecological examination.
Although kind of vaginismus is considered idiopathic, the following conditions can contribute to primary vaginismus:
- Urinary Tract Infections (UTIs)
- Vulvar Vestibulitis Syndrome (VVS), vestibulodynia or vulvar vestibulitis
- Yeast infections
- Chronic pain conditions
On the other hand, when primary vaginismus has a psychological origin, it can be motivated by the following situations or factors:
- History of sexual abuse, rape, sexual assault, or attempted sexual abuse/assault
- Having witnessed sexual and/or physical abuse of others
- Penetration phobia
- Any physically invasive trauma, even if the genitals are not involved
- Anxiety and/or stress
- Negative emotional reactions linked to sexual stimulation
- Educational factors associated with religious beliefs, ethical issues, etc.
Secondary vaginismus
Secondary vaginismus occurs when a woman who has been previously able to achieve penetration develops this condition, and is therefore unable to have intercourse or other forms of penetration anymore.
If the cause has a physical origin, it is often associated with:
- Yeast infections
- Trauma during childbirth
- Drying of the vulvar and vaginal tissues during peri-menopause and menopause, as a result of reduced estrogen
On the other hand, secondary vaginismus can be caused by psychological factors, which in many cases are linked to primary vaginismus as well, including:
- History of sexual abuse, rape, sexual assault, or attempted sexual abuse/assault
- Fear of or difficulty with losing control
- Distrusting one's partner
- General misconceptions about sex
- Undiscovered sexual orientation (asexuality or homosexuality)
- Feelings of being a transgender man
Causes
The impossibility of being penetrated may have a psychological or physical origin, or even one can be a byproduct of the other:
Psychological reasons
Psychological disorders are often the most common cause of vaginismus. Below, we will comment on the most important ones:
- Lack of sex education or education linked to taboos and prejudices.
- Poor awareness of one own's or partner's body.
- Low self-esteem or dissatisfaction with one's body image.
- Non-sexually related childhood trauma.
- Fear of getting pregnant.
- Fear of loosing virginity.
- Failings at the beginning of ones sex life.
- Previous negative sexual and/or gynecological experiences.
- Having been raped, abused or assaulted.
- Suffering from anxiety or depression.
To combat vaginismus where it comes from, a complete sex education from childhood for all girls is very important. Frequently, the lack of information is a fundamental pillar for the presence of vaginismus, since it makes people face sexual relations with fear.
All of the psychological causes previously mentioned can be worked on and help sought from professionals. They will be in charge of providing all the necessary tools to alleviate and solve this sexual dysfunction.
Physical reasons
Physical or physiological causes of vaginismus are less common than those we have already discussed, but it is also important to consider them:
- Rigid hymen.
- Vaginal infections and/or the appearance of vaginal ulcers.
- The inflammation of the Bartholi glands, located at the entrance of the vagina and which contribute to its lubrication.
- A traumatic abortion or birth.
- Poor healing of the episiotomy (incision made to facilitate the baby's exit at birth).
- The decrease of estrogens in the blood, as occurs in menopause, since it causes an increase in vaginal dryness.
- Pelvic Tumors.
The involuntary contraction of the vagina and the pain associated with it may be due to a physical reason that requires gynecological treatment, in addition to a possible psychological approach.
Symptoms & signs
The most common sign leading women to suspect that they may have vaginismus is sexual penetration being painful or truly impossible. This major sign, along with the following symptoms, can help a women tell if she has vaginismus:
- Painful intercourse (dyspareunia), with burning, stinging or vaginal tightness
- Tearing sensation or feeling like the man is "hitting a wall"
- Discomfort when inserting a tampon, menstrual cup or during a pap smear (pelvic exam)
- Generalized muscle spasms in other body muscle groups, like the legs, lower back, etc.
- Visceral reactions during attempted intercourse: breathing cessation, hyperventilation , palpitations, trembling...
- Ongoing sexual pain of unknown origin
- Unconsummated marriage
- Diminished libido due to pain
It should be clear that vaginismus does not prevent women from getting sexually aroused, but the constant feeling of pain when attempting to have intercourse leads to diminished libido levels. In other words, it is a side effect of vaginismus, not a directly related symptom.
Treatment
Vaginismus must be treated with the join collaboration between specialized psychologists and gynecologists in order to address the dysfunction across all its strands. Unfortunately, there is no surgery, vitamin supplement, or drug that can cure vaginismus.
Some medications, however, can help relieve and manage pain caused by vaginismus, but they cannot cure this condition unless the root of the problem was discovered and able to be fully addressed.
Couple therapy in combination with a physical therapy that involves pelvic floor exercises can help with vaginismus. Some of the latter are the Kegel exercises, which help the mother to monitor her pelvic musculature. Relaxation and breathing techniques are also prescribed, and the progressive use of vaginal dilators is advisable, too. These exercises should be done with someone's help, as it creates a relaxed environment.
Topical application of Lidocaine Gel or Jelly has been shown to work in some cases of unconsummated marriage according to some studies. Also, there is some research into the use of Botox as a treatment for vaginism, which would require the use of vaginal dilators as well. In any case, the use of Botox for vaginismus is still in an experimental phase.
In many occasions the dysfunction may lead to dyspareunia, experiencing thus pain during penetration. This may occur just once or multiple times. That may provoke an unconscious association between penetration and pain, making a reflex contraction of the vagina.
The resulting dyspareunia-vaginismus vicious circle prevents sexual relations. In such cases, it is crucial to visit a sexologist in order to achieve pleasant and anxiety-free sexual relations.
Getting pregnant
Although you may have heard that pregnancy is still possible in spite of vaginismus because what is called splash ejaculation or splash conception does work, actually the chances for you to get pregnant with this method are so low that we cannot consider them as a successful option for achieving pregnancy in cases of vaginismus.
Rarely, if the male ejaculates by the woman's genital lips, the semen containing sperms migrates into the vagina, causing the fertilization of the ovum and subsequent pregnancy. This is what is commonly known as splash conception or splash ejaculation.
A woman who suffers from vaginismus can achieve successful sexual intercourse with the help of Kegel exercises and vaginal dilators that allow her to have intercourse with penetration and ejaculation. In mild cases, the use of Lidocaine Gel can help get rid of pain and allow the couple to have intercourse free from pain.
When a patient with vaginismus gets pregnant, she may experience difficulties with pelvic exams and other pre- and post natal procedures, as well as delivery. For this reason, these patients are strongly recommended to resolve this dysfunction prior to delivery or even pregnancy.
FAQs from users
Does vaginismus cause infertility or female sterility?
Vaginismus is the involuntary contraction of vaginal muscles that causes pain during sex. This contraction will not influence the other functions of the rest of the reproductive system.
Likewise, vaginismus is not a cause of sterility (a situation in which a couple has tried to get pregnant for at least one week without success), much less infertility (repeated miscarriage), except in the situation where vaginismus prevents complete sexual intercourse, of course.
I suffer from vaginismus but I want to get pregnant. Which fertility treatment do you recommend?
Ideally, treatment of vaginismus should be the solution to the couple's "sterility problem". Once sexual dysfunction has been overcome, pregnancy can be achieved naturally.
Vaginismus treatments are often long, which can conflict with the desire for motherhood, especially in cases where age or ovarian reserve are in limit ranges. In cases of this type, we may find ourselves in the need to start reproductive treatments directly. These range from vaginal insemination of the semen sample at the time of ovulation, a technique that does not require medical assistance if the woman is able to self-inoculate the sample, to more complex reproduction techniques. Self-insemination can be the first step for young couples with no known pathology. At older ages, the relevance of carrying out sterility tests and reproduction treatments will be evaluated in each case.
Read more
How common is vaginismus?
Statistics have shown that about 2 in every 1,000 women have vaginismus. However, this figure could be higher, as gathering reliable information is difficult due to shame and embarrassment of the patient, or because some women are given an incorrect diagnosis and therefore are never properly treated. Moreover, it is estimated that 54% of the patients diagnosed with vaginismus are aged 26-35.
Is vaginismus curable?
Yes. In fact, it is considered to be one of the most easily treated female sexual disorders. A number of women have achieved successful sexual relationships with the proper treatment. However, the truth is, it does not involve drugs, surgery, hypnosis, or any other invasive technique.
Kegel exercises (pelvic floor exercises) in combination with insertion or dilation training are in the majority of cases the best and most successful options. Moreover, the good news is that they can be completed at home. It is important to be patient and be aware that it is a step-by-step process whereby success can be achieved progressively.
Does hypnotherapy work for vaginismus?
Actually, it does not. Neither do other invasive techniques such as surgery or certain drugs often advertised on the Internet. To put it simply, treating vaginismus requires the woman to overcome straight-forwards retraining process that can only be done with the help of pelvic floor exercises and dilators.
Can you treat vaginismus at home?
Yes, in fact, that's the treatment option that really works for vaginismus. Kegel's exercises or pelvic floor exercises, in combination with the progressive use of vaginal dilators, are the best option to help with vaginismus and eventually cure it. These exercises can be completed at home, which allows women to do them in private.
How long does it take to cure vaginismus?
On average, most women are able to overcome vaginismus in 6-10 weeks time. It should be clear, however, that treating vaginismus requires an intense full-time effort, in combination with professional assistance if necessary.
Suggested for you
Throughout this post, we have made several references to dyspareunia or pain during sexual intercourse. How does it feel? Where is it localized? Learn more about it here: Pain during Sexual Intercourse.
Vaginismus or vaginism is a primary cause of infertility of vaginal origin. What do you know about female infertility? If you want to learn about other causes leading to infertility in women, visit this guide: What Causes Female Infertility? – Definition, Signs & Treatment.
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Binik, YM. The DSM diagnostic creiterio for vaginismus. Archives of sexual Behavior 2010; 39(2): 278-291 (View)
Brosens C, Terrasa S y Astolfi E. Vaginismo. Evid Act Pract Ambul. 2009; 12(3): 102-103 (View)
Cabello-Santamaria F, Río-Olvera FJ, Cabello-García M. Sexual Pain disorders. Curr Opin Psychatry 2015; 28(6): 412-7 (View)
Melnik T, Hawton K, McGuire H. Interventions for vaginismus. Cochrane Database Syst Rev. 2012 Dec 12;12(12):CD001760. doi: 10.1002/14651858.CD001760.pub2 (View)
Pacik P. Understanding and treating vaginismus: a multimodal approach. Int Urogynecol J. 2014 Dec;25(12):1613-20. doi: 10.1007/s00192-014-2421-y. Epub 2014 Jun 4 (View)
Tourrilhes E, Veluire M, Hervé D, Nohuz E. Obstetric outcome of women with primary vaginismus. Pan Afr Med J. 2019 Apr 8;32:160. doi: 10.11604/pamj.2019.32.160.16083 (View)
FAQs from users: 'Does vaginismus cause infertility or female sterility?', 'I suffer from vaginismus but I want to get pregnant. Which fertility treatment do you recommend?', 'How common is vaginismus?', 'Is vaginismus curable?', 'Does hypnotherapy work for vaginismus?', 'Can you treat vaginismus at home?' and 'How long does it take to cure vaginismus?'.
Authors and contributors
-77x77.jpg)







Hi, I’ve got degree 3 vaginismus (severe vaginismus) and pelvic exams for me are entirely impossible… the same applying to sex with boyfriend. But I don’t know how, we managed to get pregnant and I’m in a bundle of joy now!!!!!! The problem now is that I’m kinda lost… how does pregnancy work with this condition? Will it affect the delivery of the baby? I’m kinda lost actually. Thanks for your help!
Hello America,
You should talk with your doctor about this. Anyway, perhaps continuing to use vaginal dilators can be helpful until delivery, and moreover they can make gynecological examinations easier. Also, anxiety and fear of childbirth can worsen the situation, so my advice is that you try to stay as relaxed as possible now. Have you considered seeking the support of a therapist?
I hope I have been able to help,
Best wishes