Endometriosis is a pathology that usually arises in reproductive age and is characterized by the presence of endometrial tissue in places outside the uterine cavity. Normally, endometrial tissue appears in the ovaries, although it can also be in the fallopian tubes or even in the intestine.
Pelvic pain and a series of other symptoms can be signs of endometriosis, but they are not very specific, i.e. they can appear in association with other pathologies. Therefore, it is necessary to make a differential diagnosis to confirm that the woman has endometriosis and the degree of severity of endometriosis if there is any suspicion of this disease.
Provided below is an index with the 8 points we are going to expand on in this article.
- 1.
- 2.
- 2.1.
- 2.2.
- 2.3.
- 3.
- 4.
- 5.
- 5.1.
- 5.2.
- 5.3.
- 5.4.
- 5.5.
- 6.
- 7.
- 8.
How to know if endometriosis exists?
Often, the diagnosis of endometriosis is quite complicated and can even take a long time. The main symptom that makes a specialist suspect this pathology is pelvic pain, typically at the time of menstruation (dysmenorrhea). Despite this, it is important to know that between 15% and 30% of patients with endometriosis remain asymptomatic for long periods of time.
When a woman suspects endometriosis or any other pathology, it is recommended that she consult her doctor as soon as possible. He will ask a series of questions about the symptoms, in addition to a pelvic examination.
Therefore, a detailed clinical history, followed by a gynecological examination including speculoscopy and vaginal examination will be the initial steps to detect the presence of endometrial tissue outside the uterine cavity.
Once this has been done, the specialist can request complimentary tests to establish a reliable diagnosis and, in this way, propose the best treatment for the woman.
In the following sections, each of the frequent medical tests for the diagnosis of endometriosis is detailed.
First diagnostic tests for endometriosis
As we have already commented above, if the woman has any suspicion of endometriosis or pelvic pain, the best thing to do is to go to her gynecologist. He/she will be in charge of studying the tests to request.
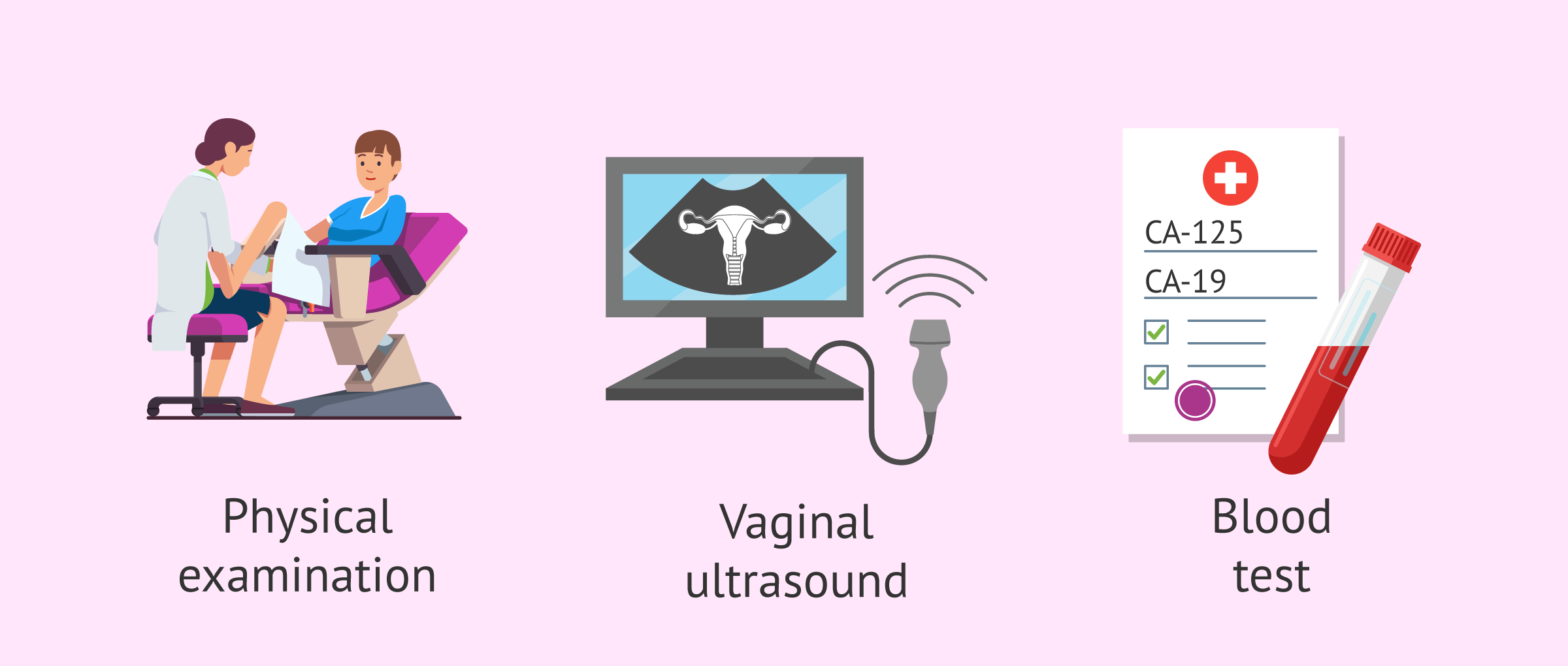
The following are the initial medical tests for the process of diagnosing possible endometriosis.
Gynecological examination
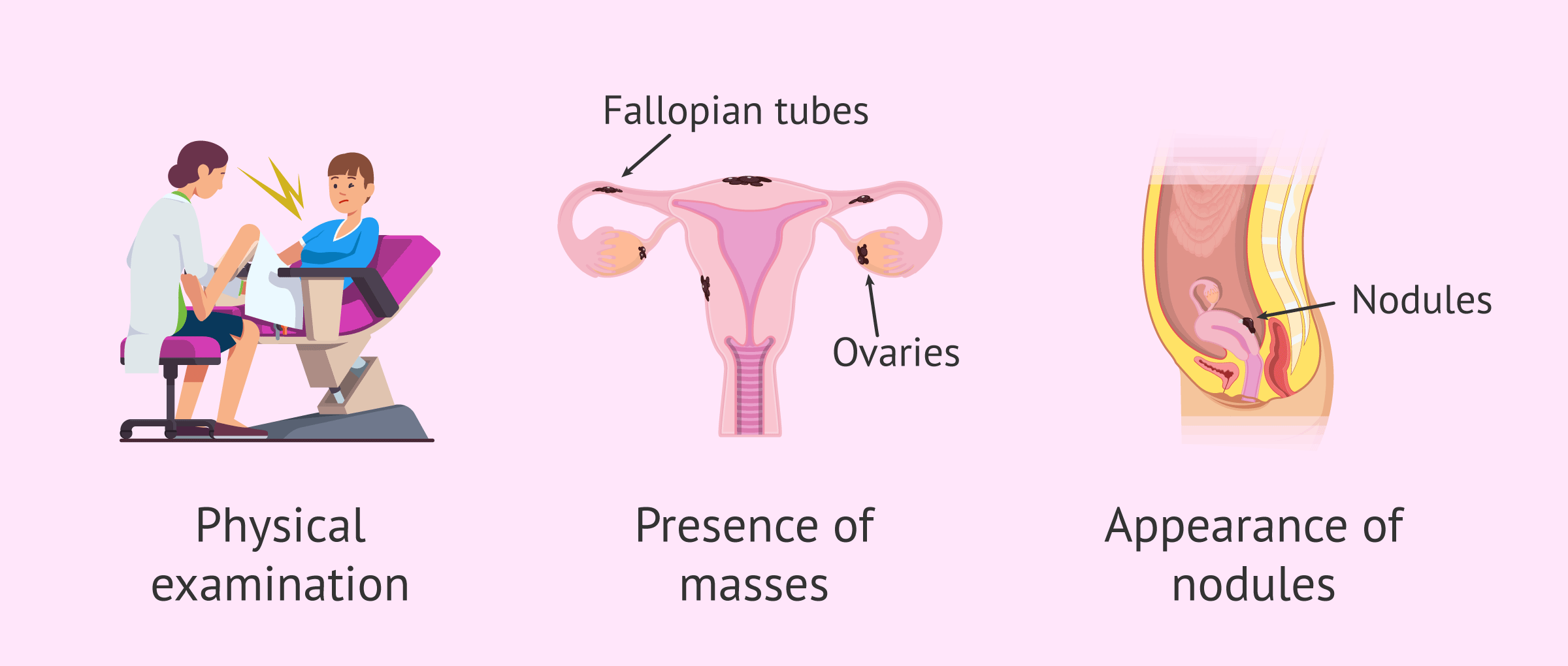
When endometriosis is suspected, the first step to follow is to perform a physical examination, a complete pelvic examination. Generally, this gynecological analysis does not allow the diagnosis of endometriosis, since the implants may be located outside the pelvic cavity or the size of these may not be large enough to palpate them.
Even so, there are some signs that could be detected through a gynecologic examination that would indicate suspicion of endometriosis:
- Pain on palpation of the fundus of the vagina or uterine ligaments.
- Painful nodules at the fundus of the vagina, ligaments or in the rectum.
- Pain with movement of the uterus.
- Masses in the fallopian tubes or ovaries.
- Lateral displacement of the cervix.
- Ovaries, fallopian tubes or uterus fixed, without mobility.
However, the specialist will not be able to reach a definitive or reliable diagnosis with only the identification of some of these signs. Therefore, further tests will be necessary.
Sonography
Ultrasonography or sonography consists of using an ultrasound probe to be able to indirectly observe the organs of the pelvic cavity. This test can be performed transabdominally or transvaginally.
Specifically, to be able to see the female sexual organs (uterus and ovaries), transvaginal ultrasound is usually used, in which the ultrasound probe is introduced through the vagina. This type of ultrasound can detect ovarian cysts, including endometriomas or chocolate cysts characteristic of severe endometriosis.
However, a transvaginal ultrasound will not clearly visualize endometrial adhesions in other organs. So, only an experienced physician will be able to see signs of bowel, uterine, bladder, or adenomyosis endometriosis.
Laboratory tests
Laboratory tests for the diagnosis of endometriosis consist of performing a simple blood test to study a tumor marker called Ca-125. The values of this marker may be increased in women with endometriosis, especially when the ovaries are affected.
However, the Ca-125 marker does not provide a clear and concise test for the diagnosis of endometriosis. Not every time endometriosis is present, this molecule is elevated above normal levels.
In addition, the amount of Ca-125 marker may also be increased in case of ovarian cancer, fibroids, peritonitis, pregnancy, and even during menstruation. Therefore, it is not a specific biomarker of endometriosis.
Elevated Ca-125 biomarker levels are quite often associated with severe and profound endometriosis. Despite this, this marker is not useful for the diagnosis of mild endometriosis.
Another useful marker for the diagnosis of endometriosis is the serum CA 19-9 antigen, but it has a lower sensitivity than Ca-125. Primarily, the information provided by Ca-19 can be related to the degree of severity of endometriosis once diagnosed.
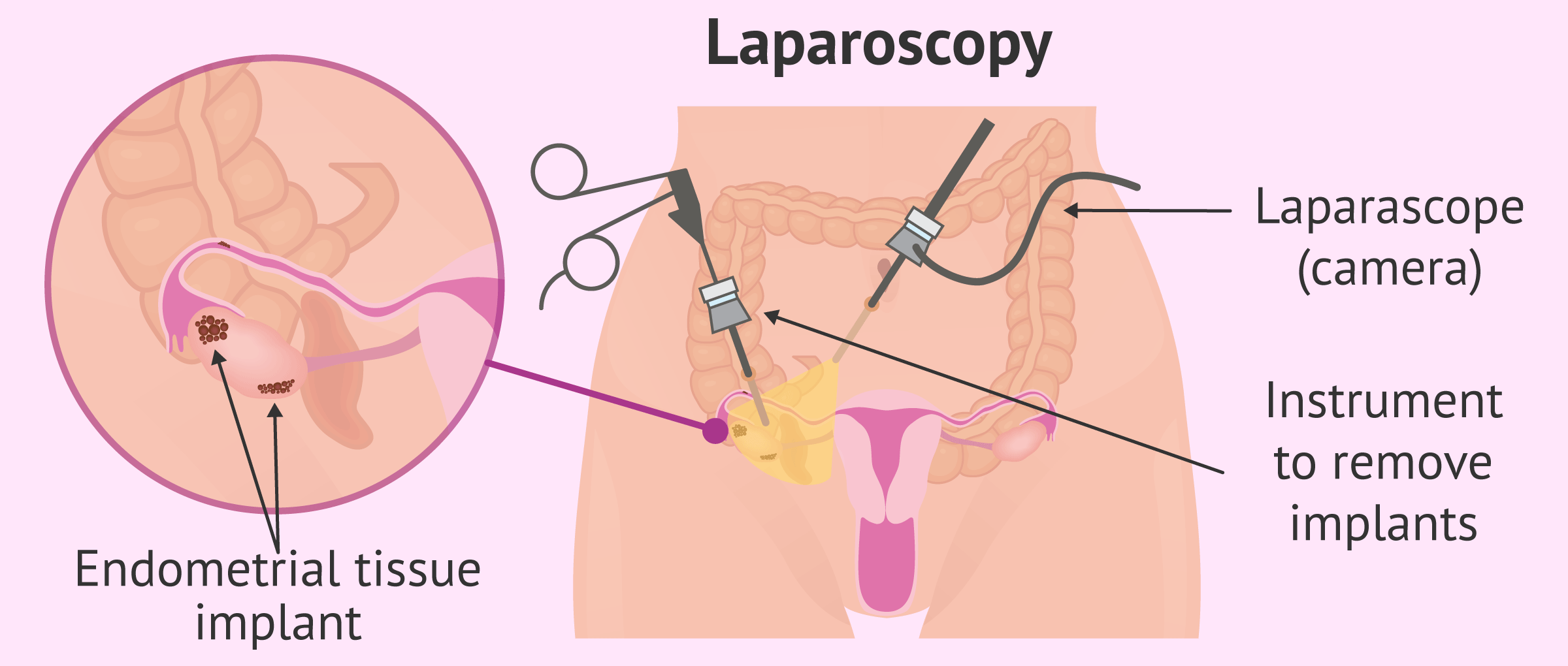
Laparoscopy for the diagnosis of endometriosis
The only way to give a certain diagnosis of endometriosis is by surgical intervention. The method used is laparoscopy, a surgery in which a camera connected to a rigid tube (laparoscope) is inserted through a small incision, usually in the navel.
The images obtained by the camera are amplified and transmitted directly to a screen. This surgical procedure is performed under general anesthesia, so the woman feels no pain.
Thanks to the camera attached, the internal organs and the walls of the pelvic and abdominal cavities can be directly observed for endometriomas or endometrial implants. In addition to being a diagnostic method, laparoscopy will also make it possible to remove endometrial implants that are accessible.
Additional tests
There are additional tests that the physician may order in case of suspected endometriosis. These complementary studies are usually recommended when the specialist thinks that it may be deep infiltrative endometriosis, one in which the implants go deep into the organs.
Listed below are some of the additional tests for diagnosing endometriosis:
- Magnetic resonance imaging (MRI)
- is a non-invasive technique that allows imaging of the interior of the organs from multiple planes thanks to radio waves, without using X-rays. It makes it possible to detect endometriosis implants with a minimum size.
- Colonoscopy
- is the technique that allows exploring the interior of the large intestine by means of an endoscope, a camera connected to a flexible tube that is introduced through the anus. Colonoscopy is used when there is suspicion of infiltrative endometriosis of the rectum or colon.
- Cystoscopy
- is the exploration of the inside of the bladder using an endoscope, an instrument inserted through the urethra. This test is performed when there is suspicion of infiltrative endometriosis of the urinary (bladder) bladder.
Colonoscopy and cystoscopy, as well as laparoscopy, are usually performed when the woman is menstruating to make it easier to locate endometrial implants. The explanation is that the implants bleed during menstruation.
FAQs from users
How is the diagnosis of endometriosis carried out?
Diagnosis of endometriosis is difficult and may take several years. The main symptom of suspected endometriosis is pain during menstruation. Therefore, a detailed anamnesis together with a gynecological examination are the first steps in the diagnosis of endometriosis.
Specifically, transvaginal ultrasound is the most useful test for the detection of endomyomas in the ovaries. In addition, other complementary tests in the diagnosis of endometriosis are magnetic resonance imaging, laparoscopy, and abdominal ultrasound, for example.
Read more
If endometrial implants are found during laparoscopy, how are they removed?
The surgeon can use different instruments to remove the implants once the endometriosis has been detected. Scissors, burning current forceps or even lasers can be used for greater precision. It will depend on where the endometrial tissue is located and its extent.
Do diagnostic tests for endometriosis hurt?
The only test that can hurt is laparoscopy, which is a surgical procedure. General anesthesia is used, so the patient will be sedated during the procedure and will not notice anything, but when the anesthesia wears off you may notice pain, so you may need analgesics.
The pain usually derives from the distension of the abdomen with gas, which may have irritated some nerve. This distension is necessary to lift the abdominal wall so that the surgeon can work. The pain disappears in a few hours or at most 2-3 days.
Can I be diagnosed with endometriosis and actually have cancer?
In order to determine that there is an endometriosis, a differential diagnosis is made, that is to say, by means of different tests other possible alterations or illnesses that may present the same manifestation are ruled out. In the case of endometriosis, in order to confirm that the woman really has this pathology, it is essential to carry out a laparoscopy. By visualising the endometrial implants and analysing the tissue that makes them up by means of a biopsy, cancer or any other pathology can be safely ruled out.
If I have endometriosis, do I have to tell my doctor if I want to get pregnant?
Yes, the specialist will usually ask the patient about her reproductive desire and will want to know if she has already had offspring. She will take into account all the information obtained from the patient as well as her age to determine what type of treatment to follow, as some may affect the woman's reproductive capacity to a greater extent.
In any case, it will be recommended not to delay motherhood, as endometriosis is a chronic disease that can worsen with time.
Recommended reading
As we discussed in the article, laparoscopy is the most reliable diagnostic method for endometriosis. If you want more information about this intervention, we recommend you visit the following article: Endoscopy in gynecology: hysteroscopy and laparoscopy.
On the other hand, if you already have a clear diagnosis of endometriosis and want to know the possible therapeutic options, do not forget to visit this link: Treatment of endometriosis: can it be cured?
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Ahn SH, Singh V, Tayade C. Biomarkers in endometriosis: challenges and opportunities. Fertil Steril. 2017 Mar;107(3):523-532 (View)
American College of Obstetricians and Gynecologists (ACOG). Medical management of endometriosis. Washington (DC): American College of Obstetricians and Gynecologists (ACOG); 1999 Dec. 14 p. (ACOG practice bulletin; no. 11) (View)
ASRM American Society for Reproductive Medicine. Endometriosis. Guía para pacientes. En: Serie de Información para pacientes. Revisado en 2013. Birmingham, Alabama (View)
European Society for Human reproduction (ESHRE). Guideline for the diagnosis and treatment of endometriosis. Human Reproduction, 2005; 20(10):2698-2704 (View)
Giudice LC. Endometriosis. Clinical Practice. N Engl J Med 2010;362(25):2389-98 (View)
Vercellini P, Viganò P, Somigliana E, Fedele L. Endometriosis: pathogenesis and treatment. Nat Rev Endocrinol. 2014 May;10(5):261-75 (View)
FAQs from users: 'How is the diagnosis of endometriosis carried out?', 'If endometrial implants are found during laparoscopy, how are they removed?', 'Do diagnostic tests for endometriosis hurt?', 'Can I be diagnosed with endometriosis and actually have cancer?' and 'If I have endometriosis, do I have to tell my doctor if I want to get pregnant?'.
Authors and contributors

More information about Cristina Algarra Goosman





Hi, a couple of months ago I was told I had endometriosis and needed exploratory surgery because they didn’t look good on ultrasounds. I am very young and want to have children. What can I do?
Hello Lucy,
The reason you are going to have surgery is because the images are inconclusive, that is, they cannot give you a clear diagnosis without doing a scan.
The ability or not to have children may be affected by endometriosis but there is the treatment for it. Here is an article on the treatment of endometriosis: Treatment of endometriosis: can it be cured?
I advise you to talk to your doctors to tell them your concerns and once you have the operation done and a diagnosis in hand you can choose the treatment that best suits your characteristics.
I hope I have helped you.
Best regards.