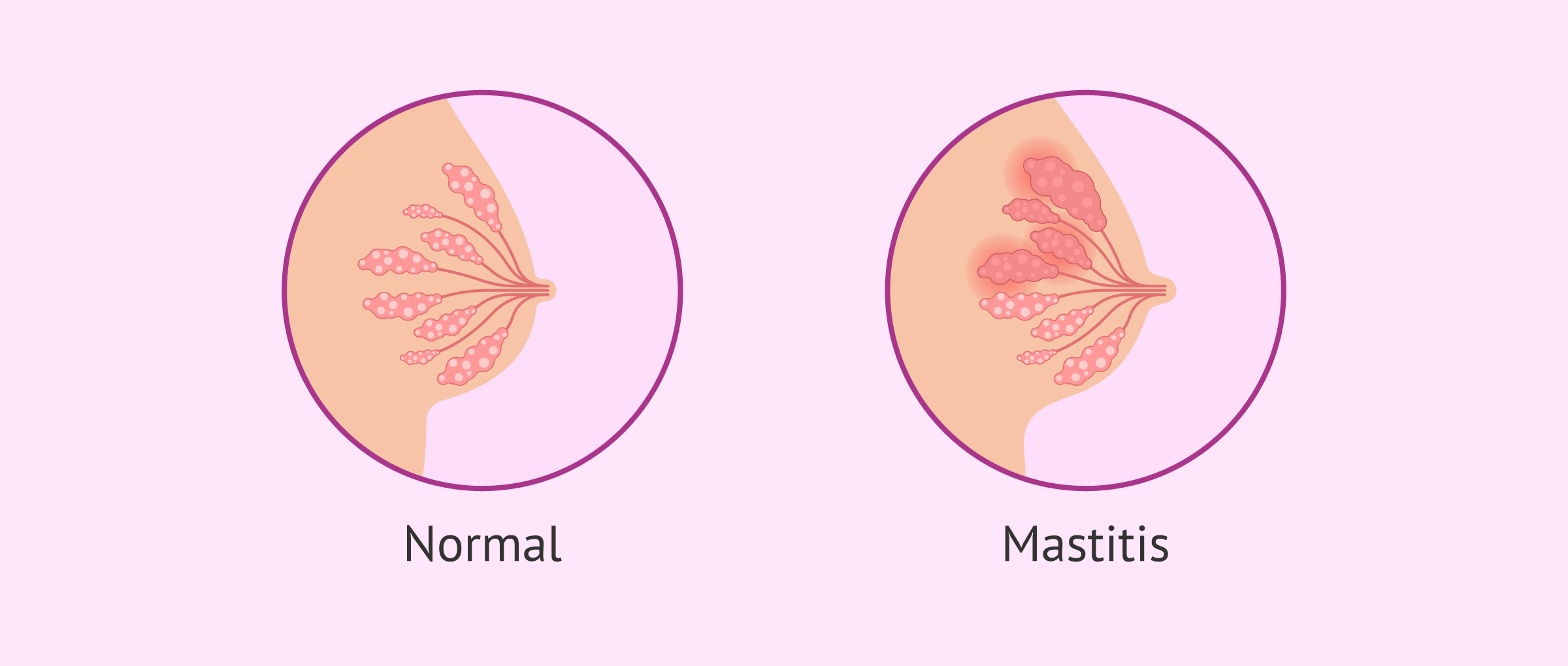
Mastitis is an inflammation of the mammary gland that may or may not be accompanied by infection. Normally, mastitis is associated with breastfeeding, which is why it is also referred to as lactational or puerperal mastitis.
However, breastfeeding is not the only cause of mastitis in women. There is also non-puerperal mastitis, which occurs for other reasons, though these are less common.
The most common clinical signs of mastitis include breast redness, breast swelling, and fever.
Provided below is an index with the 8 points we are going to expand on in this article.
- 1.
- 1.1.
- 2.
- 3.
- 4.
- 5.
- 5.1.
- 5.2.
- 5.3.
- 6.
- 7.
- 8.
Causes of Mastitis
Mastitis is the inflammation of breast tissue, which is generally caused by breastfeeding. Specifically, the primary cause of puerperal mastitis is milk stasis or duct obstruction. This blockage occurs when milk is not efficiently removed from the breast, which can happen due to what is known as engorgement or breast congestion.
Breast engorgement happens when the breast is full of both milk and tissue fluid. Venous and lymphatic drainage is obstructed, milk flow is blocked, and pressure in the milk ducts and alveoli increases. The breasts become swollen and edematous. This leads to excessive milk accumulation in the breasts, so the milk remains trapped inside and flows with great difficulty.
Another possible cause of mastitis during breastfeeding is an infection caused by bacteria entering the milk ducts through nipple wounds.
However, there are other non-puerperal causes that can lead to inflammation of the mammary glands, such as hormonal disorders, tobacco use, breast friction, etc.
Risk Factors for Mastitis
One of the main factors that predispose mothers to postpartum mastitis is latching. If the baby latches poorly during feeding, it can also cause cracks or fissures in the nipple. Due to the pain these cause, many women tend to avoid feeding from that breast, which can lead to mastitis.
There are other risk factors that can lead to mastitis, although none increase the risk of breast inflammation as much as poor breastfeeding technique. Some of these are listed below:
- Age: Some studies indicate that women aged 21 to 35 are more prone to developing mastitis than those under 21 and over 35.
- Previous mastitis: There is evidence that a first episode of mastitis predisposes to recurrence.
- Nutrition: Antioxidants such as vitamin E, vitamin A, and Selenium have been shown to reduce the risk of breast inflammation.
- Stress and fatigue.
- Working outside the home, as it can increase the time between feedings.
Autoimmune diseases, local trauma, or the use of certain medications can also increase the risk of mastitis. Ultimately, any situation that alters the mucous membranes can raise the risk of developing mastitis.
When Does Puerperal Mastitis Occur?
Inflammation of the breast tissue can occur at any time during the breastfeeding period, although it most commonly occurs in the first trimester postpartum, especially in the second and third weeks after childbirth.
Due to breast inflammation, pus can accumulate in the breast, forming what is called a breast abscess. This complication usually appears within the first 6 weeks after childbirth, although it can also occur later.
Symptoms of Breast Inflammation
The increase in prolactin production during pregnancy may be responsible for breast inflammation. The main signs and symptoms that suggest mastitis include:
- Fever.
- General discomfort and pain.
- Wedge-shaped hardening and redness of the breast area.
- Inflammation of one or both breasts. Unilateral mastitis is more common.
- Cracked nipples due to inadequate drainage.
Other clinical signs of puerperal mastitis may include fatigue and a sensation of heat in the breast.
Can Puerperal Mastitis Be Prevented?
Mastitis and breast abscess can largely be prevented if breastfeeding is properly guided from the beginning. The goal is to avoid situations that cause milk stasis and to effectively treat early symptoms like engorgement, blocked ducts, and nipple pain.
Generally, stopping breastfeeding due to mastitis is not recommended, as milk drainage can help reduce symptoms and prevent abscess formation.
With adequate guidance and clinical and emotional support, full recovery should be possible, and future breastfeeding should not be problematic. Therefore, the prognosis for mastitis is quite good, provided appropriate treatment is applied. Conversely, with poor support and guidance, one may lose the ability to breastfeed or develop chronic breast tissue inflammation.
FAQs from users
Are there any home remedies for breast pain during breastfeeding?
If breast pain during breastfeeding is due to cracked nipples, some recommended tips include:
- Spread a small amount of breast milk over the nipple after each feeding.
- Wash the breast with warm water after each feeding and dry thoroughly.
- Apply olive oil to the nipple using circular massages.
- Use a chamomile or aloe vera infusion on the nipple.
If the discomfort during breastfeeding is caused by a poor latch, it is advisable to change the breastfeeding position.
Cabbage leaves can also be useful in relieving symptoms during breastfeeding, as they help reduce breast pain and inflammation.
What treatment is applied when puerperal mastitis is due to infection?
If the cause of breast tissue inflammation is a bacterial infection, then the recommended treatment for mastitis is the administration of antibiotics. In this case, it is advisable to use an antibiotic that is resistant to β-lactamases if the causative agent is Staphylococcus aureus.
On the other hand, if the bacterium causing mastitis in the woman is gram-negative, then the best option is to use cephalexin or amoxicillin.
In any case, no medication should ever be administered without prior medical prescription.
How is mastitis due to lactation treated?
If mastitis is caused by an infection, the usual approach is to prescribe antibiotics for 10 days. In addition, the specialist may recommend certain pain relievers, such as paracetamol or ibuprofen, to relieve discomfort from breast swelling.
If mastitis is caused by a blocked milk duct, then the treatment will focus on improving milk drainage. To achieve this, it is necessary to follow a series of recommendations, such as changing the breastfeeding position and nursing the baby more frequently.
Recommended Reading
Also, if you're interested in knowing whether exclusive breastfeeding or formula feeding is better, then you'll want to continue reading here: Feeding your newborn baby - breastfeeding or formula feeding?
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Christina Krogerus, Erika Wernheden, Lone Bak Hansen. Mastitis] Ugeskr Laeger. 2019 Nov 18;181(47):V07190396.
Emily Wilson, Susannah L Woodd, Lenka Benova. Incidence of and Risk Factors for Lactational Mastitis: A Systematic Review. J Hum Lact. 2020 Nov;36(4):673-686. doi: 10.1177/0890334420907898. Epub 2020 Apr 14 (View)
Hannah W Kornfeld, Katrina B Mitchell. Management of idiopathic granulomatous mastitis in lactation: case report and review of the literature. Int Breastfeed J. 2021 Mar 4;16(1):23. doi: 10.1186/s13006-021-00370-8 (View)
Irena Zakarija-Grkovic, Fiona Stewart. Treatments for breast engorgement during lactation. Cochrane Database Syst Rev. 2020 Sep 18;9(9):CD006946. doi: 10.1002/14651858.CD006946.pub4 (View)
Jeanne P Spencer. Management of mastitis in breastfeeding women. Am Fam Physician. 2008 Sep 15;78(6):727-31 (View)
Lindeka Mangesi, Irena Zakarija-Grkovic. Treatments for breast engorgement during lactation. Cochrane Database Syst Rev. 2016 Jun 28;2016(6):CD006946 (View)
Lisa H Amir, Carmela Baeza, Jayne R Charlamb, Wendy Jones. Identifying the cause of breast and nipple pain during lactation. BMJ. 2021 Jul 13:374:n1628. doi: 10.1136/bmj.n1628 (View)
Melodie M. Blackmon, Hao Nguyen, Pinaki Mukherji. Acute Mastitis. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan.2023 Jul 21 (View)
Pamela Douglas. Re-thinking lactation-related nipple pain and damage. Womens Health (Lond). 2022 Jan-Dec:18:17455057221087865 (View)
FAQs from users: 'Are there any home remedies for breast pain during breastfeeding?', 'What treatment is applied when puerperal mastitis is due to infection?' and 'How is mastitis due to lactation treated?'.