Being a sperm donor involves voluntarily donating your sperm to people or couples who cannot conceive a child naturally.
Depending on the country in which the donation is made, it will either be anonymous or will have the possibility of presenting profiles. Normally sperm donors are compensated for the potential inconvenience caused, this compensation also varies from country to country.
Sperm donors undergo an evaluation process to check their health and eligibility for donation.
Provided below is an index with the 8 points we are going to expand on in this article.
- 1.
- 2.
- 3.
- 3.1.
- 4.
- 5.
- 5.1.
- 5.2.
- 5.3.
- 5.4.
- 5.5.
- 6.
- 7.
- 8.
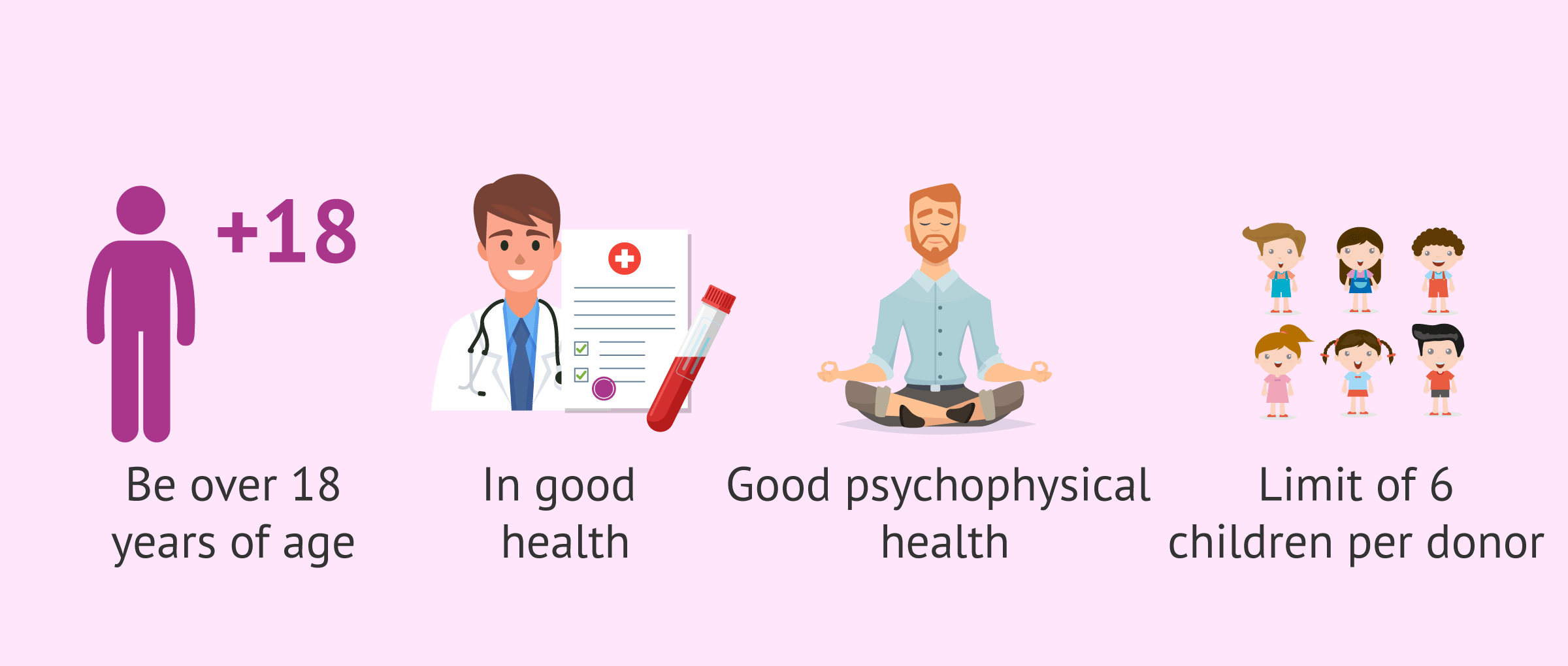
Requirements to be a sperm donor
The essential requirements to be a sperm donor are the following:
- Being over 18 years old: although legally the age limit for donating sperm is 50 years old, the reproduction clinics have reached an agreement, and only accept donors between 18 and 35 years old.< /li>
- Be in good health: candidates to be sperm donors undergo rigorous medical examinations to rule out possible genetic, hereditary or infectious diseases that could be transmitted.
- Be in good psychophysical health and in full use of mental faculties.
Should testing indicate the presence of or a risk factor for a hereditary disease, the donor will be qualified as ineligible. When selecting a potential donor, the first step involves an extensive evaluation of his health and a review of his family medical history.
The ASRM (American Society for Reproductive Medicine) and the FDA (Food and Drug Administration) recommend that both anonymous and directed donors go through the same testing process. Nevertheless, known donors are exempt from the six-month retesting requirement.
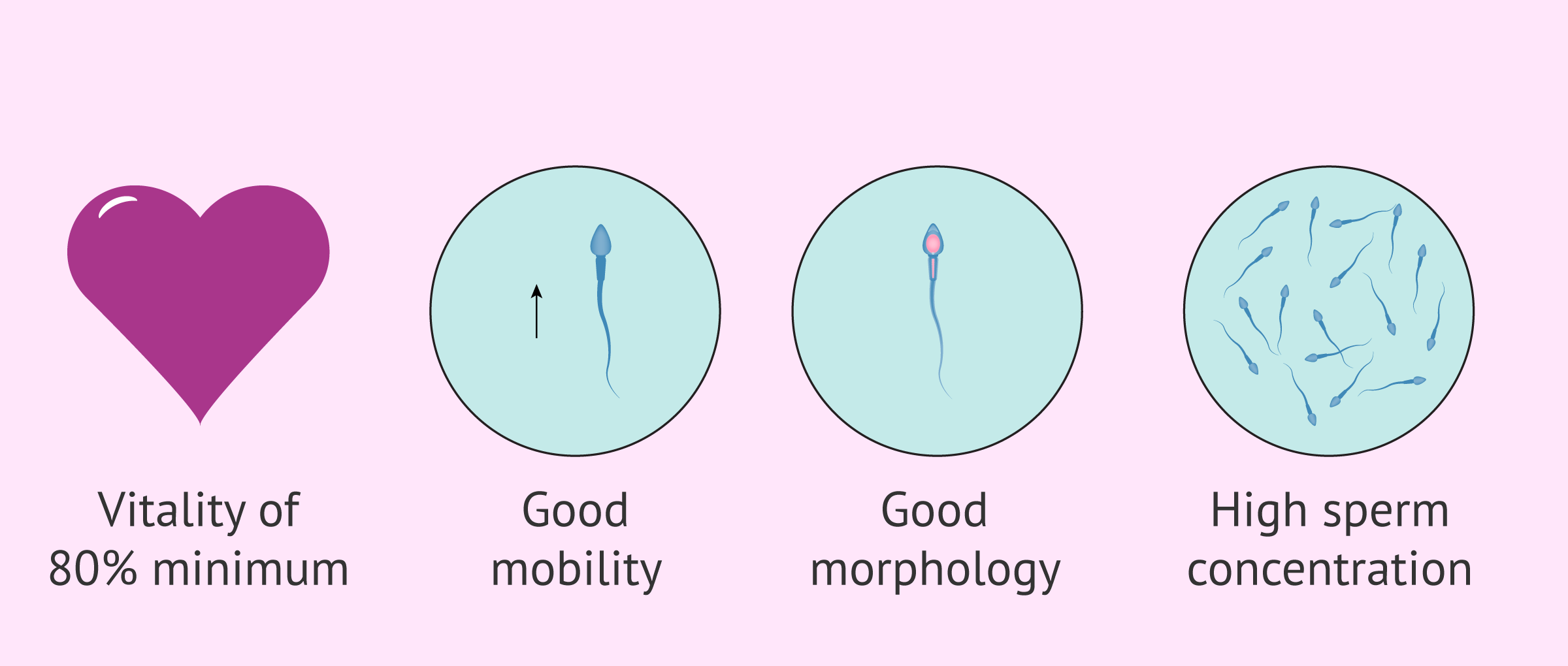
Semen quality
The required semen quality is very high. The possible donor must have a good volume of ejaculate, and exceptional seminal parameters:
- Spermatic vitality: vitality must be at least 80%.
- Good motility: with a very small percentage of immotile spermatozoa.
- Spermatic morphology must be good: oval head, intact midpiece and long, straight tail.
- High concentration of spermatozoa: which must be a concentration greater than 15 million spermatozoa, which is the reference value established by the WHO (World Health Organization ) as normal.
The donor semen sample also undergoes a freezing and thawing test, so it is essential that the vitality, motility, and concentration are well above the average values of the fertile population. These tests ensure that once the sample is thawed, despite the inevitable loss of sperm in the process, it still has a good concentration and quality for any assisted reproduction technique.
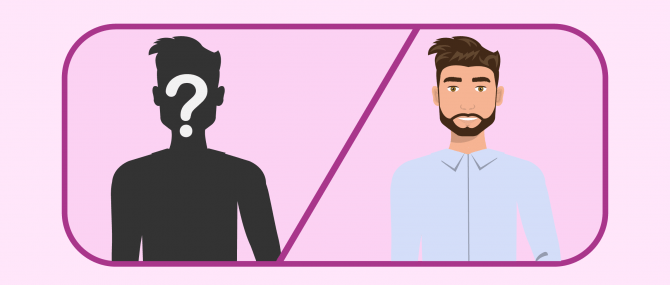
Anonymity or disclosure?
A sperm donor is a man who donates his sperm voluntarily to those who need it to create a family by means of Assisted Reproductive Technology (ART), either artificial insemination (AI) or in vitro fertilization (IVF).
From an international point of view, the profile of the donor can be anonymous or, conversely, known. The following are the basic differences between anonymous and known sperm donor profiles:
- Anonymous sperm donor: The identity of the donor will never be disclosed to the intended parents or the child. Patients should agree that they do not want to contact the donor in the future as well.
- Known sperm donor: The name, address, ID number, and other identifiable information about the donor will be released to the couple or person who requested his sperm cells. The identity will be disclosed to the child only when he or she turns 18.
Most European countries such as Spain, Greece, Croatia, the Czech Republic, and Ukraine require that potential sperm donors remain completely anonymous, with no option to be known in present or future time. However, in Denmark, the United States, and the United Kingdom, disclosure is allowed and covered by the law.
Some couples wish to select a donor based on his ethnicity or physical features (e.g. blue-eyed, with dimples, blonde or dark brown hair, etc.). In this sense, a known donor would be a good idea.
When it comes to being a known sperm donor, many patients turn to a friend, an acquaintance, or a family member to do so. However, this practice involves a series of cons and risks that should be taken into account.
Being a sperm donor for a friend
When a couple decides to use donor sperm, they have to face the decision between choosing an anonymous or a non-anonymous donor.
In these cases, some couples decide to ask a friend, sibling, family member, or acquaintance to be their sperm donor. Using a brother's sperm is common, as it is a way for the intended father to still share some percentage of DNA with the child, and therefore feel genetically connected to him.
If you agree to donate sperm for a friend or family member, you should take the following aspects into consideration:
- Even though you may have known them for a long time, you may not want to share information regarding your sexual lifestyle, which could put the baby at risk of catching a sexually transmitted disease (STD). There have been cases of donors who have lied on this matter.
- Becoming a private sperm donor takes more time than delivering it to a sperm bank, as donors should be medically pre-screened.
- If no legal contract is signed, and you do not want to contact the child in the future, things may change over time. This could damage not only your relationship but also affect the child's cognitive development.
For all the reasons listed above, both donors and intended parents are strongly recommended to sign a sperm donor agreement. This will make sure that, although the sperm donor is the biological father, he intends to waive all legal rights and responsibilities of fatherhood, including decisions on the child's health, visitation rights, and excludes the possibility of being liable for child support.
Average compensation payment
First, it should be clear that how much is paid per specimen varies from bank to bank. Nevertheless, the range is about $35-$50 per semen sample, which means sperm donors are not compensated in a one-time payment.
As explained earlier, sperm banks and fertility clinics require a six-month period between production and usage of the specimen. This quarantine period is required in order for viral infections such as HIV to be fully discarded. The pay is not released until the donor has been retested after the second set of blood tests.
In accordance with the HFEA guidelines, British fertility clinics are allowed to reimburse donors a fixed sum of £35 per sample collected and donated. It should be clear that this is done with the purpose of compensating the donor for any expenses he may have incurred.
The Law in the UK establishes that receipts must be provided for any out-of-pocket expenses that exceed this sum. Also, clinics often reimburse these expenses in two parts: half during the donor's visits to the clinic, and the remainder once the six-month quarantine period has finished and the samples have been cleared.
Similarly, the Spanish Law governing third-party reproduction has established an amount of €30-50 per specimen. It puts special emphasis on the fact that a sperm donation is an altruistic act, and therefore it is not paid, but compensation for the potential inconveniences and expenses derived from the process.
As for the United States, regulations are quite different from those established in Europe. Some sperm banks reimburse the donor's time and expenses with payments of up to $1,500/month, and can even be given periodic incentives such as gift certificates, among others.
FAQs from users
Is it possible to revoke a gamete donation contract?
A donor can demand the gametes he/she has donated for his/her personal use as long as they are available at the time of revocation. In this case, the donor is obliged to return all expenses incurred at the center.
Do I have to take any medication to be able to donate sperm?
No, to be a sperm donor you do not need to take any medication, you just need to be healthy and meet the parameters of semen quality. Unlike what happens with egg donors, sperm donors are not given medication to stimulate sperm production.
If I am not chosen as a donor because of the quality of my sperm, does that mean I have poor quality?
No, sperm donors require sperm of a higher quality than the quality needed to achieve a pregnancy naturally. Many sperm donor candidates are rejected, yet have no problem conceiving.
Can you be a sperm donor with HIV, HPV or herpes?
No, these are STDs for which a potential sperm donor would be ineligible. A history of genital herpes or warts is a cause of exclusion.
Normally, health care professionals interview donor candidates with regard to behavior that could have exposed him to STDs, including history of homosexuality, bisexuality, multiple sex partners, a recent stay in a geographical region with high incidence of HIV, etc.
What are the potential risks of donating sperm?
There are no health risks associated with sperm donation. The only potential risks derived from sperm donation are linked to donors who donate their semen too many times, as there is the risk that the children born as a result of his donations end up meeting and procreating in the future.
Recommended readings
If you are thinking of undergoing assisted reproduction treatment and need to know in more detail what donor sperm treatments consist of, you may be interested in the following article: Using a sperm donor to get pregnant - How does the process work?
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
McGovern, P. G., & Schlaff, W. D. (2018). Sperm donor anonymity: a concept rendered obsolete by modern technology. Fertility and sterility, 109(2), 230-231.
Cohen, G., Coan, T., Ottey, M., & Boyd, C. (2016). Sperm donor anonymity and compensation: an experiment with American sperm donors. Journal of Law and the Biosciences, 3(3), 468-488.
Harper, J. C., Kennett, D., & Reisel, D. (2016). The end of donor anonymity: how genetic testing is likely to drive anonymous gamete donation out of business. Human Reproduction, 31(6), 1135-1140.
Kalampalikis, N., Doumergue, M., Zadeh, S., & of CECOS, F. F. (2018). Sperm donor regulation and disclosure intentions: Results from a nationwide multi-centre study in France. Reproductive Biomedicine & Society Online, 5, 38-45.
FAQs from users: 'Why be a sperm donor? Is it worth it?', 'Is it possible to revoke a gamete donation contract?', 'Do I have to take any medication to be able to donate sperm?', 'How can you become a "natural" sperm donor?', 'If I am not chosen as a donor because of the quality of my sperm, does that mean I have poor quality?', 'What is the difference between being a sperm bank donor and a private sperm donor?', 'How difficult is it to become a sperm donor and how does it feel?', 'Can you be a sperm donor if you are gay?', 'Can you be a sperm donor with HIV, HPV or herpes?' and 'What are the potential risks of donating sperm?'.
Authors and contributors

More information about Cristina Algarra Goosman



Hello, do I have to take all the medical and psychological tests that are required? I understand the physical ones but the psychological ones?
Hi Chris,
Semen quality is just as important as the genetic load that accompanies it, which is why psychosocial testing evaluates not only current physical conditions but genetic loads for both physical and mental illnesses.
This is done to ensure the quality of the sample so that patients who need it can be certain that a donor is a healthy person in all aspects of his life.
I hope I have solved your doubt,
Best regards
I was refused the donation but I have two children of my own so my sperm is of good quality, they didn’t tell me why.
Hi Sam,
Most clinics have certain standards to accept sperm donation, this must meet certain parameters which do not mean that out of them the donor can beget children naturally but that does not reach the minimum established by the clinic that is usually of optimal quality (higher than what is established by WHO as normal).
I hope I have helped you,
Best regards