The epidural is a type of anesthesia known worldwide for its advantage in providing a painless delivery, whether during vaginal delivery or a Cesarean section.
In addition, the epidural is one of the safest forms of anesthesia with fewer side effects for the woman who has just given birth.
However, not all pregnant women defend it, as they believe that pain is something that should be felt during birth and helps to forge the bond between mother and baby.
Provided below is an index with the 8 points we are going to expand on in this article.
- 1.
- 1.1.
- 1.2.
- 2.
- 3.
- 3.1.
- 3.2.
- 4.
- 5.
- 5.1.
- 5.2.
- 5.3.
- 5.4.
- 5.5.
- 5.6.
- 6.
- 7.
- 8.
What is an epidural?
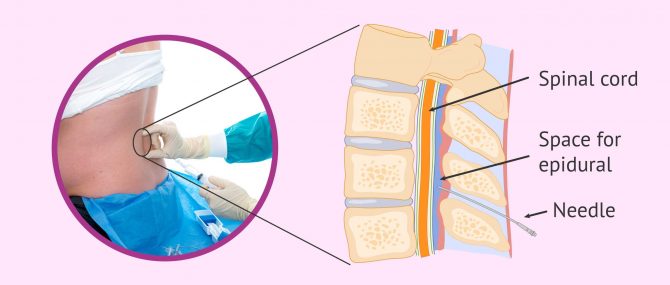
Epidural anesthesia, also known as peridural anesthesia, involves the introduction of a local anesthetic into the epidural space so that the nerve endings are blocked at the level of the bone marrow.
The effect of the epidural, therefore, takes place in the lower body. However, the person is not asleep as in the case of general anesthesia but remains conscious at all times.
The effect of this anesthesia varies depending on the dose administered: in small doses it eliminates pain and in large doses, it can produce a muscle block and paralysis.
Besides, its duration will also depend on the dose, as it can last from 15 minutes to 2 hours.
Indications
The epidural is indicated for abdominal operations, especially at the infra-umbical level, such as childbirth, inguinal hernias, operations on the bladder or testicles, etc.
Today, the epidural is the method preferred by pregnant women to give birth, because it allows them to enjoy the arrival of their child with all the sensations, but without feeling pain.
How and where is it placed?
For the administration of the epidural anesthesia, a very thin catheter is used which is introduced into the lumbar area of the spine (between the two lumbar vertebrae) and then into the area covering the spinal cord.
The woman's position at the time of the injection should be seated or lying on her side, with her back arched and her head tilted forward.
Prior to the epidural puncture, a gynecologist-midwife must ensure that the woman who is about to give birth is dilated, as she must be at least 2 centimeters dilated. It is also important that the dilation does not exceed 8 centimeters, since the risk of complications in this advanced phase is greater.
Once introduced, the epidural anesthesia takes effect gradually and in about 10-15 minutes the woman already feels pain relief.
Types of epidural
In addition to the epidural anesthesia that we have already discussed, there are other types of epidurals that can be used depending on how the delivery is going:
- Walking epidural
- reduces and controls pain, but does not prevent leg movement. Therefore, the woman can walk, participate more actively in the birth and feel everything that happens in her body.
- Combined epidural/spinal anesthesia
- consists of a combination of both anesthetics to provide a much faster effect. Spinal anesthesia is one that is inserted directly into the spinal fluid and is used when a woman is in very active labor or to perform a cesarean section.
Today, both medical specialists and pregnant women are increasingly advocating the establishment of protocols to enable them to enjoy a meaningful childbirth without pain and to reduce instrumental deliveries as much as possible.
The use of the epidural
Although epidural anesthesia is currently used in almost 90% of deliveries, it is necessary to know that it has both advantages and disadvantages.
The woman must know all the aspects related to her before choosing the way she is going to give birth and decide if she wants an epidural.
Advantages
Remaining conscious throughout the birth is the main advantage of the epidural. That's why she's so in demand by pregnant women who are about to give birth.
In addition, this type of anesthesia has multiple other advantages that we discuss below:
- It allows the woman to actively participate in the arrival of her child, as it relieves the pain completely without blocking any of the mental faculties.
- It is possible to adjust the dose of anesthetic to be stronger in case of pain or to make its effect disappear as the expulsive phase approaches so that the woman can fully control this last moment.
- The woman feels all the contractions as pressure, but no pain.
- The epidural tends to slow down labor, which can be helpful.
- It avoids the need for another anesthetic if forceps, vacuum or episiotomy are required.
- The epidural improves the baby's oxygen supply.
- It reduces the strain on a woman's lungs and heart during childbirth, which is beneficial for those with lung or heart conditions.
- Anxiety and fear that many women have about giving birth because of pain is reduced.
- There may be cases where it is not effective.
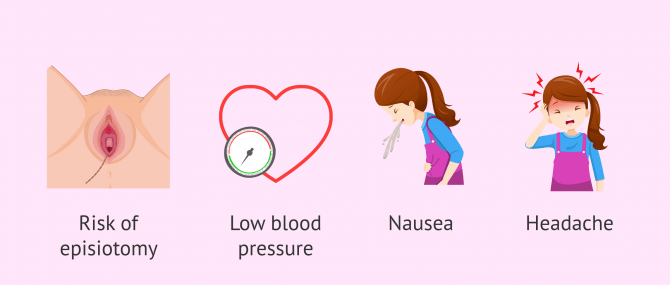
- The epidural causes a loss of muscle strength, so the second stage of labor is slower and the mother relies on the midwife's instructions to know when to push.
- There is an increased risk of episiotomy and use of forceps, as the woman loses the ability to push.
- Risk of having a rapid fall in blood pressure. In order to avoid this, it is necessary to keep the woman well hydrated through an intravenous drip.
- Epidurals have the following side effects: headache, dizziness, nausea, loss of bladder sensation, pain at the puncture site, etc.
- Obese patients.
- Patients with heart disease.
- Patients with blood clotting problems.
- Patients with lumbar hernias.
- Patients with lower back tattoos.
- Excessively advanced dilation at the time of delivery (more than 8 or 9 cm).
Therefore, the epidural offers very high safety for both mother and baby, so the risk of complications is minimal. Additionally, in the event of having to switch from a vaginal delivery to a C-section, the woman will already be anesthetized if the epidural has been used.
Disadvantages
The epidural also has a number of disadvantages or risks, such as the following:
However, there are multiple studies on this subject and all of them conclude that epidural anesthesia is safe for both mother and child. For this reason, the likelihood of complications in childbirth is minimal.
When is an epidural contraindicated?
Once the advantages and disadvantages of epidural anesthesia are known, the pregnant woman can choose whether or not to have it for delivery and this should be stated in her birth plan.
To make this decision, it is also important to follow the medical advice of the gynecologist and/or midwife who has monitored the pregnancy and to take into account the conditions of each individual case.
It should be noted that this decision can be changed at the time of delivery, i.e. if the woman has previously decided not to have an epidural but finally changes her mind, either because of the intense pain of childbirth or because the doctor recommends doing so out of necessity.
On the other hand, there are some specific circumstances in which epidural is contraindicated and cannot be administered. Some of these situations are listed below:
In any case, it is recommended to analyze each patient individually and personally. In addition, it's essential to follow the advice of the doctors.
FAQs from users
How is the childbirth with the walking epidural?
Walking epidurals have been a great advance in the field of analgesia during the birth process. It is a safe technique that allows for birth with less pain and in which the woman can participate actively, in all its phases, as long as the pain is adequately controlled.
Read more
What is a walking epidural?
The walking epidural or ambulatory epidural is a type of anesthesia that allows control of labor pains, but without paralyzing the woman from the waist down. This is achieved by decreasing the dose of anesthesia and increasing the dose of opiates so that only the sensory fibers fall asleep and the motor fibers remain awake.
Therefore, the woman can move her legs and even walk during labor to the expulsive phase. This helps the woman to participate more actively in the arrival of her child into the world and to enjoy this moment much more.
Does epidural anesthesia hurt?
The injection to put the epidural anesthesia or the catheter with the anesthesia may be a little uncomfortable, but it does not hurt. Usually, the anesthesiologist puts some anesthetic first on the skin of the area so that the woman does not feel the introduction of the larger needle.
Some women may feel the needle stick more than others, but in principle the epidural anesthesia does not hurt. What is important is that the woman be completely still so that the anesthesiologist can make the puncture without any complications.
Is epidural anesthesia also used in case of C-section?
Yes, although a combination of epidural and spinal anesthesia is usually used, since the latter has a much faster effect when introduced directly into the spinal fluid. Furthermore, it is not necessary to puncture the woman twice, since with the same puncture both types of anesthesia can be introduced.
The woman will be conscious at all times, but will be paralyzed from the navel down for approximately 2 hours.
What do you feel during delivery with an epidural?
After the epidural is placed in the dilation phase of labor, the woman gradually feels relief from the pain. After 15-20 minutes, the epidural has taken effect and the woman feels no pain at all.
On the other hand, the woman does have sensations and can feel the contractions as pressure. She may also notice that the baby slips through the birth canal until it is expelled, but she does not feel pain in the walls of the vagina. All of this will depend on the dose of anesthesia, which can be regulated at different times during the delivery.
What are the benefits of epidural anesthesia?
Epidural anesthesia is a fairly safe type of analgesia for both mother and baby. There are many benefits attributed to the epidural.
The epidural promotes the dilation of the cervix, which results in a faster delivery. In addition, it reduces stress during delivery and has no effect on breast milk.
Thanks to epidural anesthesia, women will not feel pain and will be able to actively participate in labor. This gives patients more peace of mind, since many are afraid of the moment of delivery because of the pain it may cause.
Suggested for you
After reading this article you may be interested in reading about childbirth in detail. To do so, you can access the following article: Labor & Birth - How Is a Baby Delivered?
Throughout the pregnancy, it is also very important to prepare for the time of delivery so that it can take place with as few complications as possible. For more information on this, we recommend reading the following article: Childbirth Preparation Classes: Preparing for Delivery.
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Fernández-Campos FJ, Escrivá D, Palanca JM, Ridocci F, Barrios C, Gallego J. Women's acute anxiety variations before and after epidural anesthesia for childbirth. J Psychosom Obstet Gynaecol. 2017 Jun;38(2):152-158.
Jepsen I, Keller KD. The experience of giving birth with epidural analgesia. Women Birth. 2014 Jun;27(2):98-103.
Ministerio de Sanidad y Política Social. Guía de Práctica Clínica sobre la Atención al Parto Normal. Vitoria-Gasteiz, 2010. (ver)
FAQs from users: 'How is the childbirth with the walking epidural?', 'What is a walking epidural?', 'Does epidural anesthesia hurt?', 'Is epidural anesthesia also used in case of C-section?', 'What do you feel during delivery with an epidural?' and 'What are the benefits of epidural anesthesia?'.