Newborn jaundice is the name given to the yellowish tint that many babies' skin may take on. Although it can be frightening for parents, it usually disappears without treatment after about 2 weeks.
However, monitoring jaundice and its evolution is of great importance, because if it is severe and untreated, it can lead to serious problems and complications such as brain damage. Therefore, early diagnosis and appropriate treatment is paramount.
Provided below is an index with the 9 points we are going to expand on in this article.
- 1.
- 2.
- 3.
- 4.
- 5.
- 6.
- 6.1.
- 6.2.
- 6.3.
- 7.
- 8.
- 9.
What is jaundice in the newborn?
Jaundice in the newborn is the yellowish tint that the skin and even the whites of the eyes (sclera) may take on in the first days of the baby's life. This yellowish coloration arises as a consequence of elevated bilirubin levels in the blood (hyperbilirubinemia).
Bilurrubin is a yellowish pigment produced by the body in the normal breakdown process of red blood cells. The liver is the organ that facilitates the elimination of bilirubin in the feces.
While the baby is developing inside the mother's womb, the mother's liver is responsible for eliminating fetal bilirubin. However, after birth, the baby may have somewhat elevated bilirubin levels for a few days until its own liver is ready and begins to eliminate it properly.
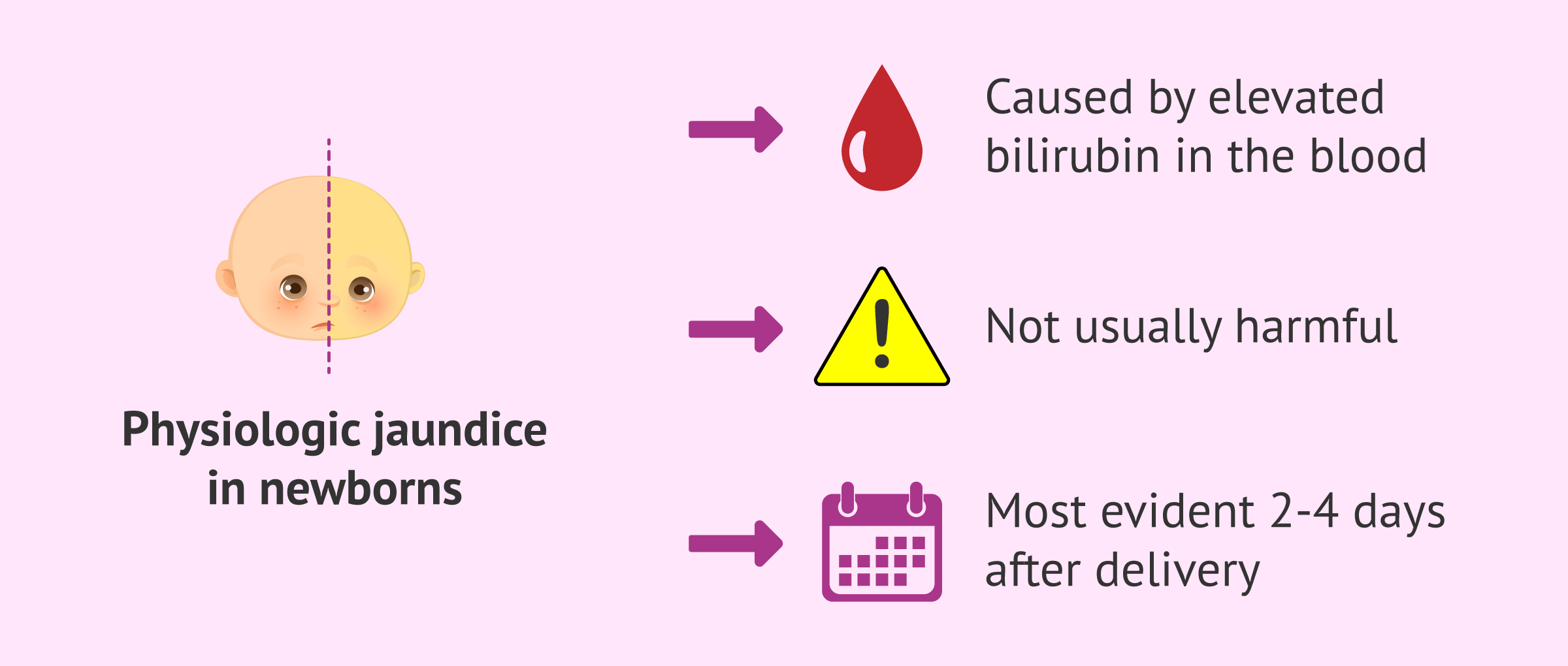
This produces mild jaundice, known as physiological jaundice physiologic jaundicethis is present in most infants and is usually not harmful. This type of jaundice is most evident 2-4 days after delivery and may last about 2 weeks until it disappears on its own.
Symptoms
Among the main symptoms of jaundice in the infant is yellowing of the skin and eyes. The appearance of the yellow color most commonly begins on the face, but may continue to spread to the chest, abdomen, arms and legs of the newborn.
However, the baby may suffer brain damage (kernicterus) if bilirubin levels rise too high. Therefore, it will be very important to monitor the jaundiced baby to avoid this situation. Call your health care provider as soon as possible if your baby has any of the following symptoms:
- More intense jaundice, which worsens or spreads.
- Drowsiness, lethargy.
- Poor appetite, problems eating well and gaining weight.
- Irritability, the baby is upset.
- Intense, high-pitched crying.
- Body arched backwards.
This will allow the baby to receive the most appropriate treatment and thus prevent the development of serious complications.
Possible causes
To discuss the possible causes of jaundice in the newborn, it is important to distinguish whether it is physiological jaundice or a more severe type of jaundice.
Physiologic jaundice is the most common jaundice in newborns and does not usually represent a serious problem. Its main cause is the immaturity of the baby's liver, which makes the elimination of bilirubin not as effective. As a result, the blood concentration of bilirubin may be elevated, resulting in a yellowish skin tone.
In addition, the half-life of red blood cells is shorter in newborns than in adults, i.e., they "live" less time, which increases bilirubin production.
However, there may be other factors that make jaundice more severe. Among the main ones are:
- Premature delivery. The greater hepatic immaturity makes bilirubin elimination even less efficient than if the baby is born at term. On the other hand, the premature infant may eat less, which makes it more difficult to eliminate bilirubin in the stool because there are fewer bowel movements.
- Hematomas. They may occur if delivery has been complicated and may increase bilirubin levels due to increased red blood cell degradation.
- Blood incompatibility between mother and baby, since maternal antibodies could attack the baby's red blood cells and cause their degradation.
- Breastfeeding Especially when breastfeeding is not going well and the baby is not sufficiently nourished and hydrated.
In addition, there may be other causes of jaundice, such as internal bleeding, infection, liver failure or other disorders. If any of these other causes occur, jaundice usually appears earlier or later than physiological jaundice and may be more severe, so it will be important to detect it early to avoid complications.
Diagnosis
To diagnose jaundice, the specialist can look at the baby's appearance. To detect yellowish skin color, especially in darker-skinned infants, you may press lightly on the newborn's nose or forehead and observe the skin color immediately after removing the pressure.
However, before the infant is discharged from the hospital, a skin test (with a sensor) or blood test should have been performed to assess the infant's bilirubin levels.
In the event that a skin test is performed and the result is elevated, it must be confirmed with a blood test.
On the other hand, certain additional tests may be done on the baby if jaundice-causing pathology is suspected.
Treatment
Treatment of jaundice in the infant will depend on the cause and severity. If it is physiological jaundice, it usually disappears without treatment in about 2 weeks. If this is not the case, a specialist should be consulted.
However, if the baby needs treatment, it may consist of:
- Increase food. The specialist may recommend more frequent feedings or supplementation to avoid dehydration and to promote the elimination of bilirubin in the stool.
- Phototherapy or light therapy. The newborn will remain under a special light without clothing (only a diaper and eye protection). The skin is exposed to light and this makes it easier for bilirubin to be eliminated from the body.
- Exchange transfusion. If phototherapy does not work, in more severe cases, an exchange transfusion is performed to replace the baby's blood, thus decreasing the bilirubin concentration.
However, depending on the cause, other treatments may be necessary to lower blood bilirubin levels.
FAQs from users
What are the possible complications of jaundice in the newborn?
The main and most serious complication of neonatal jaundice is kernicterus or nuclear jaundice, a brain damage that can occur if bilirubin levels in the infant are very high and untreated.
Kernicterus can lead to athetoid cerebral palsy and disturbances in vision, hearing and teeth.
Therefore, it is important to detect jaundice in the infant and to monitor the baby's progress by controlling the bilirubin levels in the blood to avoid this type of serious complication.
Are there any natural remedies for jaundice in infants?
If the jaundice is not severe, the specialist may recommend that the mother simply breastfeed the baby more frequently. This will cause the baby to pass more stool, which will cause the baby to eliminate more bilirubin with the stool.
However, jaundice can cause serious complications in the baby (brain damage) if bilirubin levels remain elevated without treatment.
Therefore, to avoid the appearance of these complications, it is best to follow the recommendations of the specialist regarding the frequency of feedings and the treatment considered necessary depending on the severity, symptoms and bilirubin levels in the baby's blood, since on more serious occasions this natural remedy will not be sufficient.
Is it good to put the newborn in the sun to cure jaundice?
No, exposing the newborn baby to the sun to try to reduce jaundice and make it disappear as soon as possible should not be done, as it is not safe.
Always follow the recommendations of the specialist and go to the established controls to avoid possible serious complications of neonatal jaundice.
Suggested for you
If you want to read more about Rh incompatibility between mother and baby, you can access the following article: Maternal isoimmunization due to Rh incompatibility, what are the risks?
On the other hand, if you want to know more about preterm labor, we recommend you to visit this link: What causes preterm labor - Risks, causes and symptoms.
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Gao C, Guo Y, Huang M, He J, Qiu X. Breast Milk Constituents and the Development of Breast Milk Jaundice in Neonates: A Systematic Review. Nutrients. 2023 May 10;15(10):2261. doi: 10.3390/nu15102261. PMID: 37242142; PMCID: PMC10224501. (View)
Gottimukkala SB, Lobo L, Gautham KS, Bolisetty S, Fiander M, Schindler T. Intermittent phototherapy versus continuous phototherapy for neonatal jaundice. Cochrane Database Syst Rev. 2023 Mar 2;3(3):CD008168. doi: 10.1002/14651858.CD008168.pub2. PMID: 36867730; PMCID: PMC9979775. (View)
Hegyi T, Kleinfeld A. Neonatal hyperbilirubinemia and the role of unbound bilirubin. J Matern Fetal Neonatal Med. 2022 Dec;35(25):9201-9207. doi: 10.1080/14767058.2021.2021177. Epub 2021 Dec 26. PMID: 34957902. (View)
Itoh S, Okada H, Koyano K, Nakamura S, Konishi Y, Iwase T, Kusaka T. Fetal and neonatal bilirubin metabolism. Front Pediatr. 2023 Feb 7;10:1002408. doi: 10.3389/fped.2022.1002408. PMID: 36824297; PMCID: PMC9941200. (View)
Okwundu CI, Olowoyeye A, Uthman OA, Smith J, Wiysonge CS, Bhutani VK, Fiander M, Gautham KS. Transcutaneous bilirubinometry versus total serum bilirubin measurement for newborns. Cochrane Database Syst Rev. 2023 May 9;5(5):CD012660. doi: 10.1002/14651858.CD012660.pub2. PMID: 37158489; PMCID: PMC10167941. (View)
Thomas M, Greaves RF, Tingay DG, Loh TP, Ignjatovic V, Newall F, Oeum M, Tran MTC, Rajapaksa AE. Current and emerging technologies for the timely screening and diagnosis of neonatal jaundice. Crit Rev Clin Lab Sci. 2022 Aug;59(5):332-352. doi: 10.1080/10408363.2022.2038074. Epub 2022 Feb 21. PMID: 35188857. (View)
FAQs from users: 'What are the possible complications of jaundice in the newborn?', 'Are there any natural remedies for jaundice in infants?' and 'Is it good to put the newborn in the sun to cure jaundice?'.