Combined first-trimester screening, also known as triple screening, is a non-invasive prenatal test that consists of performing an ultrasound and a blood test on the pregnant woman to rule out possible chromosomal abnormalities.
As its name suggests, this test should be done around week 12 of pregnancy, i.e. at the end of the first trimester for its result to be reliable.
One of its main advantages is that it has reduced the number of amniocentesis and chorionic biopsies in pregnant women, which are invasive tests.
Provided below is an index with the 7 points we are going to expand on in this article.
- 1.
- 1.1.
- 1.2.
- 1.3.
- 2.
- 3.
- 4.
- 4.1.
- 4.2.
- 4.3.
- 4.4.
- 5.
- 6.
- 7.
What is triple screening?
Triple screening is a combined test whose objective is to estimate the risk of pregnancy for congenital anomalies and/or fetal chromosomopathies.
It is important to note this, as it is not a definitive diagnostic test. In case of an altered result in the triple screening, the woman will have to undergo other invasive prenatal tests, such as amniocentesis, to confirm whether the fetus is completely healthy or not.
How is it done?
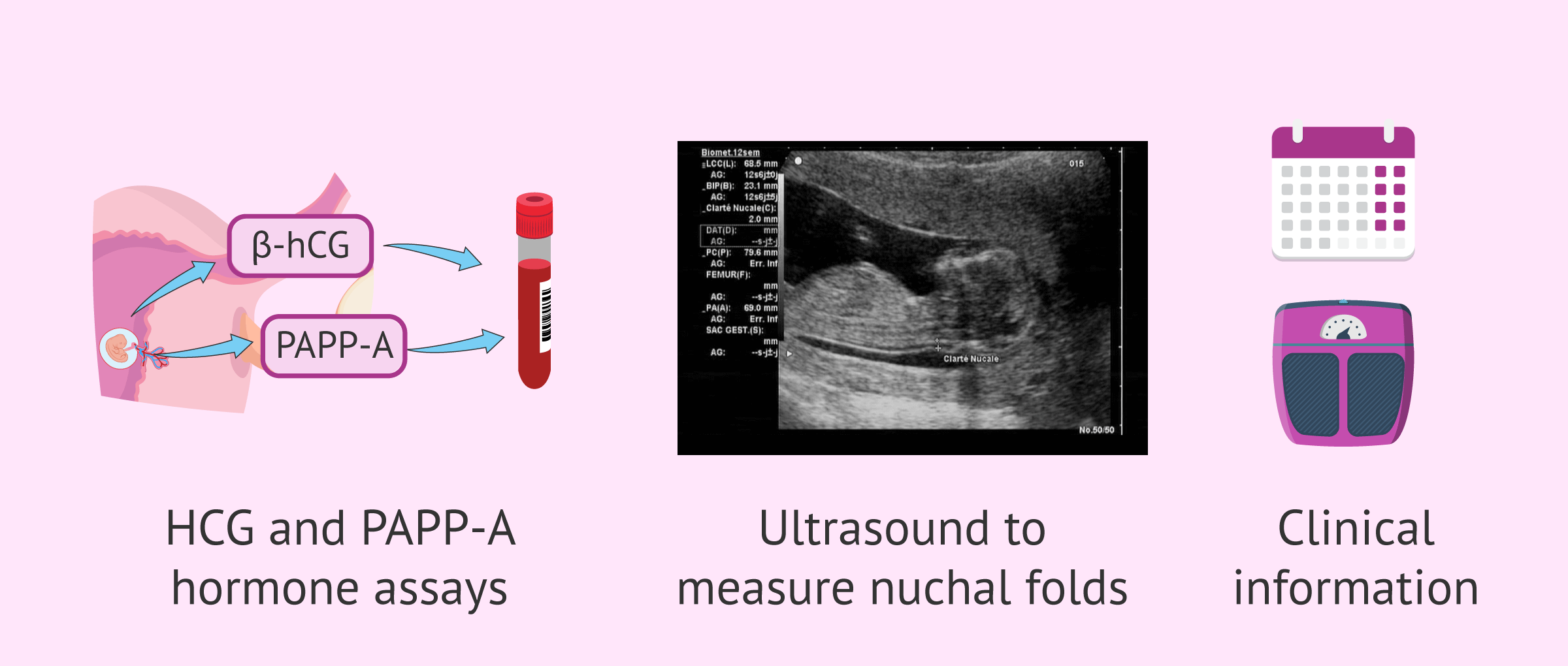
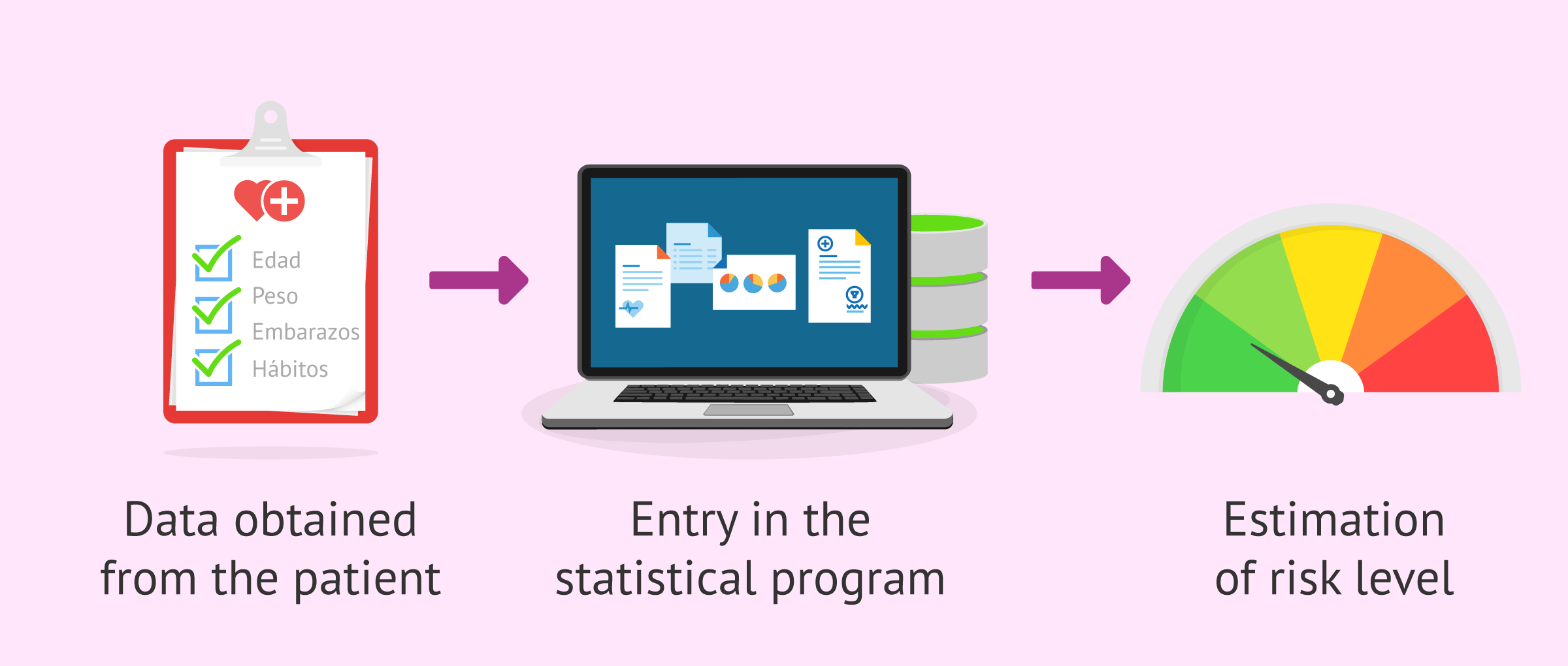
To calculate the probability of risk in the triple screening, a statistical software program relates different biochemical and ultrasound parameters together with other clinical data of the pregnant woman.
This information is obtained from the following tests:
- Blood tests
- values of pregnancy-associated placental protein (PAPP-A) and free beta-hCG hormone are determined.
- Ultrasound
- the fetal nuchal fold or nuchal translucency (NT) is measured.
- Clinical information
- mother's weight, age, number of fetuses, weeks of pregnancy, etc.
The detection rate of combined first trimester screening is about 75%, with a false positive rate of about 3%. This means that some of the cases that obtain a high probability of risk of suffering some alteration are in fact erroneous and correspond to healthy babies.
Even so, it is worth doing this test in order to rule out chromosomal pathologies and, in the worst case, to be able to decide whether to terminate the pregnancy when the baby is going to be born with a disease.
When is it done?
First trimester combined screening should be offered to all pregnant women presenting for prenatal care before 14 weeks of pregnancy.
In general, tests to estimate the combined clinical-biochemical-echographic risk are performed between 8 and 13 weeks of pregnancy in one of the following ways:
- Combined screening in one time
- the ultrasound assessment and blood collection is done on the same day, which can be between 11 and 13+6 weeks of pregnancy.
- Two-stage combined screening
- blood collection can be done at any time between 8 and 13+6 weeks of pregnancy, but ultrasound is important to perform between 11 and 13+6 weeks of pregnancy.
The way the tests are performed is indifferent and depends mainly on the number of times the pregnant woman goes to the office.
If the first prenatal visit takes place before the 8th week of pregnancy, then the combined screening can be scheduled in two stages and the first blood test can be used to determine biochemical markers together with serologies and blood grouping.
Results
As we have already indicated, the result of the triple screening is not a definitive diagnosis, but an estimate made by a statistical program of the risk that the fetus has of suffering chromosomal diseases or other congenital defects.
The specific software calculates the risk index (IR) from all the parameters entered, the interpretation of which is as follows:
- IR > 1 in 250
- there is a high risk that the fetus will have trisomy 21 (Down syndrome).
- IR > 1 in 100
- there is a high risk of the fetus having trisomy 18 (Edwards' syndrome).
In the event of a high-risk pregnancy, the gynecologist should offer the pregnant woman a more reliable invasive technique, such as chorionic villus sampling or amniocentesis.
If the risk obtained is medium or low, the woman can also undergo a fetal DNA test in maternal blood, which is non-invasive and serves to detect pathologies such as Down syndrome, Edwards' syndrome, or Patau's syndrome.
Second trimester biochemical screening
Although combined screening should ideally be done in the first trimester, pregnant women who have been seen after 14 weeks of gestation can have a biochemical screening if they are between 14 and 17 weeks of pregnancy.
There are 3 types of second-trimester biochemical screening:
- Double test
- is based on the quantification of 2 biochemical markers: alpha fetoprotein (AFP) and beta-hCG. Its detection rate is 60%.
- Triple test
- the markers AFP, beta-hCG and also estriol (E3) are quantified here. Its detection rate is 60%.
- Quadruple test
- consists of the quantification of 4 biochemical markers: AFP, beta-hCG, E3 and inhibin A. Its detection rate is 75%.
These tests are also indicative of possible structural abnormalities in the fetus, such as neural tube closure defects. For example, elevated AFP levels may indicate the presence of spina bifida or anencephaly in the fetus.
Advantages of triple screening
The main advantage of triple screening is that it is a non-invasive test that is easy to perform in all pregnant women, which has made it possible to reduce the number of invasive tests performed, which have a small risk for the fetus and could cause a miscarriage.
In the past, amniocentesis was a prenatal test performed on all pregnant women over 35 years of age. However, it is now no longer essential if a low-risk index has been obtained in the first trimester combined screening.
In addition, the fact that this combined screening can be performed in all pregnant women regardless of their age makes it possible to detect high-risk pregnancies that would otherwise have been overlooked.
Both women over 35 and younger women can have children with chromosomal abnormalities, so there is a real need for universal screening of pregnant women.
Another advantage of triple screening is that the results are obtained quickly, within a week at most. In fact, if the woman has previously undergone the blood test (combined two-stage screening), the results of the triple screening after the ultrasound can be obtained immediately.
Thanks to this advantage, expectant parents can be informed in sufficient time so that, in case of poor results, they can make the decision to perform a more reliable invasive test and, in the worst case, to terminate the pregnancy if the baby comes with congenital defects or chromosomal alterations.
Voluntary termination of pregnancy is legal in Spain until the 22nd week of gestation if the fetus presents serious anomalies and/or incurable diseases (Organic Law 2/2010).
FAQs from users
Is triple screening done in all pregnancies and is it reliable?
Triple screening is done to all pregnant women nationwide, both in the public and private health system. It is usually done in the 10th week of pregnancy.
It is a statistical computer program that combines ultrasound data with biochemical data (BHCG and PAPP-A) and patient data (age, smoking).
It provides the pregnant woman with a statistical value that informs of a risk. It has a sensitivity of 80 to 85%.
What is fetal nuchal translucency?
Nuchal translucency (NT) or nuchal fold is an accumulation of fluid seen by ultrasound under the skin at the nape of the fetus' neck, i.e. at the back of the neck.
The thickness of the nuchal translucency is the best ultrasound marker of fetal aneuploidy, especially trisomy 21, which gives rise to Down syndrome.
The NT should be less than 3 mm to consider that the baby has no problem. On the other hand, if the NT is greater than 3 mm, it indicates that the baby is at risk of suffering from a chromosomal disorder, so more prenatal tests should be performed.
Is the nasal bone also measured in the triple screening?
The nasal bone is another of the ultrasound markers that can be used to calculate the risk index for chromosomopathies in triple screening.
Specifically, the nasal bone should be present in the 12-week pregnancy ultrasound; since the absence of nasal bone, together with increased nuchal translucency, is indicative of Down syndrome.
Other ultrasound markers are the ductus venosus (Doppler measurement performed at the insertion of the fetal umbilical cord), tricuspid regurgitation (altered flow in the tricuspid valve) and the fronto-manidubular angle (inclination between the frontal bone and the mandible).
How is triple screening in a twin pregnancy?
Combined first trimester screening in multiple pregnancies depends on the type of gestation. In the case of a two-chorionic gestation, the nuchal translucency will be assessed for each of the fetuses and two different risk indexes will be calculated. In contrast, in a singleton gestation, only one risk index is calculated taking into account the upper nuchal translucency.
Recommended readings
Another non-invasive prenatal test that is currently on the rise is the fetal DNA test in maternal blood, although this is not covered by Social Security. You can learn more about it in the following article: Non-invasive prenatal test in maternal blood.
Moreover, you will find all the types of prenatal tests on the fetus in the following post: Invasive and non-invasive prenatal diagnostic techniques
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Control prenatal del embarazo normal. PROTOCOLOS SEGO. Progresos de Obstetricia y Ginecología 2011;54(6): 330-349
Sociedad Española de Ginecología y Obstetricia (SEGO). Guía de práctica clínica: Diagnóstico prenatal de los defectos congénitos. Cribado de anomalías cromosómicas. Diagnóstico Prenatal. 2013;24(2):57–72
FAQs from users: 'Is triple screening done in all pregnancies and is it reliable?', 'What is fetal nuchal translucency?', 'Is the nasal bone also measured in the triple screening?' and 'How is triple screening in a twin pregnancy?'.
Authors and contributors
More information about Cristina Algarra Goosman




I recently found out I am pregnant, I must have missed all the signals and I may be well over 12 weeks, does this put me or my baby at risk? I am kind of nervous and wondering what I should do next I didn´t get all the normal tests done when I was supposed to
Hello Christine,
Congratulations first of all, as soon as you find out you are pregnant you should go to the doctor so they can establish that everything is okay, depending on your baby´s measurements and the results of the sonogram the doctor will establish both your health and your babies, testing whatever he/she thinks is appropriate for your specific conditions.
I hope I could help,
All the best.
Hello, I got some tests done and they told me the markers were a bit off and took me to do an amniocentesis. We were a bit skeptical but got the test done. Turns out everything was okay. I wouldn´t have taken the risk of getting that invasive procedure done, it was complicated
Hello Izzie,
These kinds of tests look for markers for specific illnesses, the result of these tests lies within a range, depending on the value, if it´s high or low it will indicate if there are more or fewer probabilities of having the disease the marker tests.
This doesn´t necessarily mean that there is indeed the presence of that illness but a higher than normal probability of having it. That is why they performed an amniocentesis. This technique is invasive but among other risks has a 1% chance of fetal death.
I hope I could help
All the best