Chorionic villus sampling (CVS) or simply chorionic villus biopsy is an invasive prenatal test in which cells are obtained from the placenta and analyzed for abnormalities in the baby.
It is performed between 10 and 14 weeks of pregnancy, which allows an earlier diagnosis than amniocentesis.
Since the technique has associated risks, a chorionic biopsy will only be performed when there are indications for it, such as advanced maternal age or a poor result in the first trimester combined screening test.
Provided below is an index with the 7 points we are going to expand on in this article.
- 1.
- 1.1.
- 1.2.
- 1.3.
- 2.
- 3.
- 4.
- 4.1.
- 4.2.
- 4.3.
- 4.4.
- 5.
- 6.
- 7.
Definition of chorionic biopsy
Chorion biopsy consists of the collection and subsequent analysis of the chorionic villi, tiny protrusions that emerge from the chorion and whose cells have the same genetic endowment as the fetus.
The chorion is the external envelope that surrounds the embryo and is involved in the formation of the placenta together with the endometrium of the mother.
In the first weeks of pregnancy, during the development of the placenta, the chorionic villi come into contact with the woman's endometrium and allow the exchange of nutrients between the mother and the fetus.
How is it done?
Depending on the gynecologist performing the test, chorionic villus sampling can be performed in two different ways:
- Transcervical route
- a semi-rigid forceps or aspiration cannula is introduced through the cervix and the chorion frondosa (placenta in formation) is accessed. Then, by continuous ultrasound monitoring, a sample of the chorionic villi is taken. This is the most commonly used method and does not require anesthesia.
- Transabdomnal route
- this method is very similar to amniocentesis. The chorion is accessed by puncture of the abdominal wall, after applying local anesthesia. The chorionic villus sampling is obtained by introducing a fine forceps through a trocar or by means of a needle aspiration.
In general, a greater amount of sample is obtained transcervically. In addition, the discomfort felt by the woman is also less by this route.
After the chorionic biopsy is performed, the woman should rest for 24 to 48 hours. Above all, it is important not to exert yourself physically or have sexual intercourse.
When is it done?
One of the advantages of chorionic villus sampling is that it can be performed between 10 and 14 weeks of gestation, thus obtaining an early diagnosis.
Amniocentesis, on the other hand, cannot be performed before the 15th week.
This is very important since, in case of an altered result, the voluntary termination of pregnancy (VTP) is less traumatic than if it is performed later.
Indications
Since it is an invasive procedure, chorionic villus sampling is only performed in women with an indication.
We will now discuss these situations:
- Pregnant women with a history of chromosomal abnormalities in a previous pregnancy.
- Parents who are carriers of genetic or chromosomal alterations.
- Observation of fetal alterations in the first trimester ultrasound.
- Obtaining a high combined risk (1/250) in the triple screen for trisomy 21 (Down syndrome), trisomy 18 (Edwards' syndrome) or other aneuploidies.
- Advanced maternal age: women over 25 years old.
Currently, chorion biopsy is the technique of choice to detect chromosomal abnormalities and/or hereditary diseases in the fetus during the first trimester of gestation.
Chorionic biopsy results
With the analysis of the chorionic villi of the placenta it is possible to rule out more than 200 pathologies in the fetus, including genetic disorders, neural tube defects or cardiac malformations.
The first test results can be obtained in as little as 48 hours, where the most common diseases are ruled out, which is much faster than in amniocentesis. The complete study of the chorionic biopsy will take a few weeks, as it also includes cell culture.
On the other hand, the reliability of amniocentesis is slightly higher than the reliability of chorion biopsy. Despite this, chorionic villus sampling has a very high degree of accuracy and provides a valid result in 99% of cases.
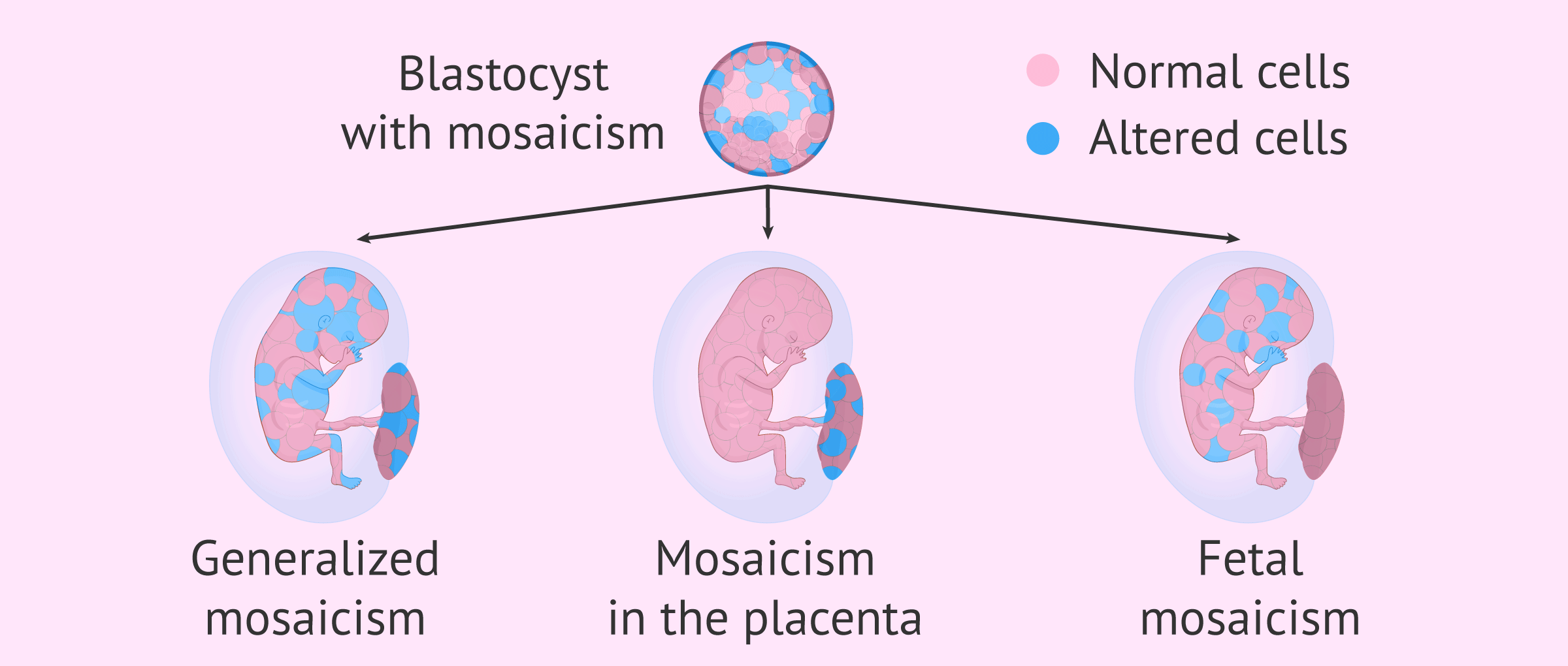
There is a minimal chance of obtaining a questionable result by the so-called mosaicism confined to the placenta. As they develop more rapidly, the chorionic villus cells may have chromosomal alterations that do not actually exist in the fetus.
In this case, it would be necessary to perform an amniocentesis to confirm the result of the chorion biopsy.
Risks
The main risk of chorion biopsy is a miscarriage, although nowadays it only occurs in a percentage of less than 1%.
Vaginal bleeding is more likely to occur after transvaginal biopsy, so it is important to rest after the test.
Other complications that can occur after chorionic villus sampling include premature rupture of the membranes, infection of the amniotic fluid and membranes (chorioamnionitis).
Chorion biopsies performed before 10 weeks gestation may result in fetal limb defects, such as shortened arms and legs or missing fingers and toes.
FAQs from users
Which is better, chorion biopsy or amniocentesis?
Both are invasive prenatal diagnostic techniques. The gynecologist should be the one to indicate when to perform one or the other depending on the gestational age.
The earliest is a chorion biopsy, which can be performed between the 10th and 14th week of pregnancy. The risk of miscarriage is 7-8%. It is performed by removing a small sample of chorionic villi.
Amniocentesis can be done between 16-18 weeks of pregnancy. It is performed by extracting amniotic fluid. The risk of miscarriage with this technique is 0.6 and 1%.
Both present a risk of natural termination of pregnancy.
Does chorionic biopsy hurt?
In principle, no. Only when the biopsy is performed transvaginally is there usually discomfort similar to that of a Pap smear, such as a prick or menstrual pain. If the biopsy is done transabdominally, the woman may feel slight discomfort when the needle enters the abdomen and subsequent pain in the lower back.
What happens if I get bad results with a chorionic biopsy?
If the chorionic villus analysis shows that the fetus is affected by some genetic malformation or abnormality, the woman or couple will have to decide whether to continue the pregnancy or perform a therapeutic abortion.
Depending on each case, the doctor may recommend amniocentesis at a later date to confirm the result.
However, it should be borne in mind that voluntary termination of pregnancy will be easier when it is done earlier.
How is chorionic biopsy performed in a twin pregnancy?
In the case of a two-chorionic gestation in which each fetus has its own placenta, it will be necessary to extract the chorionic villi from each of them. Depending on the position of each fetus in the uterus, it may be necessary to use both methods, i.e. transcervical and transabdominal.
Recommended readings
If you need more information about all the tests and the follow-up done throughout the pregnancy, you can continue reading here: Prenatal pregnancy control.
On the other hand, there are other non-invasive prenatal tests that could replace chorion biopsy, such as, for example, fetal DNA testing in maternal blood. You can read more about it in the following post: Non-invasive prenatal test in maternal blood.
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
García-Posada R, Borobio V, Bennasar M, Illa M, Borrell A. Biopsia corial transcervical: guía práctica. Diagnóstico Prenatal 2012; 23 (1): 2-10
Farrán Codina I, Sainz Bueno J A, Sánchez Durán M A, Cabero Roura L, Plaja Rustein A. Biopsia corial transabdominal en el primer trimestre: resultados en 803 casos con seguimiento neonatal. Progresos de Obstetricia y Ginecología 2002; 45 (11): 480-486
Control prenatal del embarazo normal. PROTOCOLOS SEGO. Progresos de Obstetricia y Ginecología 2011;54(6): 330-349
FAQs from users: 'Which is better, chorion biopsy or amniocentesis?', 'Does chorionic biopsy hurt?', 'What happens if I get bad results with a chorionic biopsy?' and 'How is chorionic biopsy performed in a twin pregnancy?'.
Authors and contributors
More information about Cristina Algarra Goosman




My doctor told me not to do the technique because it is risky… so it is better not to do it
Hello anon,
This procedure is indicated for women with specific concerns about their pregnancy. There are several different invasives and non-invasive techniques and not all of them are indicated for all women. If your doctor recommended not to take this test is because the risks outweigh the benefits for your particular case. This may not be true for other women.
I hope I could hep,
All the best
Hello, is this test dangerous? I am going to get it done but I am afraid that it will be painful and harmful for my baby
Hello PaigeSmith,
Chorionic villus biopsy procedure belongs to the prenatal diagnostic invasive techniques, it is used to obtain information regarding 200 pathologies the fetus may have. It takes about 10 minutes to perform and it is not painful, it has a mild discomfort associated with it but nothing out of the ordinary.
If the doctor has advised getting this test done it´s better to do it as soon as possible so you can have peace of mind and endure a healthy pregnancy.
I hope everything goes well,
Best regards.