Cervical dysplasia, also called cervical intraepithelial neoplasia, is the appearance of cells of abnormal morphology in the cervix. The cause of dysplasia may be related to contact with the papillomavirus (HPV). This virus is highly variable and only some strains are prone to cause cancer, so close monitoring by a specialist is required, but there is no need for alarm.
Its diagnosis is made by means of vaginal cytology, with subsequent analysis of the structure of the cells under the microscope. If any abnormality is detected, more specialized complementary tests, such as colposcopy, should be performed.
Provided below is an index with the 9 points we are going to expand on in this article.
- 1.
- 1.1.
- 2.
- 3.
- 4.
- 5.
- 6.
- 6.1.
- 6.2.
- 6.3.
- 7.
- 8.
- 9.
What is cervical dysplasia?
Cervical dysplasia is an alteration of the cells of the uterine cervix caused by the Human Papilloma Virus (HPV). It is these lesions that are detected by the cytology screening method. There are several types of cervical dysplasia depending on their severity.
Normally, women suffering from cervical dysplasia do not present any symptoms. Therefore, routine gynecological examinations are essential to detect any changes that may occur in the cells of the cervix as early as possible.
Degrees of dysplasia
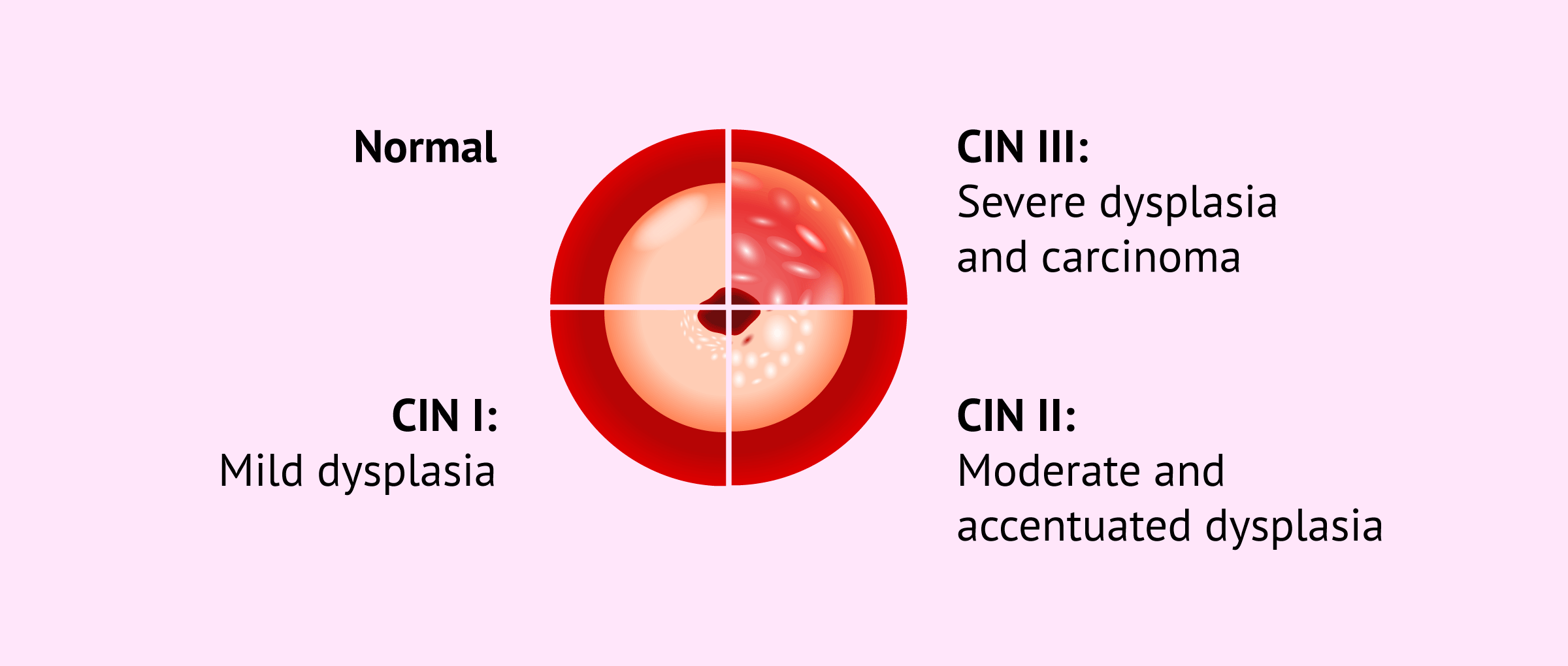
In the past, cervical dysplasia was classified as mild, moderate, and severe. However, this classification changed over the years and the term Cervical Intraepithelial Neoplasia (known as CIN) was introduced.
Based on this term and according to the appearance of abnormal cells on cervical biopsy, CIN is divided into the following groups:
- CIN I: mild dysplasia. This type of dysplasia accounts for 70% of cases and usually resolves without treatment.
- CIN II: moderate and accentuated dysplasia.
- CIN III: severe dysplasia and carcinoma. This is the most serious cervical dysplasia, as it can lead to cancer.
Why does cervical dysplasia occur?
As mentioned above, the abnormal changes that occur in the cells of the cervix are usually caused by the human papillomavirus. However, there are also other factors that increase a woman's risk of developing cervical dysplasia, for example:
- Early pregnancy and childbirth.
- Multiple sexual partners.
- Suffering from diseases such as tuberculosis or sexually transmitted diseases.
- Immune system inhibitor drugs.
In addition, women who have been exposed to diethylstilbestrol (DES) while pregnant are also more likely to develop cervical dysplasia over time. Environmental factors such as exposure to tobacco smoke as well as vitamin deficiencies are also associated with an increased risk of developing cervical dysplasia.
On the other hand, it should be noted that a certain genetic susceptibility to cervical cancer production has been observed in 1% of women.
How is it diagnosed?
The basic test for detecting possible cervical dysplasia is the Pap smear or Papanicolaou (PAP) test. However, this diagnostic test is usually accompanied by other studies to confirm that the woman has cervical dysplasia with complete certainty.
Listed below are some of the complementary diagnostic methods for cervical dysplasia:
- Visual inspection with acetic acid (IVVA)
- the physician performs a cervical lavage using 3% or 5% acetic acid. If the patient has cervical dysplasia, it will change color and become whitish. In this case, the result will be IVVA positive. When the epithelium does not change color, it corresponds to a negative IVVA and the woman does not have cervical dysplasia.
- Molecular Tests
- to detect the presence of human papillomavirus (HPV) genetic material.
- Colposcopy
- procedure through which the cervix, vagina, and cervical canal are analyzed. In addition, this test allows the gynecologist to take a sample for biopsy.
In any case, the decision to carry out complementary tests to the Pap smear will depend on the specialist himself and the doubts that may arise according to the result obtained from the PAP.
Treatment of dysplasia
Mild dysplasias may disappear without the need for any type of treatment, although monitoring is required for three to six months to ensure that the affected area does not expand.
In contrast, moderate to severe dysplasias should be treated to prevent them from eventually developing into cancer. Generally, the removal of the tissue with abnormal cells is chosen. For this purpose, there are different methods:
- Cryosurgery: discarding of altered cells by cold.
- Laser: suppression of abnormal cells by heat.
- Electrocautery: elimination of damaged cells by electricity.
- Conization, i.e., a procedure to remove abnormal uterine tissue.
In the most severe cases of cervical dysplasia, although this is not usually the case, it is necessary to resort to hysterectomy. It involves the removal of the uterus, so the woman will not be able to become pregnant. In these cases, the options for these women to become mothers would be to resort to adoption or surrogacy.
Whatever the therapeutic option applied to solve the problem, dysplasia requires periodic monitoring approximately every three to six months.
Does dysplasia affect pregnancy?
Women with cervical dysplasia can become pregnant even if they have the condition.
The gynecologist will monitor the course of the pregnancy to see if there is a change in the dysplasia. In addition, if the dysplasia is treated prior to pregnancy, it is important to know that the colposcopy technique has no contraindications for pregnancy.
However, treatment to eliminate dysplasia could entail the risk of preterm delivery and also the remission of dysplasia after delivery.
On the other hand, it has not been demonstrated that the presence of cervical dysplasia in the mother has a negative effect on the formation of the fetus, or on the achievement of a normal pregnancy.
In any case, it is very important that routine gynecological controls are performed to detect any minimal changes in the reproductive tract, and thus put it solved as soon as possible in pregnant women.
FAQs from users
Is pregnancy possible if I have cervical dysplasia?
These types of lesions in themselves do not prevent pregnancy, but if the alteration detected is of high grade (H-SIL), it is recommended that the lesion be removed (usually with a simple surgery called conization) before the woman becomes pregnant.
In other cases, with controlled low-grade lesions (L-SIL), pregnancy will not be contraindicated. Dysplasia has not been shown to have a negative effect on fetal development.
What is important to keep in mind is that women who have previously undergone conization will have an increased risk of cervical incompetence, which can lead to premature delivery. As a preventive measure, serial cervical length measurements should be taken during gestation.
In cases where the length is very short or becomes shorter during pregnancy, preventive treatments such as cervical cerclage or pessaries are indicated to try to avoid preterm labor as much as possible.
Can cervical dysplasia be prevented?
Yes, the risk of cervical dysplasia can be reduced by avoiding risky sexual intercourse, undergoing regular gynecological check-ups, practicing miscarriage, etc.
In addition, vaccination against human papillomavirus before having sex for the first time is also effective in reducing the likelihood of developing cervical dysplasia.
Is there a cure for cervical dysplasia?
There are different therapeutic ways to treat cervical dysplasia, so it can be said that there is a cure for this condition.
However, it is common for cervical dysplasia to recur in previously treated women. It is possible that the woman may be re-infected with the HPV virus or that the virus has been hiding in another part of her body.
Recommended readings
As mentioned above, the main cause of cervical dysplasia is the human papillomavirus. If you want to learn more about this virus, we recommend you to visit the following article: What is the human papillomavirus? - Types, contagion and vaccines.
In addition, a possible solution for a woman diagnosed with severe cervical dysplasia would be conization. If you are interested in learning more about this intervention, you can visit this link: Cervical conization: complications and advice.
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Amanda N Fader, Erin K Alward, Amy Niederhauser, Christina Chirico, Jamie L Lesnock, Daniel J Zwiesler, Richard S Guido, Darla J Lofgren, Michael A Gold, Kathleen N Moore. Cervical dysplasia in pregnancy: a multi-institutional evaluation. Am J Obstet Gynecol. 2010 Aug;203(2):113.e1-6. doi: 10.1016/j.ajog.2010.04.016 (See)
Giorgio Bogani, Elena Tagliabue, Stefano Ferla, Fabio Martinelli, Antonino Ditto, Valentina Chiappa, Umberto Leone Roberti Maggiore, Francesca Taverna, Claudia Lombardo, Domenica Lorusso, Francesco Raspagliesi. Nomogram-based prediction of cervical dysplasia persistence/recurrence. Eur J Cancer Prev. 2019 Sep;28(5):435-440. doi: 10.1097/CEJ.0000000000000475 (See)
Giorgio Bogani, Maurizio Serati, Umberto Leone Roberti Maggiore, Antonino Ditto, Barbara Gardella, Simone Ferrero, Arsenio Spinillo, Fabio Ghezzi, Francesco Raspagliesi. Cervical intraepithelial neoplasia in women who had vaccination against HPV. Int J Gynaecol Obstet. 2019 Nov;147(2):233-237. doi: 10.1002/ijgo.12934 (See)
Meggan Zsemlye. High-grade cervical dysplasia: pathophysiology, diagnosis, and treatment. Obstet Gynecol Clin North Am. 2008 Dec;35(4):615-21; ix. doi: 10.1016/j.ogc.2008.09.008.
Mikel Gorostidi, Arantza Lekuona, Arantxa Juaristi, Glauco Baiocchi. Vaginal carcinoma after cervical dysplasia. Int J Gynecol Cancer. 2020 Feb;30(2):265-273. doi: 10.1136/ijgc-2019-001062 (See)
Omer Cohen, Edwardo Schejter, Regina Agizim, Ron Schonman, Gabby Chodick, Ami Fishman, Anat Hershko Klement. Postcoital bleeding is a predictor for cervical dysplasia. PLoS One. 2019 May 23;14(5):e0217396. doi: 10.1371/journal.pone.0217396. eCollection 2019 (See)
FAQs from users: 'Is pregnancy possible if I have cervical dysplasia?', 'Can cervical dysplasia be prevented?' and 'Is there a cure for cervical dysplasia?'.
Authors and contributors
More information about Cristina Algarra Goosman







Hello, my doctor told me that I have cervical dysplasia and that she has to laser-tissue off or something. I am kind of afraid of having to get this procedure done, isn´t there another technique I can get done that is less invasive?
Hello Pam,
The type of procedure that the doctor chooses is based on the degree of dysplasia that your cervix presents, based on the degree and the amount of tissue that they have to remove she will decide between the different options.
I recommend you speak to your doctor so she can explain the different options you have and which one is indicated for you based on your characteristics.
I hope I could help,
All the best.