Conization, also called cone biopsy, is a small surgical procedure performed on women who have observed a precancerous lesion on the cervix. This is a preventive measure to remove tissue from the uterus that may cause problems in the future.
These precancerous lesions are caused by infection with human papillomavirus (HPV), which is acquired by unprotected sex.
Conization is not associated with serious risks to women's health, although as in any surgical intervention, they are always possible.
Provided below is an index with the 9 points we are going to expand on in this article.
- 1.
- 1.1.
- 2.
- 3.
- 4.
- 4.1.
- 5.
- 6.
- 6.1.
- 6.2.
- 6.3.
- 6.4.
- 6.5.
- 7.
- 8.
- 9.
What is cervical conization?
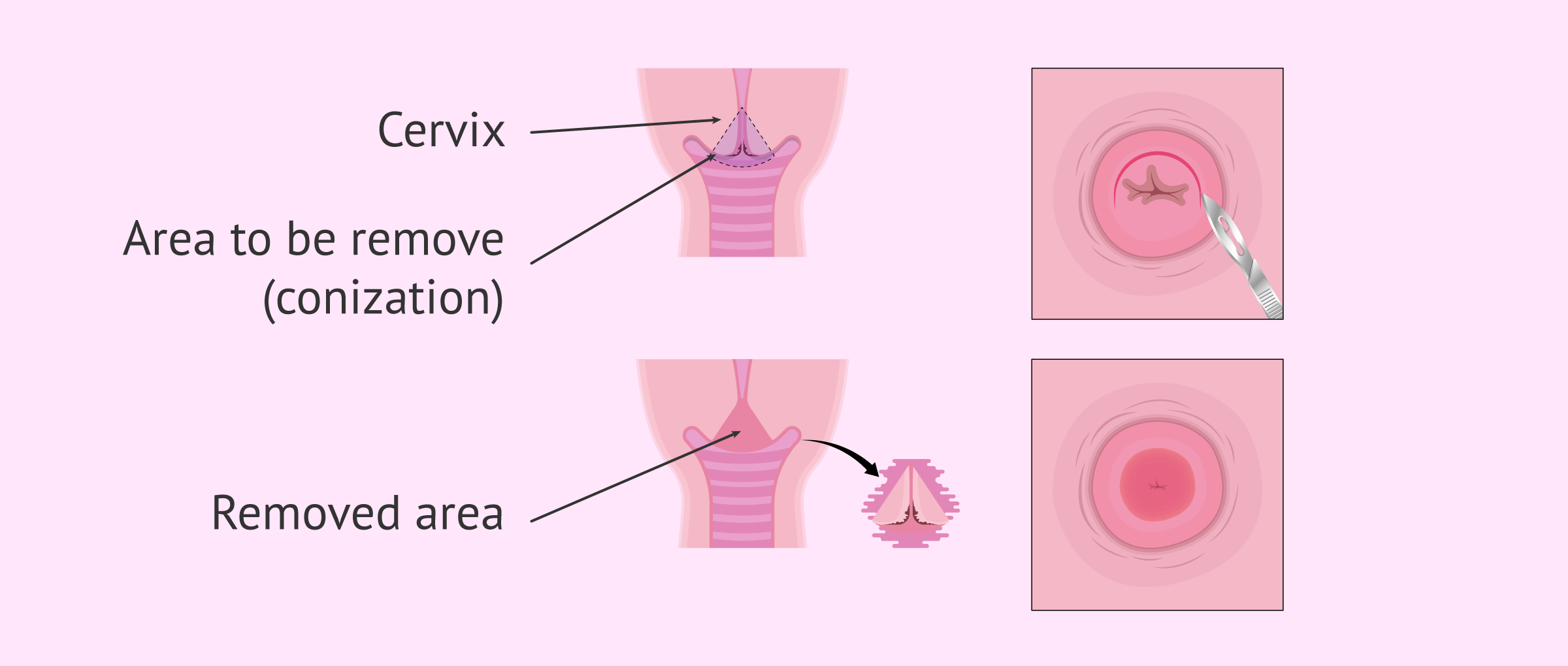
Conization is a medical procedure in which part of the abnormal tissue of the cervix is removed through a cone-shaped incision. Thus, the base of the cone comprises the external part of the cervix (exocervix); while the vertex of the cone comprises the internal part of the cervix (endocervix).
The removed piece of tissue is then evaluated under a microscope for the presence of abnormal cells. The results are usually available within a week, although this time may vary depending on each laboratory.
Cervical conization is indicated in moderate and severe cervical dysplasia, i.e., grade II or III respectively. Normally, these lesions are derived from an infection with human papillomavirus (HPV), a sexually transmitted disease (STD).
Cervical dysplasia refers to abnormal changes in the cells on the surface of the cervix, which can be considered precancerous cells. These changes are due to HPV infection.
Objectives
In general, this surgical treatment for premalignant lesions of the cervix has a double objective:
- Diagnosis
- to assess the severity and extent of the HPV lesion on the cervix.
- Therapeutic
- premalignant lesions are removed to avoid problems in the future, acting as a preventive method against cancer.
Another purpose of uterine conization is to see if there is an endocervical extension, that is, an abnormal growth within the cavity of the cervix. For this, a microlegrade is performed along with this procedure.
Procedure
Cervical conization is relatively simple and lasts about 15 minutes. The procedure can be performed with:
- Local anesthesia: this is the most uncomfortable method for women but involves fewer complications. This type of anesthesia is injected into the tissues surrounding the cervix.
- Regional or spinal anesthesia: will numb only the lower half of the body.
- General anesthesia: The patient will completely be unconscious.
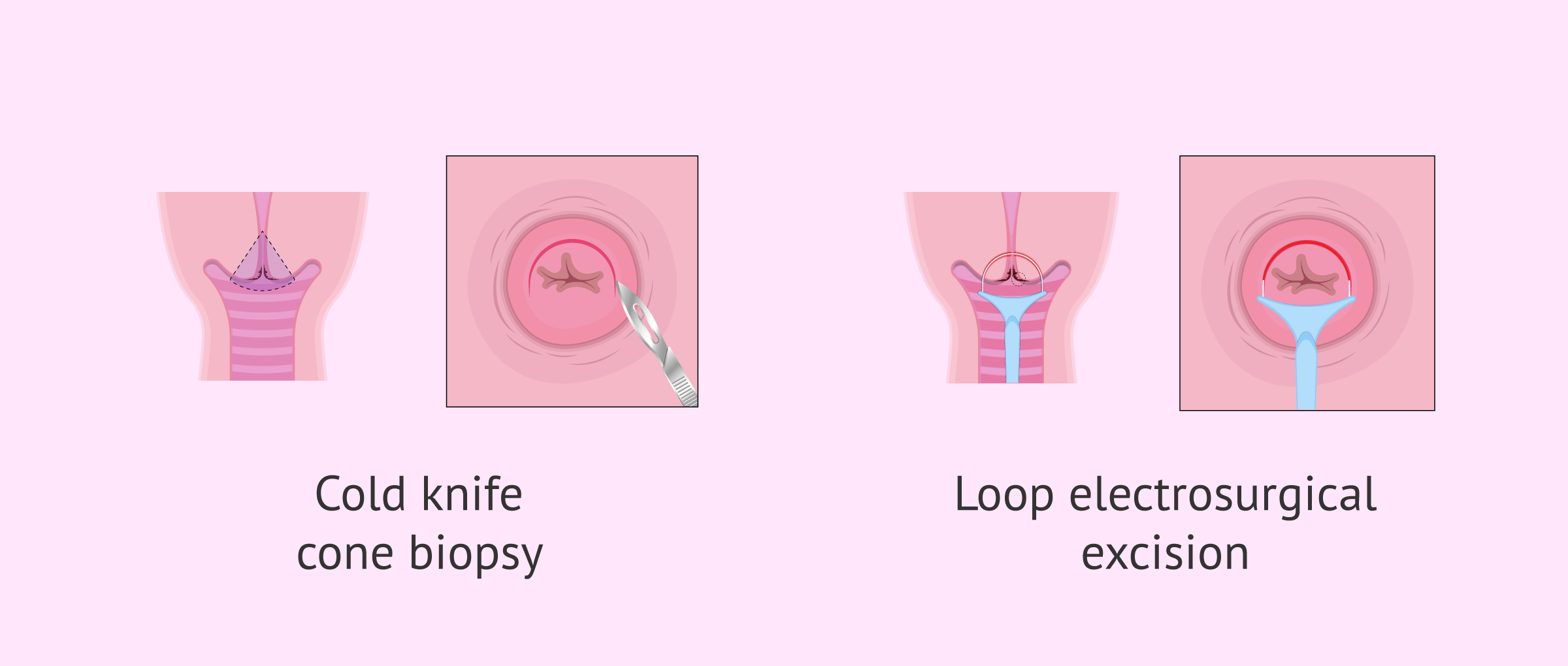
After anesthesia is given, the gynecologist places the speculum in the woman's vagina to visualize the cervix. By using a surgical scalpel, laser scalpel, or electrically heated wire, the doctor makes a cone-shaped cut in the cervix. In order to control bleeding, the doctor will also place some stitches in the patient’s cervix.
This piece of removed tissue is sent to the laboratory to check for abnormal cells or to evaluate if cancer is present.
If cancer or precancerous cells are found in the cervix, the specialist will send additional tests to the woman and a treatment plan will be put in place. After a few hours and after verifying that the patient has reacted well to the intervention and has removed the anesthesia, the patient can leave the clinic.
Complications of cervical conization
The risks of this type of treatment are very low and almost always highly effective. Most women have no serious complications after uterine conization, although bleeding is common. Therefore, the woman should be alert for heavy, bright red bleeding.
Apart from that, lesions may appear on the vaginal walls or a reaction due to drugs administered for anesthesia. Although less frequent, uterine insufficiency may also occur in the long term causing the patient to have a decreased and/or open cervix. As a result, these women will be at greater risk of miscarriage or premature birth.
Women treated for a premalignant cervical lesion have an increased risk of new lesions or cancer. For this reason, these women must undergo stricter checks and controls.
Tips for patients
Depending on how the cervical conization is performed, preoperative conditions vary. Therefore, it is vitally important to consider the type of anesthesia used.
If conization is performed under local anesthesia, fasting is not necessary; whereas when general or regional anesthesia is used, the woman must fast within 8 hours prior to the intervention.
Once the cervical conization has been performed, the woman should follow some tips such as those detailed below:
- Remain between 3 and 4 days in rest.
- Limit physical activity for two weeks.
- No sexual intercourse for 4 weeks.
- Avoid vaginal showers for the first 3-4 weeks.
If a woman has heavy vaginal bleeding or a large amount of foul-smelling vaginal discharge after uterine conization, it is recommended to consult a physician as soon as possible.
Recommendations
In order to avoid or reduce the risk of developing another injury after conization, we recommend the patient to:
- Use Condom for at least the first 6 months after conization, although her doctor will advise her to continue using it afterwards.
- Stop smoking, as tobacco interferes with the immune system's ability to defend itself against HPV.
- Vaccinate against cervical cancer, which would reduce the risk by 60-80%. It should be noted that the vaccine does not cure an injury, but reduces the risk of new infections and injuries.
Uterine conization and pregnancy
Many women undergoing uterine conization are concerned about the possible effects on their fertility. They wonder if they'll have trouble becoming mothers in the future. It is difficult to respond to this dilemma, since the consequences of this surgical procedure are not fully observed until a pregnancy is attempted.
Egg quality is not affected by the operation, since the ovaries do not suffer any alteration.
As mentioned before, one of the most common fertility consequences of cervical conization is uterine insufficiency. This occurs when a deep cone biopsy is performed that affects the muscle fibers that help keep the cervix closed. As a result, these women will be at greater risk of miscarriage or premature birth.
Although rare, scarring of the cervix can also occur, which would prevent sperm from entering the uterus and lead to a natural pregnancy. When this occurs, assisted reproduction techniques must be used to achieve pregnancy.
FAQs from users
What's the difference between colposcopy and conization?
The two terms are related to cervical pathologies.
Colposcopy is a diagnostic technique that consists of examining the cervix with a microscope after having applied different dyes and stains. In this way it is possible to locate the existence of a specific lesion and biopsy it for an accurate diagnosis.
Conization is a surgical treatment for premalignant lesions diagnosed in the cervix. It is the exeresis or removal of margins of the entire altered area of the cervix, which has been previously diagnosed by colposcopy.
What does a LEEP procedure consist of?
The LEEP procedure, which stands for Loop Electrosurgical Excision, is a method that allows for the evaluation and treatment of diseases of the cervix and vagina.
This quick technique is performed while the patient is not on her period and consists of using an electrically heated wire loop to remove abnormal tissue from infections, warts, tumors, and polyps.
In which cases is conization indicated?
Conization of the uterus is performed on women who are in any of the following situations:
- Women who have been diagnosed with early stage uterine cancer.
- Women showing signs of precancerous lesions.
- Women with a lesion on the cervix without a clear diagnosis.
- Women with persistent lesions on the cervix due to HPV infection.
How will I feel after a cone biopsy?
It is normal that after a uterine conization the patient feels cramps during the first week. In addition, over the next 2-3 weeks, the discharge may contain blood and a yellowish color.
When can I start exercising again after cervical conization?
After a cervical conization it is recommended to wait between 2 and 3 weeks approximately to return to sports.
The patient should wait until the wound has healed completely and no blood flow comes out.
Suggested for you
The main cause for uterine conization is HPV infection. You can read more about this virus here: What is human papillomavirus - Types, transmission and vaccines.
Another possible complication of uterine conization is uterus insufficiency, which leads to spontaneous miscarriage. For more information, we recommend you read the following article: What is recurrent miscarriage? Causes, Symptomes and Treatment.
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Luo C, Qiu J, Zhang J, Yuan L, Liu C, Wang C, Li Y, Zhang L, Cheng W. Analysis of the risk factors of residual lesions after conization and prognosis of multifocal micro-invasive squamous cell cervical carcinoma treated with different types of surgery. Mol Clin Oncol. 2019 Oct;11(4):364-370. doi: 10.3892/mco.2019.1904 (View)
Giannella L, D'Ippolito G. Cervical ripening balloon: An off-label but effective use to manage massive hemorrhage during outpatient cervical conization. Int J Gynaecol Obstet. 2019 Oct;147(1):126-127. doi: 10.1002/ijgo.12910.
Giray B, Kabaca-Kocakusak C, Guray-Uzun M, Akis S. Post-conization follow-up of patients with CIN 2/3 with different amount of distance to negative cone biopsy margin: a retrospective cohort study. J Obstet Gynaecol. 2019 Aug 28:1-5. doi: 10.1080/01443615.2019.1633517 (View)
Yamamoto R, Sekiyama K, Higuchi T, Ikeda M, Mikami M, Kobayashi Y, Nagase S, Yokoyama M, Enomoto T, Katabuchi H. Value and limitation of conization as a diagnostic procedure for cervical neoplasm. J Obstet Gynaecol Res. 2019 Oct 1. doi: 10.1111/jog.14118 (View)
FAQs from users: 'What's the difference between colposcopy and conization?', 'What does a LEEP procedure consist of?', 'In which cases is conization indicated?', 'How will I feel after a cone biopsy?' and 'When can I start exercising again after cervical conization?'.