When a man decides to undergo vasectomy in order to have unprotected intercourse without risk of conceiving, one should make sure that it has been 100% successful, that is, there is no risk of unintended pregnancy.
For this reason, doing several control semen analyses is necessary during the months post vasectomy in order to confirm whether the sperm count is zero. In other words, if the treatment has been successful.
Otherwise, if after some time there are still sperm in the ejaculate, then the vasectomy would not have worked and it would be necessary to repeat the intervention.
Provided below is an index with the 7 points we are going to expand on in this article.
- 1.
- 2.
- 3.
- 4.
- 4.1.
- 4.2.
- 4.3.
- 5.
- 6.
- 7.
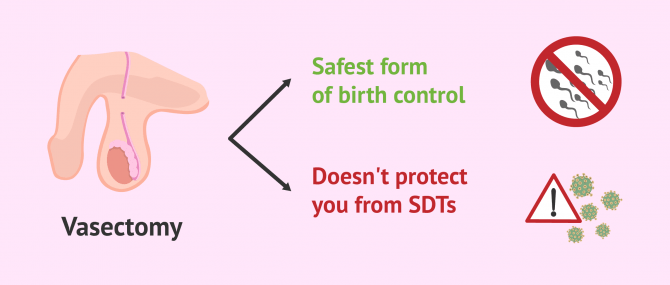
Advantages of vasectomy
A vasectomy is a type of permanent sterilization for males that involves the resection and ligation of the vasa deferentia of the male reproductive system. As a result, the man is expected to have obstructive azoospermia, that is, zero sperm count due to a blockage in the vasa deferentia.
This birth control method is permanent in almost all cases. For this reason, men who regret having had a vasectomy and wish to conceive in the future, will have to undergo a vasectomy reversal the aim of rejoining the two cut segments.
On the other hand, the following are the potential advantages of vasectomy:
- A vasectomy is a painless procedure that is very convenient for those males who don't want more children
- It doesn't lead to unpleasant intercourse, inhibit the capacity for the man to ejaculate, or lower sex drive
- The man will continue to have orgasms as usual
- Unprotected intercourse can be resumed about one week after the surgical procedure, provided that everything goes as expected
It should be noted that this technique does not protect against STDs (Sexually Transmitted Diseases), a major disadvantage if compared to the condom.
If you would like to learn more about vasectomy itself, we recommend you visit the following article: What is a vasectomy? The procedure its effectiveness explained.
Post vasectomy sperm checks
A semen analysis, also known as seminogram or semenogram, is a diagnostic test used for male fertility testing. It allows the specialist to evaluate the different sperm parameters, including sperm concentration, sperm motility, and sperm morphology.
This is the reason why a semen analysis is so useful when it comes to evaluate under the microscope whether there is presence of spermatozoa or not after a vasectomy.
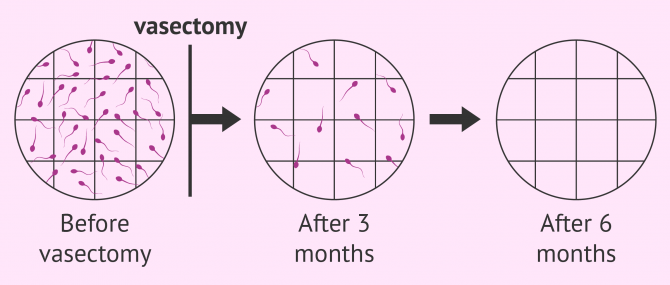
The effectiveness of vasectomy is 99%, but the effects are not immediate. The male has to ejaculate a few times after the procedure in order to release all the sperms that are still present in the seminal ducts, which could cause a pregnancy.
So, in order to prevent an unwanted pregnancy after the first months, couples are strongly advised to continue using other birth control methods.
Prior to giving sperm clearance, a series of post vasectomy sperm tests are required until no sperms are found on the semen sample. This would mean that the treatment has been successful. The first semen analysis can be done 3 months after vasectomy, when the man is expected to having ejaculated an average of 20 times.
About 80 percent of men with a vasectomy will have no sperms in the 3 month check. In these cases, sperm clearance is given after this sperm test. If the sperm test was positive after vasectomy, further rechecks would be necessary until the sperm count is zero.
In spite of this, some specialists recommend these men to undergo annual rechecks in order to make sure that recanalization of the vasa deferentia doesn't occur, which would lead to vasectomy failure.
Sperm clearance after vasectomy
To determine if the results of a vasectomy have been successful or not, clearance can only be given based on the absence of motile sperm. Particularly, the sperm count of the ejaculate after 3 months should be below 100,000 motile sperm per sample or ideally zero.
However, sometimes it takes longer than expected to reach zero sperm count. In this case, the semen analysis would be repeated 6 months after the procedure. If the sample still contains sperm the vasectomy procedure should be done again.
Giving sperm clearance to these patients is not possible if motile spermatozoa are still present on the ejaculate, as this would mean that pregnancy is still possible. Whenever motile sperm are present, a man could get a woman pregnant.
To determine if a vasectomy has been successful, azoospermia must be diagnosed after one or two post vasectomy sperm tests. That is to say, the sperm count is equal to zero.
FAQs from users
When is it recommended to check if the vasectomy has been effective?
A seminogram is usually requested three months after the vasectomy. Given that the period of production of the sperm is approximately 3 months, if azoospermia is proven after this period, it is possible to deduce that the testicle is functioning at full capacity after the surgery and that the section has been a success since no sperm reaches the exterior.
Are there live spermatozoa after vasectomy?
For the first few months after vasectomy, the vas deferens of the male still harbors sperm that have not been ejaculated, some of which may still be alive. During this time, there is a degree of post-vasectomy oligozoospermia until all sperm have been completely eliminated with several ejaculations.
Is there a risk of pregnancy after vasectomy?
Vasectomy is one of the most effective contraceptive methods available. However, if unprotected sexual relations are maintained before having passed all the post-vasectomy controls, it is possible to become pregnant. In addition, there are cases of women who have become pregnant years after their partner's vasectomy, although it is highly improbable.
Recommended reading
Men who change their minds and want to have children after vasectomy have no choice but to consider undergoing vasectomy reversal or IVF with Testicular sperm extraction (TESE). Check out this for information: Can You Get Pregnant After a Vasectomy? – Your Realistic Possibility.
The semen analysis is the most important test to evaluate male fertility. Get more info by clicking the following link: What Is a Semen Analysis Report? – Purpose, Preparation & Cost.
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Ahmad Majzoub, Nicholas N Tadros, A Scott Polackwich, Rakesh Sharma, Ashok Agarwal, Edmund Sabanegh Jr. Vasectomy reversal semen analysis: new reference ranges predict pregnancy. Fertil Steril. 2017 Apr;107(4):911-915. doi: 10.1016/j.fertnstert.2017.01.018. Epub 2017 Mar 7 (View)
Brian Z Rayala, Anthony J Viera. Common questions about vasectomy. Am Fam Physician. 2013 Dec 1;88(11):757-61 (View)
Daniel Beder, Sudhanshu Chitale. The clinical impact of British guidelines on post-vasectomy semen analysis. Cent European J Urol. 2020;73(4):558-562. doi: 10.5173/ceju.2020.0003.R2. Epub 2020 Sep 26 (View)
Jared Diederichs, Patrick McMahon, Johnathan Tomas, A J Muller. Reasons for not completing postvasectomy semen analysis. Can Fam Physician. 2019 Sep;65(9):e391-e396 (View)
Jasper C Bash, Jamie O Lo, Akash A Kapadia, Malachi Mason, Jason C Hedges. Vasectomy reversal outcomes in men after testosterone therapy. Sci Rep. 2022 Nov 14;12(1):19496. doi: 10.1038/s41598-022-22823-8 (View)
FAQs from users: 'When is it recommended to check if the vasectomy has been effective?', 'Do you shoot blanks after a vasectomy?', 'Are there live spermatozoa after vasectomy?', 'How long does it take for a man to become sterile after a vasectomy?', 'Why two sperm tests after vasectomy?' and 'Is there a risk of pregnancy after vasectomy?'.
Authors and contributors

More information about Michelle Lorraine Embleton




Hello, my semen analysis report after vasectomy says 1.5 sperm volume and 0 million per ml as regards the sperm count. How should I interpret the results? Successful or not? Will I get my wife pregnant if we have sex?
Hello Clark,
There are no sperms in your semen sample. In other words, your vasectomy has been 100% successful. You can enjoy unprotected sex with your wife without being worried about an unwanted pregnancy.
I hope this helps,
Best