Steinert's myotonic dystrophy or myotonic dystrophy type 1 (DM1) is the most common adult muscular dystrophy. Individuals affected by this disease have an abnormality in the DMPK gene.
DM1 is characterized by progressive muscle weakness, myotonia (impaired muscle relaxation), and the presence of cataracts.
It should be noted that Steinert's disease does not only affect the muscles. It is a multisystem disease that can affect the brain, heart, gastrointestinal, endocrine, and respiratory systems.
Provided below is an index with the 9 points we are going to expand on in this article.
- 1.
- 2.
- 3.
- 4.
- 5.
- 6.
- 6.1.
- 6.2.
- 6.3.
- 7.
- 8.
- 9.
Is Steinert myotonic dystrophy inherited?
Myotonic dystrophy type 1 is a multisystem disease with an autosomal dominantpattern of inheritance. This means that, if one of the parents is affected (regardless of whether it is the father or the mother), the probability of transmitting the disease to their offspring is 50% each time they have a child.
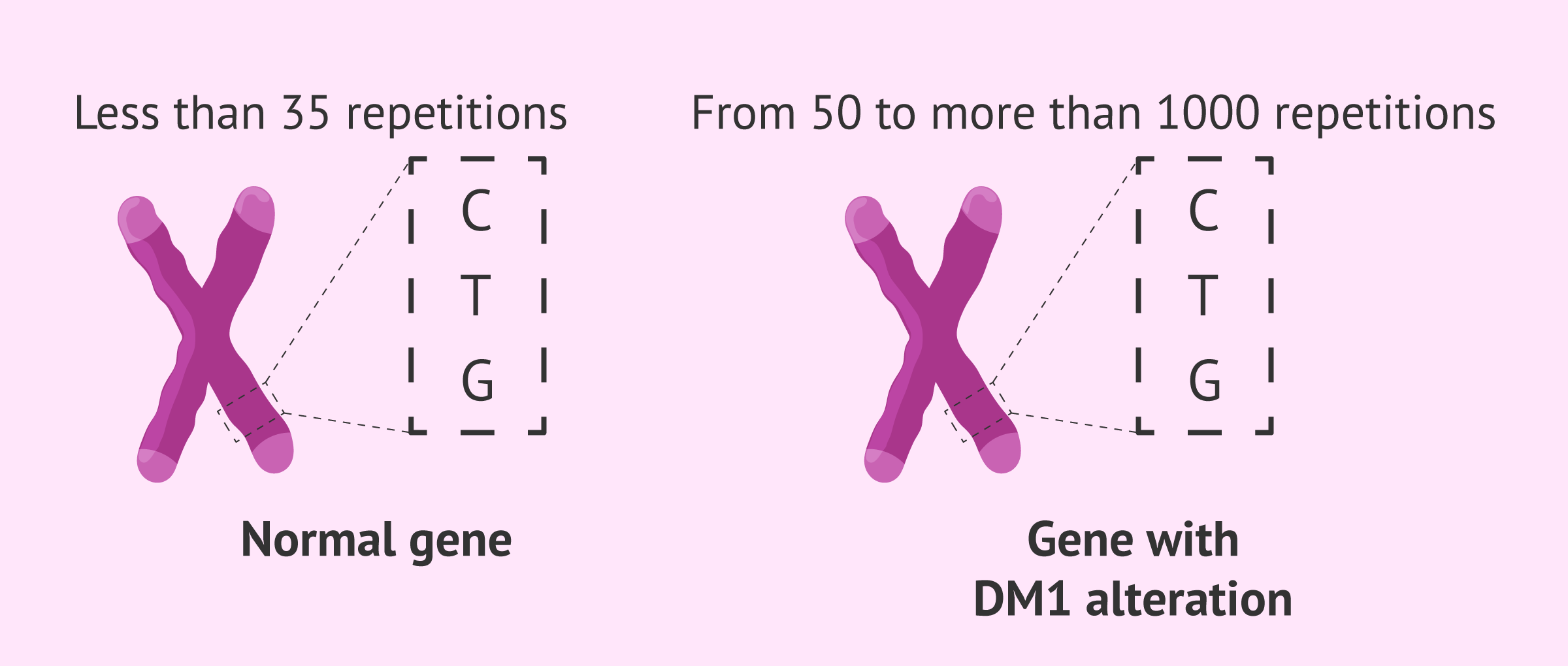
The genetic alteration causing DM1 is an expansion of the CTG triplet in the DMPK gene. This triplet is found repeated less than 35 times in healthy individuals but is repeated from 50 to more than 1000 times in individuals carrying the genetic alteration of Steinert's disease.
In addition, this disease presents the phenomenon known as anticipation. This implies that the age of onset of DM1 usually decreases as it progresses through the generations because the number of triplet repeats increases. Thus, Steinert's disease appears earlier in offspring, which presents the additional problem that the earlier the disease presents itself, the more severe it appears to be.
On the other hand, it seems that the expansion of the triplet is more pronounced when it is the female who transmits the disease to her offspring.
Symptoms
Steinert's disease can appear in the adult period, as well as in childhood or even congenitally, and will be more severe the earlier it appears. Some of the symptoms and conditions resulting from DM1, although these can be highly variable, are:
- Myotonia. Abnormal relaxation of the muscles after a contraction. Myotonia may increase with cold or stress and improve with repeated exercise.
- Cataracts before the age of 50.
- Arrhythmias and cardiac conduction disturbances.
- Fatigue and respiratory problems.
- Sleep disorders.
- Cognitive alterations.
- Endocrine disorders such as insulin resistance.
- Digestive problems. Dysphagia (difficulty in swallowing food), for example, may occur due to muscle involvement.
In addition, these patients may have an elevated risk of certain types of cancer such as endometrial, ovarian and testicular cancers, as well as complications related to general anesthesia.
Because of all this, the life expectancy of patients with Steinert's disease may be reduced.
Diagnosis
Confirmatory diagnosis of Steinert's disease is made by genetic testing of a blood sample.
It is important to note that genetic counseling is essential in this type of case. When the diagnosis of DM1 is made, questions will arise as to whether close relatives and offspring could develop the disease. These relatives may opt for genetic testing. However, especially in the case that they have no symptoms, they should know in advance the implications of knowing that they may have the genetic alteration of the disease and develop myotonic dystrophy type 1 later on.
In the event that gestation is desired and one of the parents has DM1, one option to avoid having affected offspring would be to perform in vitro fertilization (IVF) with preimplantation genetic testing (PGT). In this way, the embryos would be genetically studied, which would make it possible to select only those that have been found to be healthy.
You can obtain much more information about this genetic study in the following article: What is preimplantation genetic diagnosis or PGD?
Assisted procreation, as any other medical treatment, requires that you rely on the professionalism of the doctors and staff of the clinic you choose. Obviously, each clinic is different. Get now your Fertility Report, which will select several clinics for you out of the pool of clinics that meet our strict quality criteria. Moreover, it will offer you a comparison between the fees and conditions each clinic offers in order for you to make a well informed choice.
Treatment
There is no cure for myotonic dystrophy type 1. Treatment will consist of palliating the symptoms produced by the disease.
In addition, tests and monitoring of cardiac and respiratory function and gastrointestinal, endocrine and/or ocular manifestations of Steinert's disease will be necessary. Therefore, the approach to DM1 should be carried out by a multidisciplinaryteam.
Myotonic dystrophy type 1 and pregnancy
When a woman with DM1 becomes pregnant, the manifestations of the disease may worsen. However, these symptoms seem to improve after delivery, although disease progression may occur.
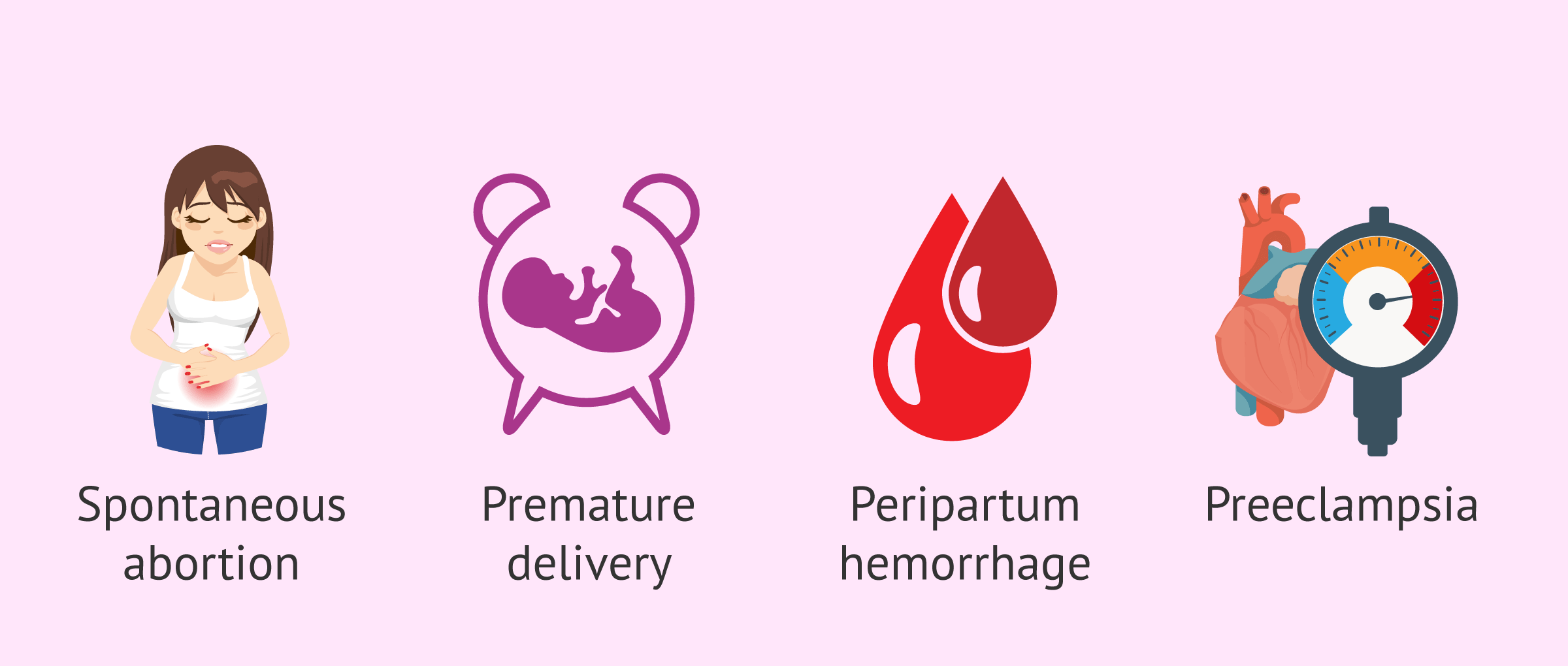
In addition, pregnant women with myotonic dystrophy type 1 may be at increased risk of complications such as miscarriage, premature delivery, peripartum hemorrhage or preeclampsia.
On the other hand, prenatal diagnosis makes it possible to check before birth whether the baby has inherited myotonic dystrophy type 1. This will be especially relevant when the mother is the one affected by DM1, as the triplet expansion may be greater for the offspring and result in a more severe and congenital form of the disease. In this way, if desired and possible, the pregnancy could be terminated.
However, it would not make sense to perform this prenatal test if you are going to continue with the pregnancy even if the result shows that the baby has the genetic alteration of the disease.
FAQs from users
Does Steinert's disease reduce life expectancy?
Steinert's disease can affect life expectancy, but it is important to take into account the time at which symptoms appear. This means that if myotonic dystrophy type 1 manifests late, life expectancy may not be reduced. However, life expectancy may be affected in the more severe congenital forms.
Is it true that Steinert myotonic dystrophy causes problems with anesthesia?
Yes, it is true that having Steinert's myotonic dystrophy can cause problems with anesthesia. This is why it is very important to make sure that the specialists and the anesthesiologist have taken into account that you have this disease, in order to prevent risks and be prepared for possible complications.
In addition, it is advisable to perform a respiratory evaluation of the patient with Steinert's myotonic dystrophy prior to general anesthesia.
Is there any alternative to PGD to prevent the transmission of genetic diseases?
If preimplantation genetic diagnosis is not done, the only option left would be fetal or prenatal resting through amniocentesis or chorionic villus sampling (CVS). The main disadvantage of this type of genetic testing is that the woman would have no alternative but to choose to terminate her pregnancy in case a genetic disease was detected, given that she has to be already pregnant for these techniques to be carried out.
Alternatively, prospective parents can decide not to use their oocytes and/or sperms to avoid the transmission of genetic diseases to their offspring. In such case, donor gametes would be used.
Recommended readings
Steinert's disease is a monogenic disease, i.e. it affects a single gene. If you want to learn more about monogenic diseases, you can visit the following link: What are monogenic diseases - Avoiding them with PGD.
On the other hand, if you are interested in prenatal diagnosis techniques, we recommend you to read the following article: Invasive and non-invasive prenatal diagnostic techniques
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Bird TD. Myotonic Dystrophy Type 1. 1999 Sep 17 [updated 2021 Mar 25]. In: Adam MP, Ardinger HH, Pagon RA, Wallace SE, Bean LJH, Mirzaa G, Amemiya A, editors. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993–2021. PMID: 20301344.
Gutiérrez Gutiérrez G, Díaz-Manera J, Almendrote M, Azriel S, Eulalio Bárcena J, Cabezudo García P, Camacho Salas A, Casanova Rodríguez C, Cobo AM, Díaz Guardiola P, Fernández-Torrón R, Gallano Petit MP, García Pavía P, Gómez Gallego M, Gutiérrez Martínez AJ, Jericó I, Kapetanovic García S, López de Munaín Arregui A, Martorell L, Morís de la Tassa G, Moreno Zabaleta R, Muñoz-Blanco JL, Olivar Roldán J, Pascual Pascual SI, Peinado Peinado R, Pérez H, Poza Aldea JJ, Rabasa M, Ramos A, Rosado Bartolomé A, Rubio Pérez MÁ, Urtizberea JA, Zapata-Wainberg G, Gutiérrez-Rivas E. Clinical guide for the diagnosis and follow-up of myotonic dystrophy type 1, MD1 or Steinert's disease. Neurologia (Engl Ed). 2020 Apr;35(3):185-206. English, Spanish.
Jain A, Al Khalili Y. Congenital Myotonic Dystrophy. 2020 Dec 15. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan–. PMID: 32809353.
Johnson NE. Myotonic Muscular Dystrophies. Continuum (Minneap Minn). 2019 Dec;25(6):1682-1695.
Romeo V. Myotonic Dystrophy Type 1 or Steinert's disease. Adv Exp Med Biol. 2012;724:239-57.
Smith CA, Gutmann L. Myotonic Dystrophy Type 1 Management and Therapeutics. Curr Treat Options Neurol. 2016 Dec;18(12):52.
Vydra DG, Rayi A. Myotonic Dystrophy. 2021 Feb 11. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan–. PMID: 32491378.
Wahbi K, Furling D. Cardiovascular manifestations of myotonic dystrophy. Trends Cardiovasc Med. 2020 May;30(4):232-238.
FAQs from users: 'Does Steinert's disease reduce life expectancy?', 'Is it true that Steinert myotonic dystrophy causes problems with anesthesia?' and 'Is there any alternative to PGD to prevent the transmission of genetic diseases?'.
Authors and contributors
More information about Cristina Algarra Goosman





Hello, is there any way to prevent the disease from developing? I was diagnosed late and by that time I already had my daughter. I don’t want her to go through it like me
Hello Yohana,
Steinert’s myotonic dystrophy is a monogenic disease, i.e. it affects only one gene. If your daughter has an alteration in this gene, she will inevitably present this disease.
It is recommended that you see a doctor so that he can evaluate her DNA and identify the DMPK gene to see if there is an alteration or not.
In the case of future children, it is possible to perform a preimplantation genetic test in which the malformation could be identified and, if present, the embryo transfer could not be performed.
I hope I have helped you.
Best regards.