In the first trimester of pregnancy, nausea and vomiting are normal, especially in the early morning hours. However, when this nausea is intense and constant during pregnancy, it is hyperemesis gravidarum.
This condition may begin around 6-8 weeks of gestation but usually subsides by week 20. Hyperemesis gravidarum can have negative effects on the mother's health and that of the baby, so it must be treated appropriately.
Provided below is an index with the 9 points we are going to expand on in this article.
- 1.
- 2.
- 3.
- 4.
- 5.
- 5.1.
- 6.
- 6.1.
- 6.2.
- 6.3.
- 6.4.
- 7.
- 8.
- 9.
What is Hyperemesis gravidarum?
When a woman is pregnant, morning sickness and vomiting are common (although they can occur at any time of the day). These symptoms occur most frequently during the first trimester of gestation and are generally thought to be due to a rapid increase in human chorionic gonadotropin (hCG) or estrogen.
Hyperemesis gravidarum would be a complication of this situation, so typical of pregnancy, which occurs in 0.3% to 3.6% of cases. It is the presence of intense and constant nausea and vomiting during pregnancy, which leads to avoidance of food intake and weight loss.
Hyperemesis gravidarum may begin to occur around 6-8 weeks of pregnancy, with symptoms being most pronounced around week 12. However, this condition tends to improve after the 20th week, although its duration may be prolonged.
If not properly treated, hyperemesis gravidarum can endanger and affect the health of both mother and baby.
Risk Factors
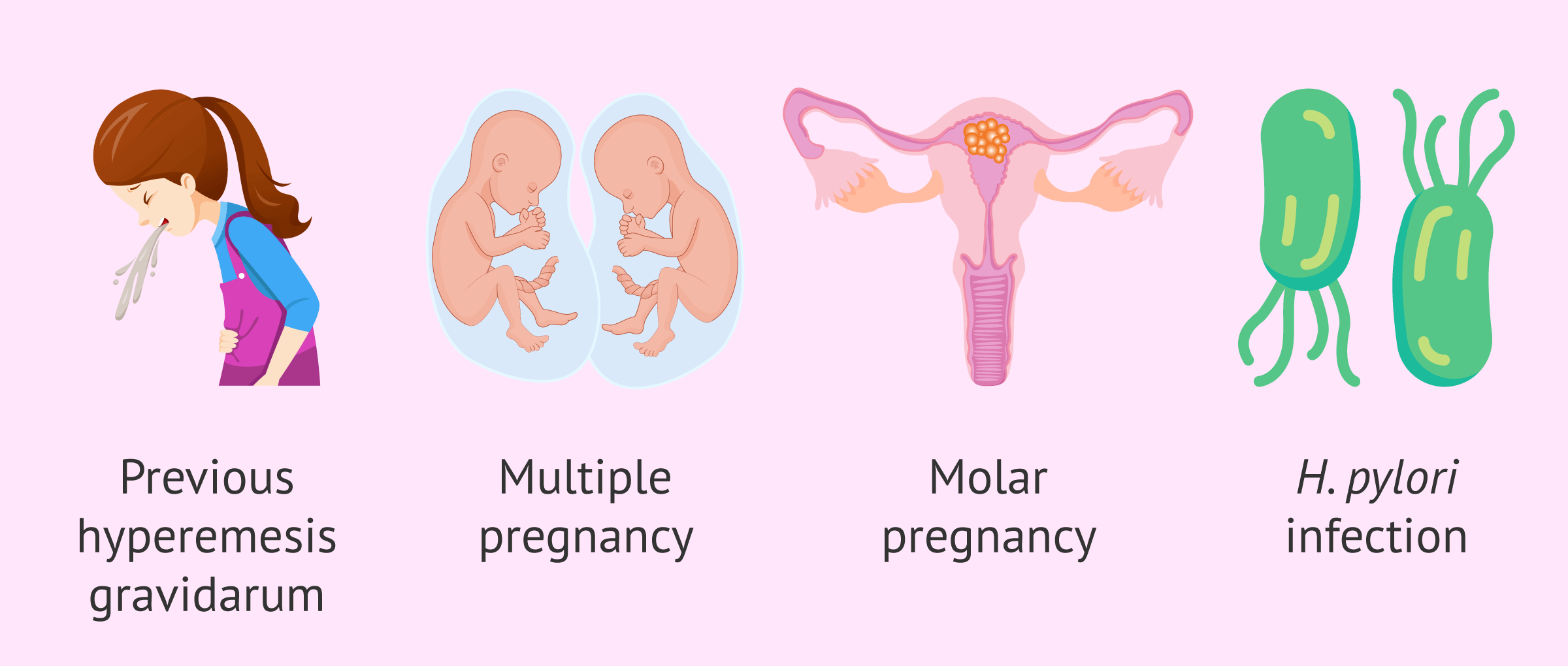
There are several factors that could increase the chances of developing hyperemesis gravidarum. Among them are:
- Hyperemesis gravidarum in a previous pregnancy.
- Twin or multiple pregnancy.
- Molar pregnancy or hydatidiform mole.
- Helicobacter pyloriinfection.
On the other hand, other risk factors such as obesity, pre-existing diabetes, young age and not having had children previously have also been proposed.
Symptoms
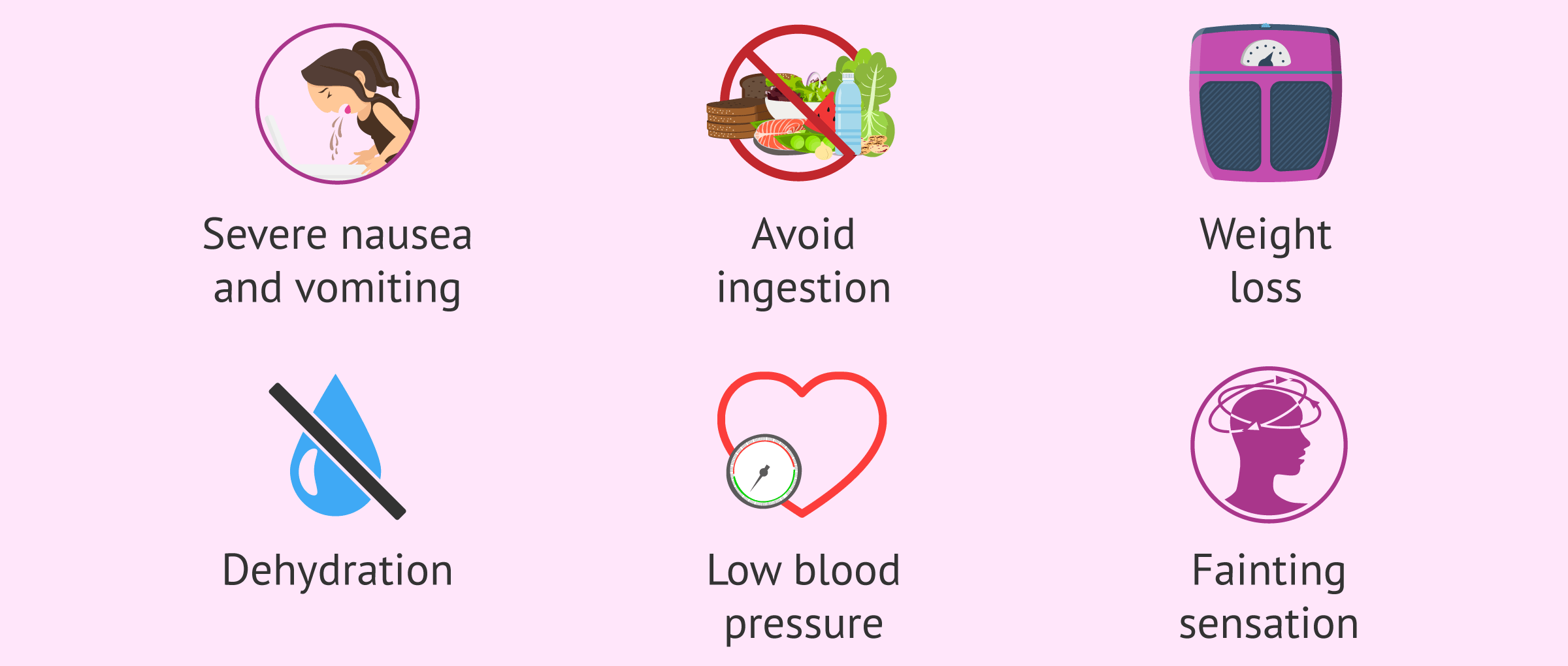
As mentioned, the main symptom of hyperemesis gravidarum is severe nausea and vomiting that persists during pregnancy. However, this situation can lead to the woman presenting:
- Inability to eat and/or drink.
- Weight loss greater than 5%.
- Dehydration.
- Malnutrition.
- Low blood pressure (hypotension) and increased heart rate (tachycardia).
- Alterations in the electrolyte balance of salts in the body.
- Fatigue, dizziness and even fainting.
- Temporary hyperthyroidism.
- Excessive salivation.
In addition, due to the lack of nutrients and vitamins caused by hyperemesis gravidarum, the pregnant woman may develop anemia and other serious complications such as Wernicke's encephalopathy. On the other hand, damage to the esophagus can also occur from constant vomiting, which can lead to blood in the vomit.
Finally, as for the effects on gestation, hyperemesis gravidarum has been associated with preterm delivery, having a smaller baby than would be appropriate for its gestational age, and with low birth weight.
However, it is also very important to mention that constant vomiting and nausea reduce a woman's quality of life. The pregnant woman limits her activities and social contacts and may show symptoms of depression and anxiety. For this reason, support from family, friends, and, if necessary, psychological support is necessary. It should be understood that hyperemesis gravidarum is not usual nausea and vomiting.
Diagnosis
The diagnosis of hyperemesis gravidarum is made on the basis of the patient's symptoms and weight loss. However, certain tests such as urine and blood test will also be performed to evaluate the woman's condition and to rule out other possible causes of vomiting.
In addition, the physician should perform an ultrasound in case there is a multiple or molar pregnancy.
Treatment
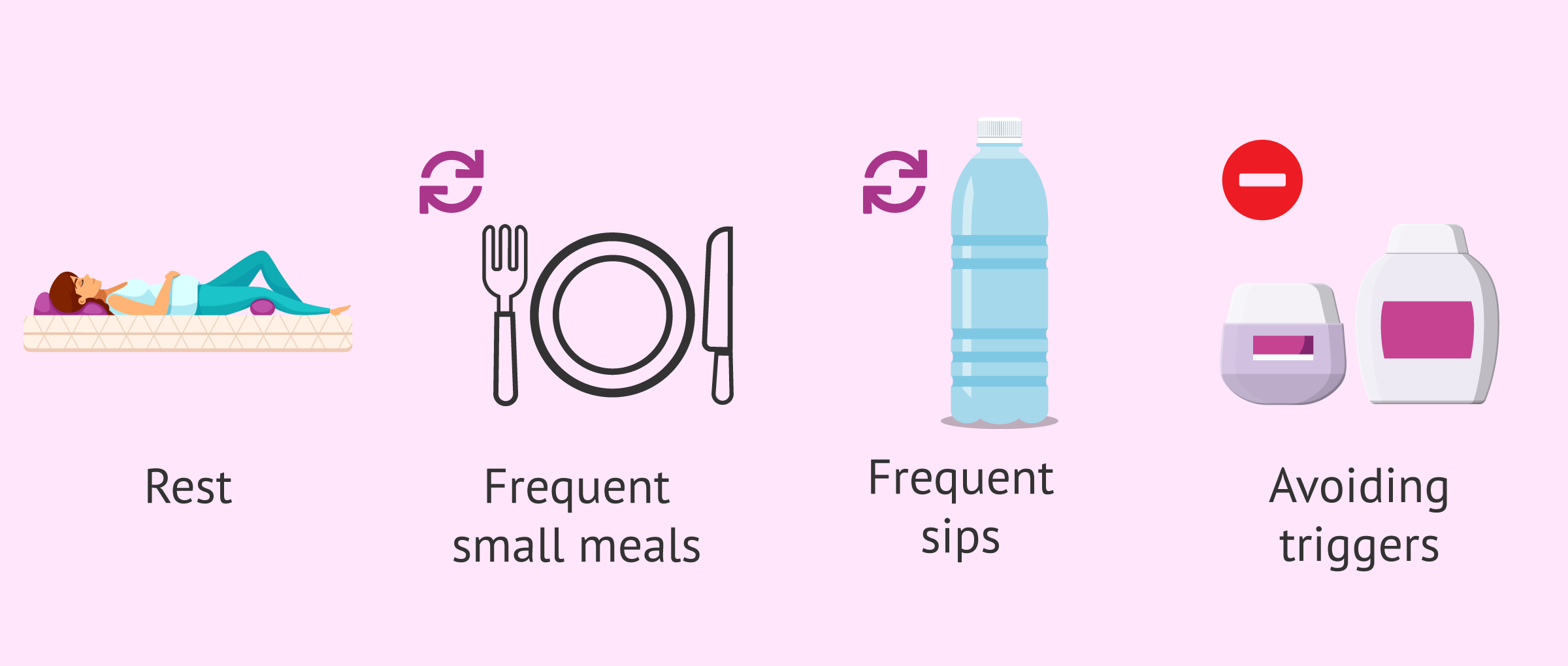
As for the treatment of hyperemesis gravidarum, initially the woman can try certain remedies such as the following:
- Rest.
- Eat little and often.
- Avoid excessively spicy foods, as well as fried foods.
- Drink plenty of fluids, but little by little. If the liquid causes the pregnant woman to vomit, fruits may be another option.
- Try to detect certain triggers of vomiting, such as odors or certain foods, and avoid them.
However, it is common that this advice is not sufficient and does not alleviate nausea and vomiting in pregnant women with hyperemesis gravidarum. Therefore, it is relatively common for a woman to visit her doctor when she has already lost weight and shows signs of dehydration.
Medical treatment
When the pregnant woman arrives at the hospital, the specialist will generally instruct the woman to stop eating and intravenous fluids will be administered.
In addition, electrolyte replacement and the administration of vitamins and antiemetics (drugs to reduce nausea and vomiting) are necessary according to the woman's needs and requirements. For this reason, the patient may require hospitalization for several days.
Once this is done, when the situation is more under control, the pregnant woman can gradually resume fluid intake. If these are tolerated, certain foods will be introduced in small quantities.
However, if the woman does not improve, other interventions such as tube feeding may be performed. In addition, in certain more extreme cases, the specialist may even propose a therapeutic termination of pregnancy.
FAQs from users
How much vomiting is considered hyperemesis gravidarum?
The number of vomiting is not what determines having hyperemesis gravidarum. If in doubt, a professional should be consulted for evaluation.
Read more
Is hyperemesis gravidarum common in the second trimester?
Hyperemesis gravidarum usually appears around 6-8 weeks of gestation, which would correspond to the first trimester of pregnancy. However, hyperemesis gravidarum has a duration that does involve the second trimester, as it often begins to subside around the 20th week of gestation.
On the other hand, if the onset of vomiting is late in the second trimester, the specialist should carefully rule out other possible causes before diagnosing hyperemesis gravidarum.
Can hyperemesis gravidarum lead to sick leave?
Yes, hyperemesis gravidarum is characterized by intense and constant nausea and vomiting, affecting the woman's quality of life and the performance of daily activities. In addition, weight loss and dehydration can even lead to hospitalization of the pregnant woman.
Is hyperemesis gravidarum the same as morning sickness?
No. Morning sickness, so-called even though it can occur at any other time of the day, is very common in pregnant women and can occur in up to 80-90% of pregnancies.
Hyperemesis gravidarum is a less common form of nausea and vomiting during pregnancy, occurring in 0.3 to 3.6% of cases. However, it is a more severe condition, as the vomiting is constant and intense and can lead to weight loss and dehydration of the pregnant woman.
Recommended readings
In this article, molar pregnancy has been mentioned as a possible risk factor for hyperemesis gravidarum. If you want to read more about this topic, we recommend you to visit the following link: Molar pregnancy or hydatidiform mole: types, symptoms, and diagnosis.
On the other hand, we have also mentioned that hyperemesis gravidarum has been related to premature delivery. For more information, you can read this article: What causes preterm labor - Risks, causes and symptoms
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Austin K, Wilson K, Saha S. Hyperemesis Gravidarum. Nutr Clin Pract. 2019 Apr;34(2):226-241. (See)
Boelig RC, Barton SJ, Saccone G, Kelly AJ, Edwards SJ, Berghella V. Interventions for treating hyperemesis gravidarum. Cochrane Database Syst Rev. 2016 May 11;(5):CD010607. (See)
De Haro K, Toledo K, Fonseca Y, Arenas D, Arenas H, Leonher K. Hiperemesis gravídica: manejo y consecuencias nutricionales; reporte de caso y revisión de literatura [Hyperemesis gravidarum: management and nutritional implications; case report and review of literature]. Nutr Hosp. 2014 Oct 3;31(2):988-91. Spanish. (See)
Jansen LAW, Koot MH, Van't Hooft J, Dean CR, Bossuyt PMM, Ganzevoort W, Gauw N, Van der Goes BY, Rodenburg J, Roseboom TJ, Painter RC, Grooten IJ. The windsor definition for hyperemesis gravidarum: A multistakeholder international consensus definition. Eur J Obstet Gynecol Reprod Biol. 2021 Nov;266:15-22. (See)
Lowe SA, Armstrong G, Beech A, Bowyer L, Grzeskowiak L, Marnoch CA, Robinson H. SOMANZ position paper on the management of nausea and vomiting in pregnancy and hyperemesis gravidarum. Aust N Z J Obstet Gynaecol. 2020 Feb;60(1):34-43. (See)
Lowe SA, Steinweg KE. Review article: Management of hyperemesis gravidarum and nausea and vomiting in pregnancy. Emerg Med Australas. 2022 Feb;34(1):9-15. (See)
Nijsten K, Dean C, van der Minnen LM, Bais JMJ, Ris-Stalpers C, van Eekelen R, Bremer HA, van der Ham DP, Heidema WM, Huisjes A, Kleiverda G, Kuppens SM, van Laar JOEH, Langenveld J, van der Made F, Papatsonis D, Pelinck MJ, Pernet PJ, van Rheenen-Flach L, Rijnders RJ, Scheepers HCJ, Vogelvang T, Mol BW, Roseboom TJ, Koot MH, Grooten IJ, Painter RC. Recurrence, postponing pregnancy, and termination rates after hyperemesis gravidarum: Follow up of the MOTHER study. Acta Obstet Gynecol Scand. 2021 Sep;100(9):1636-1643. (See)
Sharma V. Treatment of Depression in a Patient With Intractable Hyperemesis Gravidarum. Prim Care Companion CNS Disord. 2021 Dec 16;23(6):20cr02905. (See)
Varela P, Deltsidou A. Hyperemesis gravidarum and neonatal outcomes: A systematic review of observational studies. Taiwan J Obstet Gynecol. 2021 May;60(3):422-432. (See)
FAQs from users: 'How much vomiting is considered hyperemesis gravidarum?', 'Is hyperemesis gravidarum common in the second trimester?', 'Can hyperemesis gravidarum lead to sick leave?' and 'Is hyperemesis gravidarum the same as morning sickness?'.
Authors and contributors
More information about Cristina Algarra Goosman




Hi, I’m 15 weeks and I thought that throwing up so much and having such a bad time was typical of pregnancy. I am relieved to have read that there is something else.
Hi MarthaLowes,
Indeed, despite the conceptions that are held about nausea during pregnancy this can be pathological causing an inability to lead a normal life.
I recommend that you see your doctor so that he/she can diagnose you and prescribe treatment to mitigate the symptoms.
I hope everything goes well,
Best regards
Hi, I have lost a lot of weight since I got pregnant and I have been vomiting but I can’t tell if it’s anything out of the ordinary. It is true that it makes it impossible for me to keep food in my body but I don’t know if it is something out of the ordinary.
Hello Annah,
Weight loss in pregnancy can be due to different causes, in general, it is recommended to maintain or gain weight over the course of pregnancy as this constitutes part of the weight of the fetus and placenta.
Food during pregnancy is also an important point since it is necessary to have good nutrition that favors the proper development of pregnancy. An increase of 300-500 calories is recommended in the second-third trimester of pregnancy.
If you have lost a lot of weight and you cannot keep the food in your body, I recommend that you go to your doctor to establish a nutritional plan that ensures proper nutrition for both of you.
I hope everything is goes well