Oligospermia or oligozoospermia is a sperm disorder that causes a low sperm count in the ejaculated semen.
Since oligospermia has no symptoms associated, it is typically detected when the affected male has been trying to conceive for a long period of time without success.
Fertility specialists can diagnose oligozoospermia using the following tests
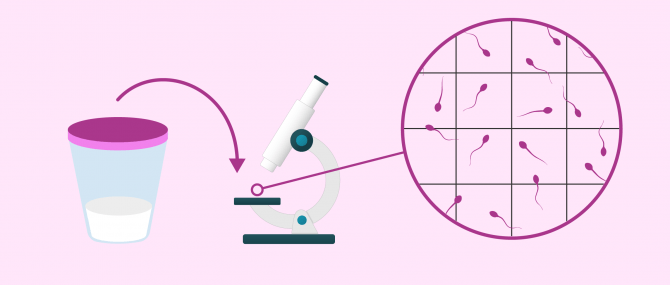
- Semen analysis
- also called sperm test or seminogram, it is used to evaluate sperm parameters microscopically.
- Bloodwork
- provides information about sex hormone levels and potential abnormalities.
Provided below is an index with the 7 points we are going to expand on in this article.
- 1.
- 1.1.
- 1.2.
- 2.
- 2.1.
- 3.
- 4.
- 4.1.
- 4.2.
- 4.3.
- 4.4.
- 4.5.
- 4.6.
- 4.7.
- 5.
- 6.
- 7.
Semen analysis
A semen analysis is the main diagnostic test used in Andrology labs to assess sperm quality. Aside from the sperm count, it also provides information on sperm motility, morphology, vitality, etc.
To perform a semen analysis and maximize the accuracy of the results, about 3 to 5 days of sexual abstinence are required. Then, the sample is produced through masturbation at the fertility clinic. The ejaculate is collected in a sterile container and taken directly to the laboratory for analysis.
A semen sample is diagnosed with oligospermia when the sperm count is below 15 million sperm per milliliter.
The sample is first left to liquify in the lab, then the macroscopic and microscopic examinations can begin.
Macroscopic analysis
Firstly, the semen is examined with the naked eye in order to evaluate the following parameters, always taking as a reference the guidelines of the World Health Organization (WHO):
- Volume: over 1.5 ml
- pH: between 7.2 and 8.0
- Color: white or whitish gray, sometimes a bit yellowish
- Consistency: sticky, jelly-like liquid, without lumps or strands
- Liquefaction time: 20 minutes
If the volume of a semen sample is under 1.5 ml, it might be a case of hypospermia. This sperm disorder could aggravate oligospermia, since a reduced amount of semen correlates with a poor sperm count.
Fertility treatments, like any other medical treatment, require that you trust the fertility specialists that will be by your side during your journey. Logically, each clinic has a different work methodology. Our Fertility Report will offer you a selection of recommended clinics, that is, fertility centers that have passed our rigorous selection process. Moreover, our system is capable of comparing the costs and conditions of each one so that you can make a well-informed decision.
Microscopic analysis
Secondly, the sperm sample is examined under the microscope to see the characteristics of spermatozoa that cannot be seen by the naked eye:
- Sperm count: more than 15 million/ml
- Motility: more than 32% with progressive motility, or 40% total motility
- Morphology: 4% of sperm with normal shape
- Vitality: 58% live sperm
- Leukocytes (WBCs): fewer than 1 million/ml
According to the WHO's reference values, a man has a good sperm count if it is above 15 million/ml. Values lower than this mean the sample would be qualified as oligospermic. Despite presenting with a low sperm count, a natural pregnancy may be possible as long as the rest of the seminal parameters are within the normal ranges.
However, it is possible that aligospermia may be accompanied by other seminal alterations. Thus, if both sperm count and motility are compromised, the diagnosis would be oligoasthenospermia. Conversely, if count and morphology present alterations, it would be a case of oligoteratozoospermia.
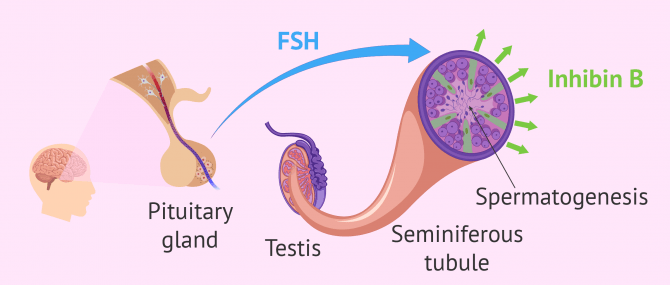
Hormonal analysis
Once oligospermia has been diagnosed with a semen analysis, a blood test can help us find the cause behind it.
The main hormones that regulate male fertility are:
- FSH
- produced by the pituitary gland, its function is to stimulate the production of sperm in the testicle. High FSH levels indicate that something is wrong with spermatogenesis and fewer sperm than expected are being produced. Normal FSH levels range from 1.0 to 12.0 mIU/ml.
- Inhibin B
- Produced in the testis, its function is to regulate spermatogenesis, causing FSH levels to diminish. Thus, elevated inhibin B levels indicate that sperm production is occurring with normality. The normal inhibin B level is 140 pg/ml.
To sum up, there exists an inverse correlation between FSH and inhibin B levels.
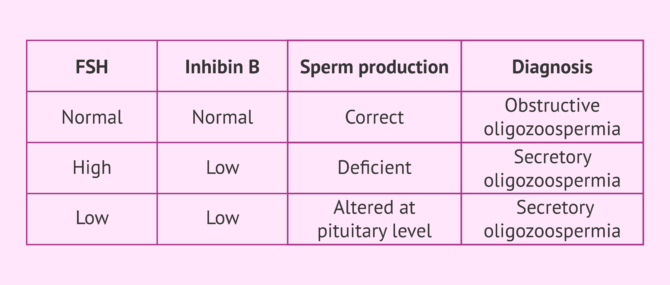
Interpretation of results
Depending on the results of these hormones, we can expect any of the following outcomes:
- Normal FSH and inhibin B levels
- Sperm production occurs as expected. Thus, it might be a case of obstructive oligospermia: there may exist a blockage in the vasa deferentia, epididymis, or urethra that impedes the exit of the sperm in the ejaculate, even though they are produced normally.
- Elevated FSH and decreased inhibin B levels
- Defective spermatogenesis due to a reduced amount of stem cells in the testicle. This points to a case of secretory or (non-obstructive) oligospermia.
- Decreased FSH and inhibin B levels
- spermatogenesis is affected by a hormonal alteration at the pituitary level, but it could be stimulated with drugs such as clomiphene citrate. This happens in males with secondary hypogonadism.
In addition to the semen analysis and a blood test, a physical exploration is also indispensable in order to detect potential abnormalities in the testicles, including cryptorchidism, varicocele and so on, which can also affect sperm production.
Medical history
Finally, to conclude the interpretation of results, patients are asked to complete a form that helps the fertility specialists determine the cause of infertility.
Some interesting aspects that help the specialist to render an accurate diagnosis are:
- For how long the patient has had infertility, and if there have been previous pregnancies or children born
- Professional career and potential exposure to environmental toxic substances
- Family history of genetic diseases or abnormalities
- Medication intake
- Lifestyle habits: diet, sports, tobacco, alcohol, etc.
- Childhood diseases: mumps or meningitis
- Possible trauma, infections, surgical procedures and so on.
Simply put, any data that may go unnoticed by the patient at first could turn out to be crucial for the diagnosis of oligospermia or any other male fertility problem.
FAQs from users
What is the importance of hormonal analysis in the diagnosis of oligozoospermia?
It is essential to look for the reason for the oligozoospermia, since knowing the origin, it will be possible to establish the treatment. This is especially useful in hormonal disorders, which justifies performing hormonal determinations in cases of low sperm count to try to find the cause of this problem and solve it.
Read more
Does oligozoospermia always end up as azoospermia?
Oligozoospermia is the presence of an abnormally low number of spermatozoa in the ejaculate.
Patients with oligozoospermia, especially in cases of severe oligozoospermia, may progress to a diagnosis of cryptozoospermia and subsequently to azoospermia, i.e., absence of sperm in the ejaculate.
The diagnosis of oligozoospermia must be associated with tests to evaluate the origin of this oligozoospermia and to be able to anticipate its evolution. In this way, an early diagnosis makes it possible to establish an adequate treatment (hormonal, antioxidants, etc.). Likewise, patients with moderate or severe oligozoospermia are usually recommended to cryopreserve a semen sample in order to foresee a possible absence or decrease in sperm quality.
What are the causes of a low sperm count in the ejaculate?
It can be due to a number of causes that can cause oligospermia, and some of them are not easily detectable. Generally, they can be classified into pre-testicular, testicular, and post-testicular causes, based on whether there exists an alteration in the hormone levels, a testicular issue or blockage, respectively.
Read more: Causes of Oligospermia.
How many types of oligospermia exist?
Based on the number of sperm under the reference value of 15 million sperm per milliliter, there exist three degrees of severity:
- Mild oligospermia: 14-5 million/ml
- Moderate oligospermia: 5-1 million/ml
- Severe oligospermia: <1 million/ml
Learn more: Types of Oligospermia.
What is extreme or very severe oligospermia?
Extreme or very severe oligospermia is diagnosed when the number of sperm per milliliter of ejaculated semen seen under the microscope is fewer than 1 million.
Is oligozoospermia the same as cryptozoospermia?
Both seminal alterations are characterized by a low quantity of spermatozoa in the ejaculate with respect to the reference value considered normal by the World Health Organization (WHO).
A male has oligozoospermia when he has less than 15 million sperm per mL of ejaculate. On the other hand, the diagnosis is cryptozoospermia when the value of sperm concentration in the ejaculate is less than 100,000 spermatozoa per mL.
What symptoms are associated with low sperm count?
There are no particular symptoms linked to oligospermia. There exist no visible or noticeable symptoms such as pain, which means males are unable to know they have oligospermia until they find out with a semen analysis. In short, couples find it out when pregnancy does not occur after having been trying to conceive for a reasonable period of time and decide to undergo infertility testing.
Recommended reading
The semen analysis is the most important of all laboratory tests for males. To get more information about this diagnostic test you can visit the following link: What Is a Semen Analysis Report? – Purpose, Preparation & Cost.
The treatment chosen to attempt to regain fertility will depend of the cause of oligospermia. If you are interesting in reading about treatment options we recommend reading this article: Treatment of Oligospermia.
Sex hormones play an important part in the regulation of the reproductive function. To learn more about the processes involved with male hormones you can click on the following link: Male hormone analysis: what should the normal hormone levels be?
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Guzick DS, Overstreet JW, Factor-Litvak P, Brazil CK, Nakajima ST, Coutifaris C, et al. (2001). Sperm morphology, motility, and concentration in fertile and infertile men. N Engl J Med 2001; 345: 1388-1393.
McLachlan RI. Approach to the patient with oligozoospermia. J Clin Endocrinol Metab. 2013;98(3):873-80.
Sigman M, Zini A. (2009). Semen analysis and sperm function assays: what do they mean? Semin Reprod Med; 27: 115-123
World Health Organization (WHO) (1999). Laboratory manual of the WHO for the examination of human semen and sperm-cervical mucus interaction. Annali dell'Istituto Superiore di Sanita.
World Health Organization (WHO) (2010). WHO laboratory Manual for the examination of human semen and sperm-cervical mucus interaction. Cambridge Academic Press.
FAQs from users: 'What is the importance of hormonal analysis in the diagnosis of oligozoospermia?', 'Does oligozoospermia always end up as azoospermia?', 'What are the causes of a low sperm count in the ejaculate?', 'How many types of oligospermia exist?', 'What is extreme or very severe oligospermia?', 'Is oligozoospermia the same as cryptozoospermia?' and 'What symptoms are associated with low sperm count?'.
Authors and contributors

More information about Michelle Lorraine Embleton





Hi
Which tests are done first? The semen analysis or the blood tests?