Gestational surrogacy, also known as host surrogacy or full surrogacy, is a fertility procedure that allows all family types to become parents. This type of surrogacy involves using an egg donor and a gestational carrier (hereinafter, GC) for IVF, which involves using the oocytes of a person other than the surrogate. The process is more complex and involves more parties, but has the advantage that the surrogate is not genetically linked to the child.
For host surrogacy to be successful and in order to reduce the number of risks for everyone, intended parents (hereinafter, IPs) are strongly advised to seek legal counsel, which is dependent on the laws on surrogacy established by each country to a large extent. In general, using a gestational carrier is today's trend, as it makes it easier for the parties involved, thereby increasing the success rates and paying attention to the child's best interest above all.
Provided below is an index with the 7 points we are going to expand on in this article.
- 1.
- 1.1.
- 1.2.
- 2.
- 2.1.
- 2.2.
- 3.
- 4.
- 5.
- 6.
- 6.1.
- 6.2.
- 6.3.
- 6.4.
- 6.5.
- 6.6.
- 6.7.
- 6.8.
- 6.9.
- 6.10.
- 7.
Definition and process
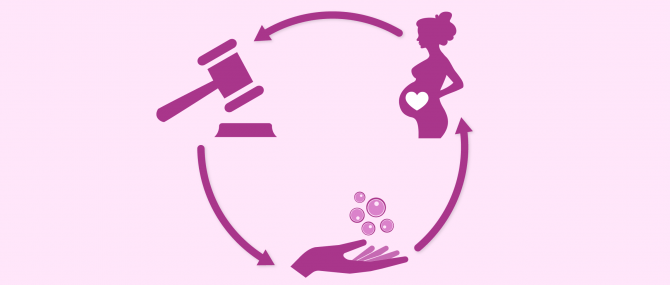
The meaning of the term surrogacy is simple: a woman other than the intended mother carries and gives birth to a baby for a couple that wishes to create a family but cannot achieve so by their own means. Through a legal contract, the surrogate agrees to relinquish the child to the commissioning parents.
Also known as full surrogacy, the fact that there are more parties involved makes the IVF process a more complex one from a technical point of view, but it is however the most widely used type because it does not involve the carrier's DNA with that of the child.
As mentioned earlier, the surrogate is not the person contributing the egg, but only the one who carries the pregnancy to term and gives birth to the baby. Keeping this in mind, it is the intended mother (in the case of straight couples without egg production problems) or the egg donor (a third party) who undergoes ovarian stimulation for egg retrieval (i.e. ovum-pick up or follicle puncture).
To learn more about the process of follicle puncture to retrieve donor eggs, we recommend you to visit the following article: How are eggs harvested from a donor's ovaries?
Once obtained, the oocytes are fertilized in the laboratory with the sperms of the intended father or a sperm donor by means of in vitro fertilization (IVF). In case the partner's sperm cells are used, IVF with ICSI might be required depending on the quality of the semen sample.
Technically, the process followed is exactly the same as that followed for conventional IVF cycles. What is different, however, is the step at which the embryo transfer (ET) is carried out: it is the gestational carrier who has the embryo transferred to her uterus instead of the intended mother. This is the reason why the surrogate will have no genetic link with the baby.
Gestational vs. traditional surrogacy
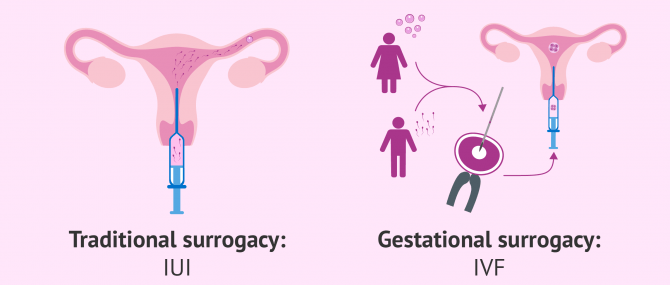
Surrogacy can be classified into two types in accordance with the method through which the pregnancy is achieved, as well as the extent to which the gestational carrier is related to the baby. Taking this into account, the differences between them are explained below:
- Traditional or partial surrogacy: Pregnancy is achieved by means of intrauterine insemination (IUI). In this case, the surrogate (commonly referred to as surrogate mother) is also the person contributing the eggs that will be fertilized. In other words: she is the biological and birth mother of the child.
- Gestational or full surrogacy: As explained above, the surrogate gets pregnant with IVF, that is, by transferring an embryo created with donor eggs and the partner's or donor sperm. The surrogate is not the biological mother of the child, as the IPs' or donor gametes have been used for oocyte fertilization.
Although IUI is simpler from the technical point of view, traditional surrogacy is becoming less used due to the creation of genetic ties between the baby and the surrogate mother. This can lead to the appearance of a number of ethical and legal complications in case the woman regrets it and wishes to keep the baby.
Success rates and statistics
In general, a single person or couple has a favorable prognosis with a gestational carrier. Statistical data has shown that, on average, families are able to bring home a baby within 14 to 18 months since they get started with the process.
However, determining the success rates for surrogacy is rather difficult, given the number of parties involved and the factors that might have an influence, including:
- The gestational carrier's ability to get pregnant
- The age of the intended mother or the egg donor
- The quality of the gametes used
- The success of IUI vs. IVF procedures
- The quality of the embryo(s) transferred
Out of all the factors listed above, the truth is, the most important one is the age of the woman providing the eggs, as the quality of a woman's oocytes diminishes over time.
Also, it should be borne in mind that gestational carriers are screened for a number of factors, including their state of health and fertility. For this reason, it is estimated that over half of all carriers become pregnant after the first IVF attempt. If not, the likelihood of getting pregnant on the second or third try is very high.
To learn more about the chances of success with IUI and IVF, visit any of the following links:
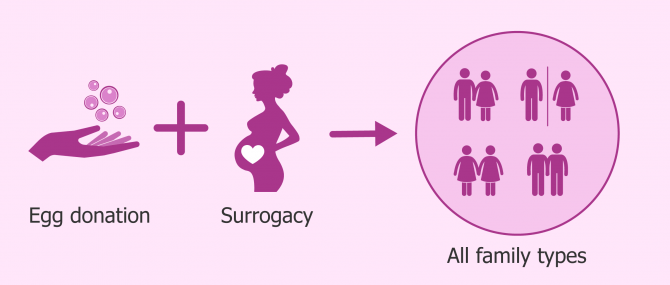
Intended parent profiles
Egg donation, also known as ovum donation or oocyte donation, and surrogacy are two fertility treatments that often go hand by hand. One may think that both methods can only be combined in the case of same-sex male couples.
However, the truth is that it becomes useful also for a great number of straight couples in which the woman is unable to use her eggs, and to carry the pregnancy to term for medical reasons.
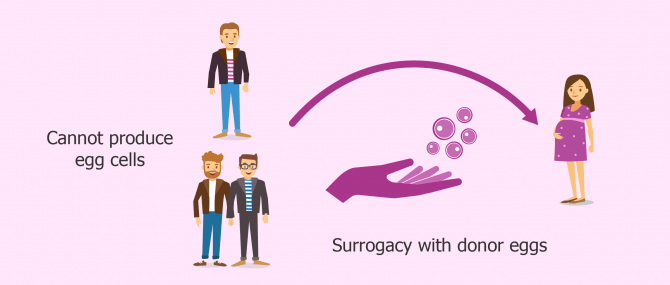
Gay and single parents
When a single man or same-sex male couple wish to have a baby using their own sperms, they have no alternative but to turn to donor eggs in order to bring the surrogacy process to an end.
In this case, it is not about a medical condition, but a biological inability. In other words, the reason why they cannot bear a pregnancy is solely the natural male anatomy, and not a health issue.
This is also the reason why many destination countries do not allow this group to undergo surrogacy, since the legal framework of some countries ask for a medical justification that proves you are actually unable to carry a pregnancy to term.
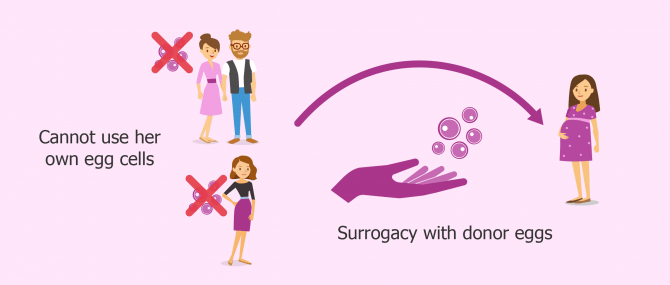
Heterosexual couples
The main reasons why a woman may need to use a gestational carrier because of her incapacity to bear a pregnancy to term are varied:
- Absent uterus, whether it is caused by a congenital or acquired dysfunction
- Uterine malformations
- Implantation failure
- Recurrent pregnancy loss (RPL)
- Certain diseases as to why pregnancy can put the health of the pregnant woman and/or the baby at risk
Some of the above mentioned abnormalities are associated with the absence of viable eggs. For instance, recurrent pregnancy losses and/or miscarriages may be caused by egg production problems, uterine alterations, or both. This is the reason why, in certain cases, egg donation can become the definitive solution; in other cases, however, a combination between egg donation and surrogacy may be necessary.
This also can be useful in cases where pregnancy can constitute a serious danger to the pregnant woman's life because the intended mother suffers from a particular disease, as it may compromise egg quality and/or quantity.
Women with an absent uterus due to cancer, the oncological treatment administered could have compromised egg production. In these cases, a combination between surrogacy and egg donation may be necessary.
Gestational surrogacy laws
The regulations governing surrogacy vary to a great extent from country to country, and even in the countries where it is allowed, as each one may have established different requirements and peculiarities:
- Certain policies force both intended parents to deliver their gametes for the creation of embryos in a surrogacy process, thereby ruling out the possibility of using donor eggs.
- Others allow for the use of donor gametes, whether it is only the egg, the sperm, or both, and regardless of whether the embryo transfer is done to the intended mother or the gestational carrier.
- Certain places have an intermediate regulation, which is to say, it allows for the use of one donor gamete, but the other one must be delivered by one of the intended parents.
Egg donor identity is another crucial aspect. While some policies establish that donor and surrogate must be two different people, other countries allow traditional surrogacy as well, in which the surrogate herself delivers the eggs apart from being the gestational carrier.
Finally, we come back to the point related to a woman's incapacity to bear an effective pregnancy. Certain destination countries allow patients to undergo surrogacy provided that they can justify their inability to carry a pregnancy to a live birth. Others, conversely, allow surrogacy to everyone wishing to have a baby through this technique, regardless of the reason that impelled them to pursue surrogacy.
How much does it cost?
Depending on the type of surrogacy chosen and the country where it is carried out, the cost of treatment might be higher or lower. Nevertheless, what is true is that surrogacy is the most expensive of all infertility treatments available nowadays. On average, the total cost ranges from €35,000 to €150,000.
This sum can be broken down into various fees, including:
- Compensation to the gestational carrier
- Compensation to the egg donor
- In vitro fertilization
- Fertility medications
- Agency fees
- Legal fees
- Fertility clinic fees
- Travel and accommodation costs
In most of the cases, carriers are economically compensated. The average compensation payment given to surrogates ranges from €10,000 to 40,000, depending on the country where it is done. Also, the fact that the surrogate has previous experience or not might add to this sum.
The medical expenses derived from the pregnancy should be added as well: gynecological consultations, ultrasounds, medications, etc. Maternity clothes as well as visits to the clinic are on the intended parent's expense, too. Some insurance companies cover medical expenses derived from surrogacy arrangements, though.
Bioethical considerations and potential risks
The main argument against gestational surrogacy is that carriers can be perceived as just a "womb for rent", available for those who want to create their own family. For some groups, this practice is morally unacceptable.
Critics denounce the use of a woman's body with commercial purposes, as if it were nothing but a machine or an incubator. To sum up, they see it as an open door to exploitation and manipulation of females, especially in those cases where the GC is facing a poor economic or familiar situation.
Conversely, proponents argue that potential surrogates are free to choose what they want to do with their own bodies, as long as they take responsibility for their acts and decisions. A gestational surrogacy agreement should be signed voluntarily and freely, which leaves no room for exploitation or commercialization.
In addition to ensure the welfare of the child, gestational carriers should be pre-screened and psychologically evaluated in order for their state of health and personal circumstances to be analyzed. Taking care for her is essential and, in this sense, betting on single embryo transfers (SETs) to avoid the risk for a twin pregnancy is crucial.
Finally, the fact of getting pregnant and giving up the baby does not necessarily translate into a negative impact on the GC's mental and physical integrity. While some surrogates do feel attached to the baby only during pregnancy, there are others who reject the fetus, and a third group that develops no feeling of attachment during the process.
FAQs from users
In which cases should you use a surrogate to have a baby?
In general, the two reasons for the use of surrogacy are the absence or abnormality of the uterus or a medical contraindication.
Cases of absent/abnormal uterus:
- MRKH syndrome. Mayer-Rokitansky-Küster-Hauser syndrome is a disorder where the female is born with an underdeveloped or absent uterus and vagina.
- History of hysterectomy – a surgery to remove the uterus
- Multiple fibroid tumors of the uterus that cannot resolved by a surgery
- Severe intrauterine scarring (Asherman’s syndrome) irreparable
- A single male or gay male couple
- Unexplained recurrent pregnancy loss or unsuccessful embryo implantations
- Inability to develop the uterine lining (endometrium)
Cases of medical contraindications (relative and absolute):
- A serious medical condition that worsens with pregnancy posing risk to mother and fetus
- Pulmonary hypertension
- Turner’s syndrome
- Uterine cancer
Can two males have a biological child with the DNA of both in a single pregnancy?
Currently, fertilization of an egg only occurs by one sperm cell that is produced from one man.
What are the different types of surrogacy?
There are two types of surrogacy:
- Traditional surrogacy involves the woman who will carry the pregnancy also to be the source of the egg. She usually will ovulate naturally and undergo intrauterine insemination (IUI). Countries vary in their laws overseeing this arrangement so it is imperative that you consult, in advance of your treatment cycle, with an attorney who is well versed in this area.
- IVF surrogacy is the process of using an egg donor and a separate gestational carrier. Following hormonal stimulation of the egg donor and egg retrieval, the eggs are fertilized with the sperm of one or both partners in a reproductive laboratory through IVF. The embryo is then transferred into the gestational carrier’s uterus, previously prepared hormonally to synchronize optimal receptivity. The resulting baby is genetically unrelated to the carrier.
Is it true that a number of celebrities have turned to a gestational carrier to have a baby?
Yes, gestational surrogacy is a fact for many celebrities, especially those aged between 35 to 50. Also, in the case of same-sex couples and single men, gestational surrogacy with egg donation has allowed them to create a family. Examples include Elton John, Matt Bomer, Cristiano Ronaldo, Ricky Martin...
If you want to find out which stars have turned to an egg donor and/or a gestacional carrier to have a baby, do not miss the following post: Celebrities who used donor eggs or a surrogate.
Is gestational surrogacy allowed in India?
Yes, host surrogacy is allowed in this country, but only for Indian people, foreign residents, or foreign people married to an Indian citizen. Also, only married heterosexual couples that have been married for at least 5 years have access to it.
These regulations were approved in October, 2015 due to the massive arrival of foreign couples and persons willing to undergo surrogacy in India. As for the GC, she must be a member of the family. Especial emphasis should be put on the fact that traditional surrogacy is not allowed in any case, as a requirement is that she has no genetic link to the child.
What's the difference between 'egg donor' and 'gestational carrier'?
An egg donor is the woman who donates her oocytes for an embryo to be created from them. She replaces the intended mother's uterus in the case of heterosexual couples, and contributes the female cell to the fertilization process. This means she is the biological mother of the child, and therefore the one who passes her DNA to the baby.
A gestational carrier is the woman who carries the pregnancy to term and gives birth to the baby for the intended parents. She is not biologically linked to the resulting baby.
Do babies from egg donation share genes with the birth mother?
Egg donor babies do not share the genetic load of the birth mother, but that of the egg donor, who is in fact the biological mother.
Nevertheless, recent studies have shown that recipients of donor eggs still pass some traits of their DNA through a phenomenon called epigenetics, a branch of Biology that studies the influence of a person's lifestyle on who he or she is, regardless of the gene expression.
So, factors such as the mother's diet during pregnancy could affect the development of the baby-to-be's gene expression.
If I use donor eggs, will the baby be mine?
Absolutely. Having a child is not only about sharing your DNA with him or her, but about educating, bringing up and enjoying life together as a family. Women who become mothers via egg donation love the baby exactly as any other female who got pregnant naturally with her own eggs would do. Having a child, no matter how you do it, is one of the most gratifying and rewarding experiences in life.
So, those women who are afraid of developing feelings of regrets once pregnant or after the birth of the child should know that this idea will disappear eventually.
Is South Africa a good destination for intended parents willing to undergo gestational surrogacy abroad?
Certainly not. Despite surrogacy is allowed in South Africa, a requirement established by the law is that only residents are allowed to undergo it. If a foreign citizen or couple travels to South Africa for gestational surrogacy, the agreement would be illegal. Thus, it is an unsafe destination for surrogacy overseas.
Can I use my eggs for gestational surrogacy?
Yes, if the intended mother produces healthy eggs, there is no reason why they should be rejected. Donor eggs are used only in cases where, in addition to the incapacity to bear an effective pregnancy, the intended mother suffers from infertility.
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
FAQs from users: 'In which cases should you use a surrogate to have a baby?', 'Can two males have a biological child with the DNA of both in a single pregnancy?', 'What are the different types of surrogacy?', 'Is it true that a number of celebrities have turned to a gestational carrier to have a baby?', 'Is gestational surrogacy allowed in India?', 'What's the difference between 'egg donor' and 'gestational carrier'?', 'Do babies from egg donation share genes with the birth mother?', 'If I use donor eggs, will the baby be mine?', 'Is South Africa a good destination for intended parents willing to undergo gestational surrogacy abroad?' and 'Can I use my eggs for gestational surrogacy?'.
Surrogacy process at the clinic we’ve been with is performed in the following steps:
The initial consultation is to be scheduled at least 1 week ahead and contains the following activities: A set of tests depending on the program (fasting is mandatory). Consultation with a fertility specialist who will be in charge of your program (in case of stimulation you will need to have the transvaginal ultrasound check done). Consultation with a manager who will guide you through the program step by step. The signing of contracts First payment (please note, if you are taking medications for stimulation from the clinic, the medications are to be paid in cash on the day of consultation). Before any initial consultation, you will receive the Guidelines for the Initial Consultation – failure to follow these recommendations may affect the initial consultation in a negative way.
After you sign contracts and make the first payment, the medical team starts the selection process that includes: Initial pre-selection by the local coordinator. Consultation of the fertility specialist. Consultation of a psychologist. Legal consultation and verification of documents. screening for possible addictions (urine and blood tests). – This check-up process, including all necessary tests and exams, takes about 1 month.
Then the cycle of egg donor or the biological mother is synchronized with the cycle of a surrogate mother. According to your contract, you have to follow all doctor’s instruction. In the case of self-treatment or violation of the treatment protocol, the clinic may cancel the cycle and terminate the contract. The date of the pick up is scheduled by the doctor in charge of the program.
If the Intended Parents wish to use a previously frozen sperm sample for fertilization they shall notify the program coordinator about that by email no later than 24 hours before the procedure. If it is the second/further attempt and more than 2.5 months has passed since your last blood test in the clinic, be ready to have your blood test repeated, and that means fasting in the morning. In case the biological mother undergoes hormonal stimulation and is being prepared for egg retrieval, the second visit may take up to 10 days If it’s surrogacy using own eggs it is not recommended to leave the same day. Flying the following day is fine.
The rules for sperm donation are similar as for the initial consultation. A man needs to abstain from ejaculation from 3 to 5 days before. The second payment (according to your contract) is to be made on this day if in cash, prior to this day if by the bank transfer. After fertilization, the embryo development is monitored by the embryology unit. The embryo transfer takes place on the 5th day as they are transferring the blastocysts. You will receive the protocol of embryo cultivation and transfer within 3 working days after the embryo transfer. The HCG test takes place 2 weeks after the embryo transfer. The surrogate mother has her test. The results of the test are known the day after the test. The first ultrasound scan is carried out in 2 weeks after the positive HCG test by the doctor in charge of the program. The report will be sent the same or the next day after the check.
Hello, need advice.
How to choose the right company that can do this? Which country is better, is there any rating?
Hello there,
Guess the best thing in these cases is to use a donor on the one hand and a surrogate on the other hand. I think it’s unavoidable that a surrogate mother would’t develop a certain level of attachment to the unborn child, let alone if she knows she’s genetically bound to the baby.
So, I think egg donation and surrogacy is the best possible combination!
Best