If we take into account that the average length of human pregnancy is 40 weeks (280 days), during the second week of pregnancy—counting from the date of the last menstrual period (LMP)—the body is still preparing to receive the embryo. Two major events take place: proliferation of the endometrium and ovulation.
Egg fertilization and embryo implantation have not taken place yet. In other words, technically conception per se hasn't occurred. Nevertheless, gynecologists start counting the weeks of pregnancy from the first day of the last menstrual period.
For this reason, during the first and second weeks of pregnancy, the woman is not yet pregnant. Some specialists prefer to refer to them as the countdown to conception or just the weeks before conception.
During these weeks, important changes also occur in a woman's body that are related to the beginning of pregnancy and, therefore, we should pay some attention to them.
Provided below is an index with the 7 points we are going to expand on in this article.
- 1.
- 1.1.
- 1.2.
- 2.
- 2.1.
- 3.
- 4.
- 4.1.
- 4.2.
- 4.3.
- 4.4.
- 5.
- 6.
- 7.
Changes in the uterus & ovaries
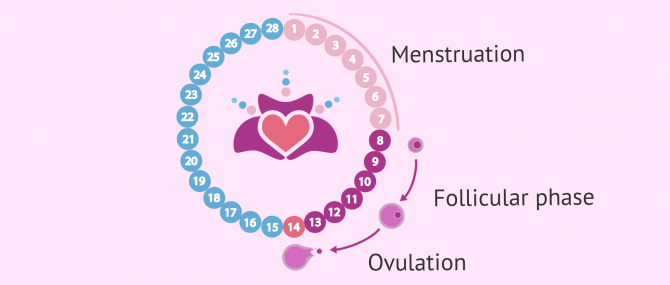
As mentioned above, the second week of pregnancy is actually the second week of the menstrual cycle. Particularly, it is the stage at which follicle recruitment takes place, hence the name preovulatory phase.
After the beginning of the menstrual cycle, which occurs during the first week of pregnancy, the pituitary gland starts producing FSH and LH, the hormones that make the ovaries work. LH and FSH surges occur during the second week, thereby causing the following phenomena:
Follicle recruitment
The FSH surge that occurs in the first two weeks of the menstrual cycle causes the ovarian follicles to grow and migrate to the surface of the ovary. At the same time, follicle growth causes the ovary to increase the production of estradiol.
Estradiol is a sex hormone responsible for the proliferation of the uterine lining. When endometrial cells proliferate, blood vessels and uterine glands develop.
When the second week starts, the concentration of FSH hormones stablizes due to the inhibitory effects of estradiol. This causes follicle recruitment to happen: just one out of all the ovarian follicles is able to interact with FSH and continue its development. The remaining follicles will degenerate, and the eggs they contained are lost.
The follicle that has been able to survive continues growing until it becomes a preovulatory follicle or Graaf follicles.
Ovulation
By the end of the second week of the menstrual cycle, another major hormonal change occurs: the LH surge.
The LH surge causes the Graaf follicle to burst and release the egg that it contained, which travels to the Fallopian tube. This is the process that we all know as ovulation.
Finally, the follicle that has just released an egg cell becomes the corpus luteum. This endocrine structure is involved in the production of estrogen and progesterone, which have a direct effect on the endometrium (uterine lining).
Symptoms to expect
Since pregnancy has not occurred yet, there is no way for you to feel pregnancy symptoms. If any, the symptoms you are likely to have are those associated with ovulation, including:
- Watery, egg white cervical mucus (EWCM)
- Increased basal body temperature (at least 0.2-0.5 °C)
- Increased sex drive
- Pain in the lower abdomen
- Bloating
- Lots of gas
- Spotting or light bleeding in the most severe cases
Broadly speaking, the discomforts and symptoms caused by ovulation are milder than those caused by the Premenstrual Syndrome or PMS.
You can read more about ovulation pain in this article: What is ovulation pain?
Ovulation predictor kits
Those women who are trying to conceive (TTC) and have trouble identifying their fertile days because they lack ovulation symptoms can use an ovulation predictor test to find them out.
Ovulation test strips can be purchased at pharmacies and work by detecting the LH surge in urine. Thanks to them, you can learn about your most fertile days easily and quickly.
Sexual intercourse during the second week of the menstrual cycle increases the chances of getting pregnant, as the woman is in her fertile days (fertile window).
For more information on this topic you can continue reading the following post: Ovulation tests - how do they work and what is their purpose?
Special recommendations and care
Those who are trying to get pregnant should start following healthy lifestyle habits in order to have a healthy pregnancy.
In women who have fallen pregnant unexpectedly, it is common that they pick up healthy habits once they learn about the pregnancy and not earlier.
To sum up, when a couple is TTC, following healthy habits is crucial. Here are some useful tips for you to follow from this moment on:
- Visit your OB/GYN: If you are trying to get pregnant, you should tell your doctor about your plans in order to make sure that everything's fine with you.
- Foods to eat: Although there are no foods to avoid, you should include those that are reach in proteins, folic acid, calcium, etc. Moreover, you can add vitamin supplements to your diet to stay healthier.
- Caffeine, tobacco and alcohol: You should quit these unhealthy habits as soon as possible if you want to have a healthy pregnancy from the very beginning. Caffeine, nicotine, and alcoholic drinks are toxic substances that may damage the baby and increase the miscarriage risk.
- Antibiotics: You can take antibiotics during this second week, especially if there in cases of urinary tract infections (UTIs). Drinking plenty of water is strongly recommended as well.
Additionally, specialists do recommend that women who are trying to become pregnant get informed about good health habits to pick up before and during pregnancy. Learning about the habits to avoid is essential, too. Magazines, reliable forums and support groups can be of great help.
FAQs from users
Will the pregnancy test be positive in the second week of gestation?
Human chorionic gonadotropin or hCG is the biomarker used to detect pregnancy, as it is produced exclusively by the trophoblast (which is what gives rise to the placenta). This hormone can be detected in both blood and urine before pregnancy can be detected by ultrasound.
HCG begins to be secreted into the maternal circulation after implantation, which normally occurs 8 to 10 days after ovulation, and its concentration doubles approximately every 48 hours during the first 30 days after implantation.
Normally, urine pregnancy tests will be able to detect hCG at 4 weeks gestation, as they will only be positive when the hCG concentration is at least 20mIUI/ml. It should be borne in mind that pregnancies are counted from the last menstrual period, so that 4 weeks of gestation will actually be 2 weeks from ovulation, which is when fertilization has occurred and the embryo has been created. In other words, the hCG concentration will be easily detected about 8-10 days after implantation.
The determination of hCG in the blood will be much more sensitive and can be positive when the urine test does not yet detect the hormone. According to studies, at 8 days after ovulation it would be possible to detect concentrations of around 10MUI/ml of hCG in the blood.
What does it feel like in the second week of pregnancy?
During the first two weeks of pregnancy you do not feel anything related to gestation since conception has not yet taken place. Remember that the weeks of pregnancy are counted from the last menstrual period and not from the moment the embryo implants in the uterus.
Therefore, during these two weeks, the woman's body prepares for the future pregnancy and the symptoms that can be noticed are those related to menstruation or subsequent ovulation, such as, for example, slight pain in the abdomen, pain in the ovary during the period, etc.
Can you see a 2 week pregnancy on ultrasound?
No, in this second week of pregnancy, conception has not yet occurred, the embryo does not exist and, therefore, it does not make sense to do a pregnancy test or an ultrasound.
Another case would be if we were talking about an ultrasound during a gynecological check-up to see the uterus or the ovaries. In this case, there is no problem in performing this diagnostic test.
How can I have an abortion in the second week of pregnancy?
The second week of pregnancy is not the same as the second week of embryonic development.
In the second week of pregnancy there is no abortion because the fetus does not yet exist. However, it is possible to take the so-called morning-after pill to prevent pregnancy if you have had unprotected sex and do not wish to have a child.
However, in the second week of life of the fetus after conception, which corresponds to the fourth week of gestation, it is possible to have an abortion using drugs such as misoprostol, under doctors supervision.
Recommended reading
In this post we have talked about the second week being when ovulation occurs. You can find out more about this and the symptoms a woman can experience in this post: When does ovulation occur?
It is during the second week when couples should start having intercourse every two days approximately in order to increase the chances for egg fertilization and embryo implantation. You cna read more about this in the following article: How Does Natural Conception Occur?
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Barros C, Crosby JA, Moreno RD (1996). Early steps of sperm-egg interactions during mammalian fertilization. Cell Biol Int; 144: 33-9
Bellido, P. (1997). Mecanismo de fertilización. Ginecol Obstet (Perú); 43(3): 183-90.
Cerqueira Dapena MJ. (2003). Metabolismo en el embarazo. Modificaciones endocrinas. Modificaciones psíquicas. En: Cabero Roura L (Director). Tratado de Ginecología, Obstetricia y Medicina de la Reproducción. Madrid: Editorial Médica Panamericana.
Chiazze L Jr Brayer F T Macisco J J Jr Parker M P Duffy B J 1968 The Length and Variability of the Human Menstrual Cycle JAMA, 203 (6) pp 377-380.
Fluhmann C F 1934 The Length of the human menstrual cycle. Department of obstetrics and gynecology American Journal of Obstetrics and Gynecology, 2 (1) pp 73-78.
González Merlo J. (1992). Modificaciones fisiológicas producidas en el organismo materno por el embarazo. En: Williams. Obstetricia (4.a ed.). Barcelona: Masón.
Haroun HSW. Reproductive cycles in females. MOJ Women’s Health. 2016;2(2):62‒64.
Heffner LD (2001). Human reproduction at a glance. New York: Blackwell Science Ltd; 45.
Hummel, T., Gollisch, R., Wildt, G., and Kobal, G. (1991). Changes in olfactory perception during the menstrual cycle. Experentia, 47, 712-715.
Vollman R F 1956 The Degree of Variability of the Length of the Menstrual Cycle in Correlation with Age of Woman Gynaecologia 142 (5): 310–314.
Wilcox AJ, Weinberg CR, Baird DB. Timing of intercourse in relation to ovulation: effects on the probability of conception, survival of the pregnancy and sex of the baby. N Engl J Med 1995;333:1517– 1521.
FAQs from users: 'Will the pregnancy test be positive in the second week of gestation?', 'Why are you considered two weeks pregnant at conception?', 'What does it feel like in the second week of pregnancy?', 'Can you see a 2 week pregnancy on ultrasound?', 'Can you get a positive pregnancy test at 2 weeks?', 'How can I have an abortion in the second week of pregnancy?' and 'How big is your baby at 2 weeks?'.
Authors and contributors

More information about Michelle Lorraine Embleton






Hi, I have cystitis and I am TTC and hoping this month is the month we will get that positive test. Is it going to affect my chances if I take the antibiotics? Thanks
Hi Marylou365
Don’t worry, there is no problem with you taking antibiotics in week 2 of pregnancy. In fact it is especially important to treat a urine infection, which could cause problems for gestation. It is also a good idea for you to drink lots of water (at least 2 litres a day).
I hope this has helped you. Kind regards
hello, i did an opk and the line is not as dark as the control line… i did several opks but the result is always the same, does it mean positive or not? i can clearly see a line, but not so dark… very curious! pls help