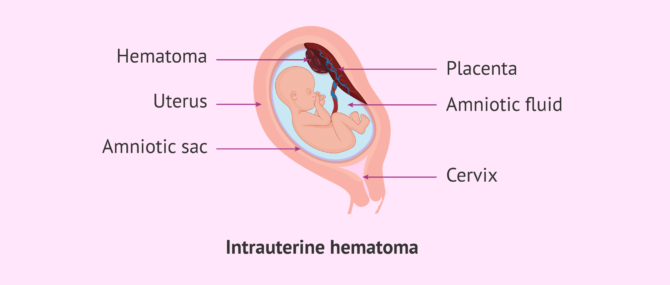
An intrauterine hematoma is an accumulation of blood within the uterine cavity during gestation.
They appear most frequently in the first trimester of pregnancy and may or may not result in vaginal bleeding.
Intrauterine hematomas are always a cause for concern in pregnant women. In addition, the pregnancy is considered high-risk and, therefore, it will be necessary for the woman to rest and monitor her condition more closely.
Provided below is an index with the 7 points we are going to expand on in this article.
- 1.
- 1.1.
- 2.
- 2.1.
- 3.
- 4.
- 4.1.
- 4.2.
- 4.3.
- 4.4.
- 4.5.
- 5.
- 6.
- 7.
What are intrauterine hematomas?
Intrauterine hematomas, also called interdeciduotrophoblastic hematomas, are blood clots that accumulate between the placenta or chorionic tissue and the inner lining of the uterus.
The appearance of these hematomas can compromise fetal development and lead to miscarriage in the worst case scenario.
However, most of the time, the clotted blood is reabsorbed and gestation proceeds normally.
Types of intrauterine hematomas
Intrauterine hematomas are classified according to their location between the different tissue layers. These are discussed below:
- Retroplacental
- are formed between the placenta and the endometrium. They are associated with placental abruption, which is usually the most common cause of bleeding after 28 weeks. Therefore, they may result in miscarriage or premature delivery.
- Subchorionic
- are normally formed inside the endometrial cavity in the first weeks of pregnancy. Although they also constitute a threat of miscarriage, these hematomas usually have a favorable evolution and do not end in gestational loss.
- Supracervical
- are the ones with the best prognosis due to their location. They are usually excreted from the vagina in the form of bleeding.
In addition to the location of the hematoma, its severity will also depend on the size of the hematoma. In general, the volume of intrauterine hematomas is measured using the formula of length by width in millimeters.
The hematoma is considered small if its size is less than 20% of the gestational sac and large if it exceeds 50%.
What are the causes of intrauterine hematomas?
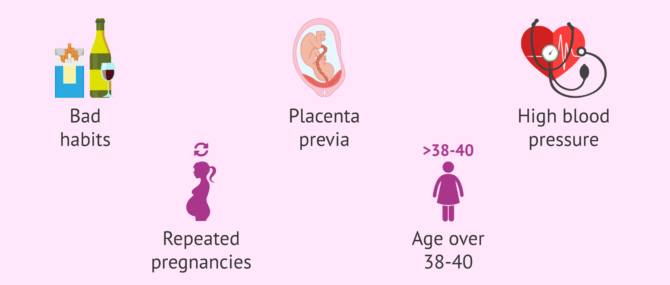
The causes of intrauterine hematomas formation are unknown. However, their occurrence has been related to the following factors:
- Bad habits such as smoking or alcohol.
- Previous abdominal injuries
- Placenta previa.
- Arterial hypertension or preeclampsia.
- Having had several pregnancies.
- Pregnancy in women over 38-40 years old.
Most probably, the origin of intrauterine hematomas is located around embryo implantation, due to the injury caused to the endometrium, which eventually turns into clotted blood.
If these blood clots are not broken up or reabsorbed, the hematomas can continue to grow and put pressure on the embryo, which could lead to miscarriage in the worst case scenario.
How are they diagnosed?
Intrauterine hematomas do not usually have associated symptoms such as pain, but sometimes it is possible for the woman to have blood loss.
Vaginal bleeding caused by intrauterine hematomas can vary in color and amount. In any case, whenever there is bleeding in pregnancy, it is advisable to see a doctor as soon as possible.
Intrauterine hematomas will be diagnosed by ultrasound, where measurements will be taken to follow their evolution.
In the absence of blood loss, hematomas will be detected during routine ultrasound scans.
Treatment and prognosis
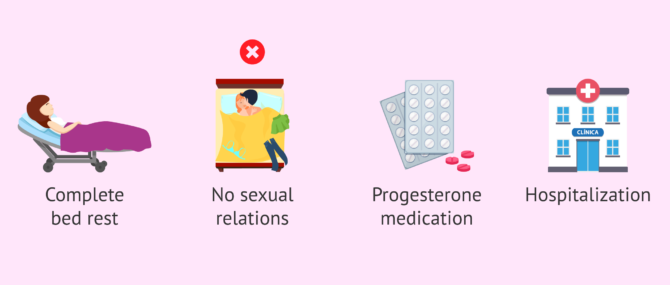
First of all, when faced with an intrauterine hematoma, it is necessary to follow all the doctor's recommendations and go to the doctor's office as often as indicated by the doctor for monitoring. Normally, the pregnant woman should visit the doctor once every one or two weeks until the risk has passed.
The prognosis of intrauterine hematomas is mainly assessed taking into account two elements: their location and size.
Small hematomas usually have a favorable evolution and are spontaneously reabsorbed. The time it will take for intrauterine hematomas to be eliminated depending on the size and location.
If the hematomas grow and reach a large size, the pregnancy will be considered high risk and some preventive measures will have to be taken. Some of them are listed below:
- Absolute rest.
- Do not have sexual relations.
- Progesterone pessaries in some cases.
- Emergency hospitalization in the most severe cases.
Usually, as gestation progresses, the circulation of hematomas normalizes and most of them gradually disappear. As we have said, bleeds during pregnancy are very alarming for women. Especially in cases of large intrauterine hematomas, where bleeding will be abundant and dramatic. However, this symptom does not indicate a worse prognosis, as it means that the hematoma is being progressively eliminated and reduced in size.
FAQs from users
What are the intrauterine hematomas with the worst prognosis?
Large hematomas located in the wrong place. For example, large central retroplacental hematomas, in which there is separation between the chorionic tissue and the basal decidua (layers that surround the placenta). This can lead to placental abruption or premature rupture of the placenta, resulting in miscarriage or preterm birth, if the pregnancy is in an advanced stage.
What are the risks of hematoma in a twin pregnancy?
As with a singleton pregnancy, the severity of the hematoma depends on its size and location in the uterus. However, as there is less intrauterine space in a multiple pregnancy, the situation could become more complicated. In short, twin pregnancies with intrauterine hematomas will require greater control and absolute rest on the part of the mother.
In the gynecological consultation, the growth of both fetuses will be monitored and a cesarean section will be scheduled in case of fetal distress.
What precautions should you take if you have a hematoma in pregnancy?
Depending on the size and severity of the hematoma, the doctor may indicate partial or complete rest. In general, no exercise or sexual intercourse is recommended.
It is also possible that the doctor may prescribe a special diet and/or the administration of progesterone pessaries.
¿Los hematomas intrauterinos siempre aparecen en el primer trimestre de embarazo?
Most frequently, yes, but intrauterine hematomas can also appear later in pregnancy. In this case, when intrauterine hematomas appear in more advanced stages, good control is important since they could cause gestational complications.
¿Un hematoma intrauterino es amenaza de aborto?
To some extent intrauterine hematomas pose a threat of miscarriage. However, most hematomas that appear inside the uterus are usually not dangerous since they usually reabsorb on their own.
Recommended reading
Blood loss during pregnancy may have a different cause than the one discussed in this article. You can find out more about the possible causes of bleeding during pregnancy here: Is bleeding in pregnancy normal? What are the causes?
If you want to continue reading about the cause and advice for high risk pregnancies, we recommend the following post: High Risk Pregnancy - How Can You Manage it?
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
C I Akman, J Cracco. Intrauterine subdural hemorrhage. Dev Med Child Neurol. 2000 Dec;42(12):843-6. doi: 10.1017/s0012162200001559.
C L Tower, L Regan. Intrauterine haematomas in a recurrent miscarriage population. Hum Reprod. 2001 Sep;16(9):2005-7. doi: 10.1093/humrep/16.9.2005 (View)
M Al-Memar, T Vaulet, H Fourie, S Bobdiwala, J Farren, S Saso, T Bracewell-Milnes, B De Moor, S Sur, C Stalder, P Bennett, D Timmerman, T Bourne. First-trimester intrauterine hematoma and pregnancy complications. Ultrasound Obstet Gynecol
. 2020 Apr;55(4):536-545. doi: 10.1002/uog.20861 (View)
Marc Van de Velde, Christian Diez, Albert J Varon. Obstetric hemorrhage. Curr Opin Anaesthesiol. 2015 Apr;28(2):186-90. doi: 10.1097/ACO.0000000000000168.
Thaisa A R M Narciso, Mara S Hoshida, Priscilla R Costa, Andrea Niquirilo, Sckarlet E Biancolin, Lawrence H Lin, Rossana P V Francisco, Maria L Brizot. Fetal-Maternal Hemorrhage in First-Trimester Intrauterine Hematoma. Fetal Diagn Ther (Ver). 2021;48(3):227-234. doi: 10.1159/000513747. Epub 2021 Mar 11
FAQs from users: 'What are the intrauterine hematomas with the worst prognosis?', 'What are the risks of hematoma in a twin pregnancy?', 'What precautions should you take if you have a hematoma in pregnancy?', '¿Los hematomas intrauterinos siempre aparecen en el primer trimestre de embarazo?' and '¿Un hematoma intrauterino es amenaza de aborto?'.
Authors and contributors

More information about Michelle Lorraine Embleton




Hi
I am 6 weeks pregnant and I am having some spotting and I am really worried. Could one of these hematomas be the cause of the bleeding? What can I do about it?
Any help much appreciated.
Hi Deborah DD
The best thing you can do is consult your specialist as soon as possible. There can be different causes for bleeding in early pregnancy. An intauterine hematoma is one of the possible causes but you should see your doctor so they can perform the necessary tests.
At six weeks pregnant they may decide to do a vaginal ultrasound to see if the baby’s heartbeat can be detected, and blood tests to check the levels of pregnancy hormones could be ordered.
Most importantly, try not to panic and take it easy. I know this is easier said than done but the less stress the better.
I wish you the best and hope this answer has helped.