The endometrium is the inner lining of the uterus. It is a layer that varies throughout the menstrual cycle, with the purpose of allowing the embryo to implant in it in order to give rise to a gestation.
Taking into account this premise, in assisted reproduction treatments (ART) it is of vital importance to control that the endometrium has the appropriate characteristics to favour the implantation of the embryo. For this reason, there are several tests that can be performed to assess the patient's endometrium prior to embryo transfer.
In this way, we try to guarantee that the endometrium is in the best conditions to receive the embryo.
Provided below is an index with the 6 points we are going to expand on in this article.
- 1.
- 2.
- 2.1.
- 2.2.
- 2.3.
- 3.
- 3.1.
- 3.2.
- 3.3.
- 4.
- 5.
- 6.
How does the endometrium change?
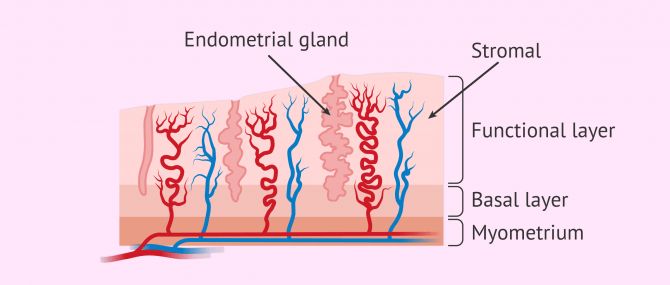
The endometrium is composed of a basal layer and a functional layer. The basal layer is responsible for producing a new functional layer each cycle, as this functional layer is regenerated each month in the event that no gestation has occurred.
To do this, the endometrium undergoes changes throughout the menstrual cycle. These variations are guided by estrogens and progestogens produced by the ovary. In this way, the endometrium goes through different phases:
- Proliferative phase: the stromal cells and endometrial glands increase due to oestrogenic influence. This phase takes place until ovulation, i.e. day 14 of the menstrual cycle.
- Secretory phase: glandular secretion of substances necessary for embryo implantation. This change occurs in response to progesterone released by the ovarian corpus luteum after ovulation.
If pregnancy has not occurred, the degeneration of the corpus luteum leads to the shedding of the endometrium, which will be expelled with menstruation.
You can learn more about changes in the endometrium at this link: What's the Role of the Endometrium? - Function & Thickness.
Tests for endometrial assessment
The embryo should implant in the endometrium approximately 6 days after fertilization. Not only the quality of the embryo is important, but also the condition of the endometrium plays an equally decisive role. In addition, embryo and endometrium must be synchronized.
For this reason, there are several tests that can be performed to assess the patient's endometrium prior to embryo transfer.
Ultrasound monitoring of the endometrium
As a non-invasive technique, vaginal ultrasound allows us to study the endometrium throughout the menstrual cycle. In assisted reproduction, endometrial thickness and endometrial pattern are evaluated in a standard way to assess and estimate its receptivity.
The ideal for embryo transfer is that the endometrium has an adequate thickness. It seems that an ideal endometrium is one that is 7-9 mm thick and with a trilaminar pattern. A thin endometrium seems to be associated with lower pregnancy rates.
In egg donation programs or frozen embryo transfers, vaginal ultrasound plays a fundamental role in confirming that the endometrium is ready to receive the embryo. In these cases, the endometrium must be prepared in advance by administering hormones (estrogens and progesterone), or by taking advantage of the natural cycle if the woman still has regular menses.
Assisted procreation, as any other medical treatment, requires that you rely on the professionalism of the doctors and staff of the clinic you choose. Obviously, each clinic is different. Get now your Fertility Report, which will select several clinics for you out of the pool of clinics that meet our strict quality criteria. Moreover, it will offer you a comparison between the fees and conditions each clinic offers in order for you to make a well informed choice.
Endometrial receptivity test
In assisted reproduction cycles, a great effort is made to obtain optimal embryo development. Subsequently, a selection is made among the available embryos to transfer the one that will have the best chances of success. However, this would be useless if the embryo is transferred into an endometrium that is not exactly at the right time to receive it.
This time is known as the window of implantation and, in women with regular cycles, usually corresponds to days 19-21 of the menstrual cycle. However, this window of implantation may be displaced in time in some women, which may result in failure to achieve pregnancy after several attempts with good quality blastocyst transfer.
However, there are tests available for the analysis of endometrial receptivity. These tests are performed on the basis of an endometrial biopsy and indicate whether the endometrium is receptive or not. If the endometrium is receptive, the embryo transfer will be performed under the same conditions as the biopsy. In the event that the endometrium is not receptive, the results would indicate when the embryo transfer should be performed.
Endometrial receptivity tests allow a more personalized embryo transfer, increasing the success rates of ART.
If you are interested in this type of endometrial receptivity test, we recommend you read this article: Endometrial Receptivity Array (ERA): Procedure and Success Rates.
Study of the endometrial microbiome
This type of test analyses the endometrial flora or microbiome, that is, the microorganisms found in the endometrium. In this way, from an endometrial biopsy, the test provides a result about whether the microbiome of the endometrium is suitable for the implantation of an embryo. This is because an imbalance in the endometrial flora could hinder embryo implantation.
If the endometrial flora is not dominated by Lactobacillus, it will not be the most favourable to host the embryo. In this case, the test report will recommend a personalized treatment with probiotics or antibiotics, depending on the result.
On the other hand, there is also a test that detects the main bacteria that cause chronic endometritis (inflammation of the endometrium). This test is also very important to improve the results of ART, especially when there is recurrent implantation failure, since chronic endometritis is present in a high percentage of these patients.
FAQs from users
Can endometrial thickness be improved naturally?
Endometrial thickness grows naturally in women with regular cycles in the middle of the cycle. Medications and supplements with anti-inflammatory effects should be avoided in order to avoid interfering with normal endometrial growth.
Plenty of hydration and daily physical exercise, together with a varied diet and a healthy lifestyle, will promote natural endometrial growth. In patients without menstrual periods (menopause) or patients with very irregular menstrual cycles, it will be necessary to administer drugs to help the endometrium grow.
What is the cost of the endometrial receptivity test?
The cost of the endometrial receptivity test is usually around 350-600 euros, although it is true that there may be differences between fertility clinics.
For this reason, it is essential to request a personalised quote during the first visit to a fertility centre, including the cost of complementary techniques and additional tests.
What endometrial thickness is needed for IVF?
Ideally for an embryo transfer after an IVF cycle, the endometrium should be about 8 mm thick and have a trilamellar appearance on ultrasound.
However, an endometrial thickness of 8 mm does not guarantee that the embryo will implant. Similarly, gestation is also possible with thinner endometria, although these endometria result in lower pregnancy rates.
Suggested for you
If you want to learn more about how the endometrium is prepared in assisted reproductive techniques (ART), you can read the following article: Endometrial Preparation for Implantation After IVF Embryo Transfer.
If, on the other hand, you are interested in learning more about the embryo transfer process, we recommend you to visit this link: IVF Embryo Transfer Procedure - Definition, Process & Tips.
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Bu Z, Sun Y. The Impact of Endometrial Thickness on the Day of Human Chorionic Gonadotrophin (hCG) Administration on Ongoing Pregnancy Rate in Patients with Different Ovarian Response. PLoS One. 2015 Dec 30;10(12):e0145703.
Enciso M, Carrascosa JP, Sarasa J, Martínez-Ortiz PA, Munné S, Horcajadas JA, Aizpurua J. Development of a new comprehensive and reliable endometrial receptivity map (ER Map/ER Grade) based on RT-qPCR gene expression analysis. Hum Reprod. 2018 Feb 1;33(2):220-228.
Moreno I, Codoñer FM, Vilella F, Valbuena D, Martinez-Blanch JF, Jimenez-Almazán J, Alonso R, Alamá P, Remohí J, Pellicer A, Ramon D, Simon C. Evidence that the endometrial microbiota has an effect on implantation success or failure. Am J Obstet Gynecol. 2016 Dec;215(6):684-703.
Moreno I, Simon C. Relevance of assessing the uterine microbiota in infertility. Fertil Steril. 2018 Aug;110(3):337-343.
Simón C, Gómez C, Cabanillas S, Vladimirov I, Castillón G, Giles J, Boynukalin K, Findikli N, Bahçeci M, Ortega I, Vidal C, Funabiki M, Izquierdo A, López L, Portela S, Frantz N, Kulmann M, Taguchi S, Labarta E, Colucci F, Mackens S, Santamaría X, Muñoz E, Barrera S, García-Velasco JA, Fernández M, Ferrando M, Ruiz M, Mol BW, Valbuena D; ERA-RCT Study Consortium Group. A 5-year multicentre randomized controlled trial comparing personalized, frozen and fresh blastocyst transfer in IVF. Reprod Biomed Online. 2020 Sep;41(3):402-415.
FAQs from users: 'Can endometrial thickness be improved naturally?', 'What is the cost of the endometrial receptivity test?' and 'What endometrial thickness is needed for IVF?'.
Authors and contributors