Genetic infertility is infertility caused by some alteration in the DNA sequence of the man or woman who is trying to have a child.
Depending on the type of genetic anomaly, it is possible to differentiate between:
- Aneuploidies
- numerical or structural alterations of the chromosomes.
- Genetic mutations
- defects in one or more genes.
Sometimes, prospective parents are not aware that they are carriers of a genetic disorder until they begin to have difficulties in achieving pregnancy.
Provided below is an index with the 8 points we are going to expand on in this article.
- 1.
- 1.1.
- 2.
- 3.
- 4.
- 4.1.
- 4.2.
- 4.3.
- 4.4.
- 5.
- 5.1.
- 5.2.
- 5.3.
- 6.
- 7.
- 8.
Genetic male infertility
Although apparently, they do not show other symptoms that affect their health, men affected by or carrying a genetic pathology may suffer sterility.
In the following list, we will describe the most common causes of this genetic sterility in the male:
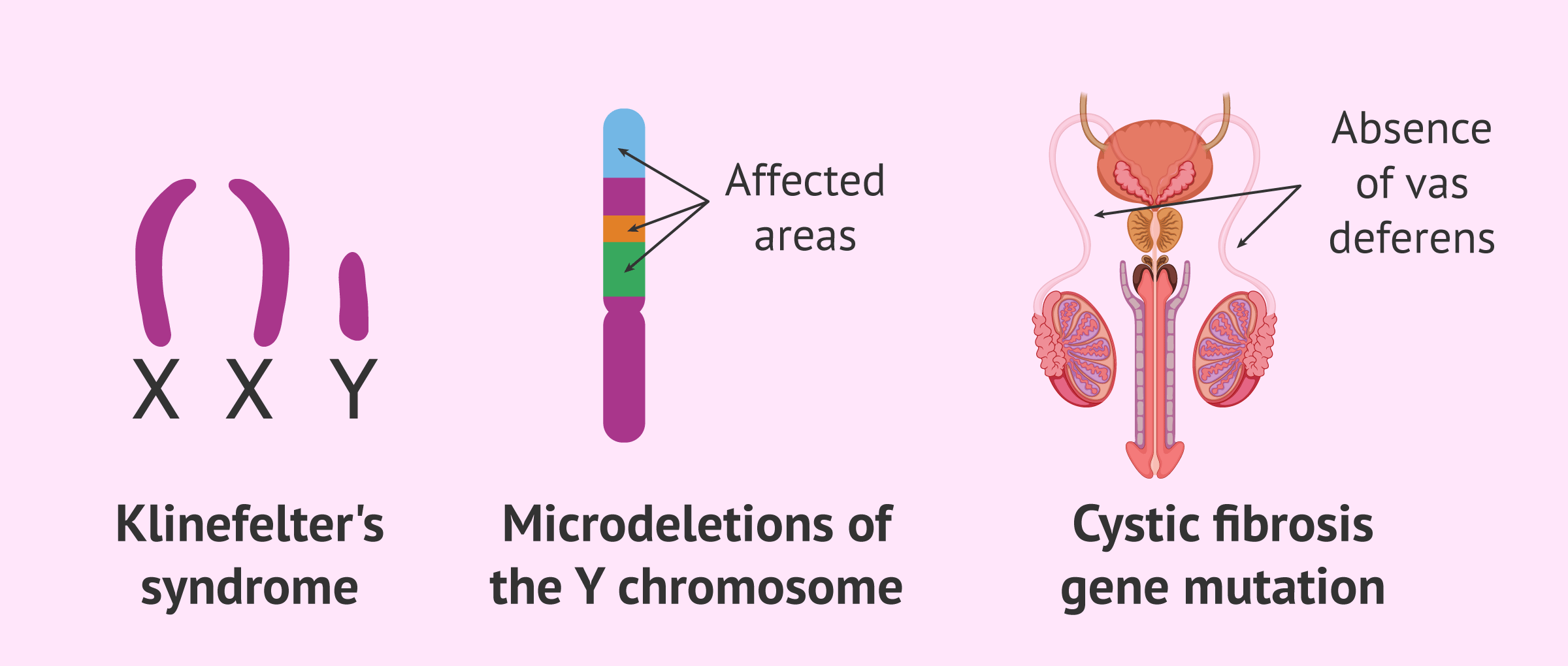
- Klinefelter's syndrome
- these males have an extra X chromosome (47,XXY). As a consequence, spermatogenesis is defective and they do not produce spermatozoa, being the most important genetic cause of secretory azoospermia.
- Y chromosome microdeletions
- this is a small loss of genetic material on the Y chromosome. The consequence of this is also a secretory azoospermia in the male.
- Mutations in the cystic fibrosis gene (CFTR)
- these defects give rise to the well-known congenital bilateral absence of the vas deferens. As a consequence, sperm cannot exit through the urethra with ejaculation and is the main genetic cause of obstructive azoospermia.
Thanks to assisted reproduction, these men have been able to have children by obtaining sperm from the testicle with a biopsy and performing in vitro fertilization (IVF). However, it should be noted that there is a risk of transmitting this genetic infertility to offspring.
Genetic alterations in spermatozoa
It is also possible that the man has no alteration in his genetic material, but his spermatozoa do. This would result in fertilization failure, implantation failure, or recurrent miscarriages.
The origin of these genetic faults lies in the process of sperm formation and maturation that occurs in the testes. It is possible that it may occur:
- Sperm DNA fragmentation
- Diploid spermatozoa (with two chromosomes instead of one)
- Nullisomic spermatozoa (no genetic material)
- Spermatozoa with structural abnormalities in chromosomes
Unfortunately, in the present, there are no techniques to separate genetically healthy spermatozoa from those with abnormalities in their DNA. Therefore, the only option for these couples is to resort to preimplantation genetic diagnosis (PGD) or donor sperm.
Genetic female infertility
In the case of females, the most relevant chromosomal disease-causing sterility is Turner syndrome. This disorder is due to the presence of a single-sex chromosome (45,X0).
Women with Turner syndrome have defined characteristics such as short stature or short neck, in addition to other fertility-related alterations, such as lack of sexual development, ovarian failure, absence of menstruation, etc.
However, there are females who present Turner syndrome in mosaicism. This means that some cells in your body are normal, while others are missing an X chromosome.
Women with mosaic Turner syndrome often find out about this condition when they have trouble conceiving and have genetic testing.
Other disorders that can cause female sterility of genetic origin are hereditary thrombophilias, such as mutation of the MTHFR gene. Defects in blood clotting can lead to repeated miscarriages.
Finally, as in the case of sperm, eggs can also carry numerical or structural chromosomal abnormalities caused in the process of meiosis.
Genetic alterations in the embryo
There is a possibility that, although the couple's eggs and sperm are healthy and free of genetic alterations, the embryos resulting from fertilization may not be viable.
During fertilization, the female nucleus of the egg must fuse with the male nucleus of the sperm, and the new chromosomal endowment of the embryo is established. Any error in this process will result in aneuploid embryos that cannot implant or if they do, will result in miscarriage or the birth of a sick baby.
The main cause of these genetic alterations in embryos is poor oocyte quality due to advanced maternal age.
How is genetic infertility diagnosed?
In most cases, genetic infertility is not diagnosed until more specific fertility tests are done. A simple seminogram, ultrasound or hormone analysis cannot detect genetic alterations.
Below, we will discuss the most common tests for genetic diagnosis of infertility.
Karyotype analysis
The karyotype refers to the set of chromosomes found within each cell. In the human species, the karyotype consists of 22 pairs of autosomal chromosomes and one pair of sex chromosomes that define the sex of the individual:
- Man
- 46,XY.
- Woman
- 46,XX.
Therefore, karyotype analysis is used to study whether a person has the chromosomal load that corresponds to him or, on the other hand, presents some type of translocation, trisomy, monosomy, etc.
The karyotype is performed on both members of the couple and has an approximate cost of about 100-2000$. More and more fertility clinics are indicating the performance of a karyotype at the first visit to make a more personalized diagnosis.
FISH of spermatozoa
Fluorescent in situ hybridization or FISH is another technique used to analyze possible abnormalities in the number or structure of chromosomes.
As it can be performed on spermatozoa, this diagnostic test provides more information about the male's reproductive capacity.
The chromosomes analyzed are those most likely to be altered: 13, 18, 21, X, and Y, although in cases of recurrent miscarriages chromosomes 16 and 22 are also analyzed.
However, after analysis, these spermatozoa cannot be used in any assisted reproduction technique to achieve pregnancy, so it is not possible to select or separate viable spermatozoa from those with chromosomal alterations.
You will find all the information about this genetic test in the following post: FISH in spermatozoa.
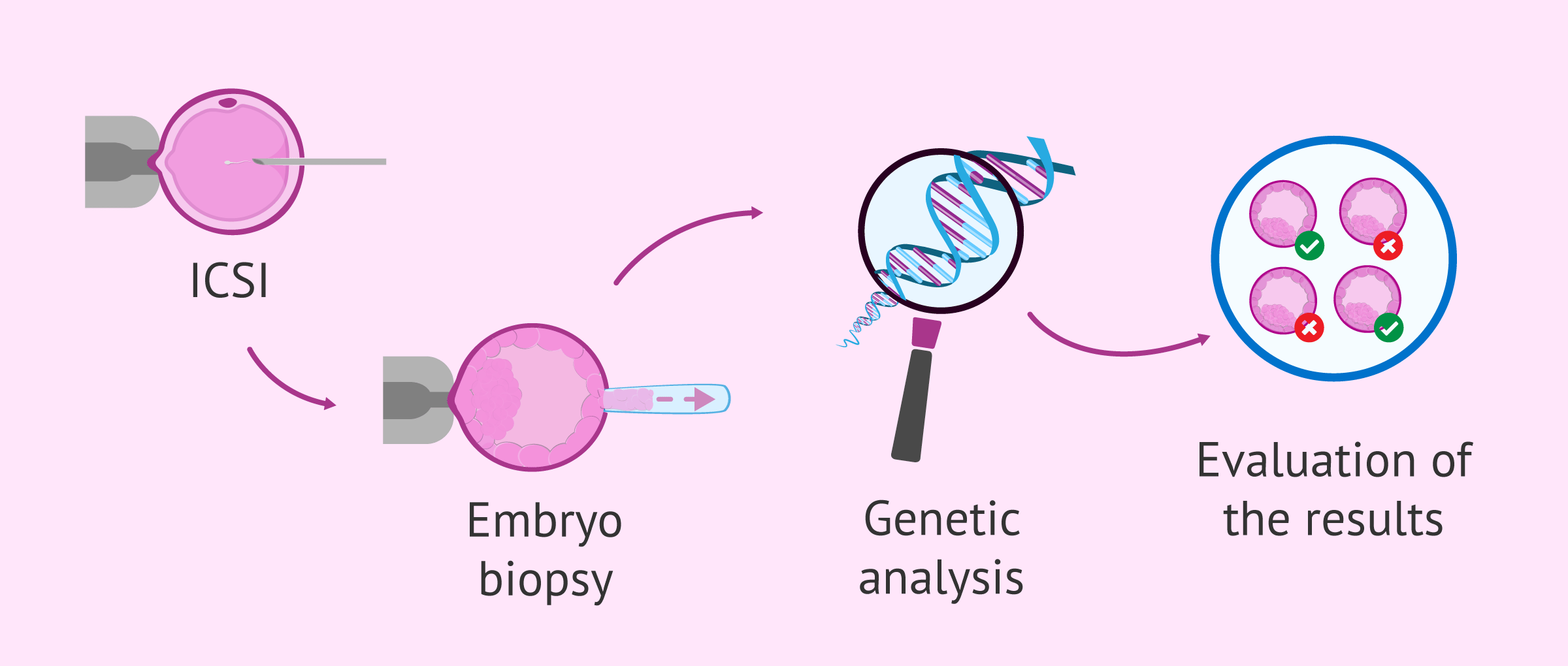
Preimplantation genetic diagnosis
Preimplantation genetic diagnosis or PGD is a genetic analysis performed on the embryos resulting from the fertilization of the couple's eggs and sperm. Therefore, PGD is the only technique that ensures the pregnancy of a healthy baby, free of any genetic alteration coming from the parents.
To perform PGD, it is necessary for the couple to undergo in vitro fertilization (IVF) treatment and thus obtain the embryos in the laboratory. An embryo biopsy is then performed to collect one or more cells from each embryo, which will be analyzed.
Once the PGD results are obtained, genetically viable embryosare selected. This means that embryos that are genetically healthy will be transferred and embryos that have any aneuploidy or genetic mutation will be discarded.
If you want more information about this complimentary technique, you can read the following article: What is the preimplantation genetic diagnosis?
Prenatal tests
If there is a risk of having children with genetic pathologies and a PGD has not been performed to ensure a viable pregnancy, there are prenatal genetic tests that can be performed on the fetus during the course of gestation.
If the result of these prenatal tests is not favorable, the woman or couple will have to choose whether to terminate the pregnancy in order to avoid the birth of a sick baby.
The different types of prenatal genetic testing are as follows:
- Fetal DNA blood test
- this is a non-invasive prenatal test, since it analyzes the DNA of the fetus found in the maternal blood.
- Chorionic biopsy
- through an abdominal or vaginal puncture, a sample of the chorionic villi of the placenta is obtained to perform the genetic study.
- Amniocentesis
- amniotic fluid is obtained through an abdominal puncture and the fetal cells suspended in it are analyzed.
We recommend you to read the following article if you are interested in knowing more information about this topic: Types of prenatal diagnostic tests.
FAQs from users
Is it advisable to perform PGD whenever there is a risk of aneuploidy?
Yes, it is the only technique that allows embryos with normal chromosomal endowment to be transferred to the uterus, without chromosomal aneuploidy.
What is genetic counseling?
Genetic counseling or genetic counseling is a service to provide all the information and support to couples who suffer from or are at risk of transmitting a genetic disorder.
In the consultation, the geneticist analyzes all the family history of the patients and the genetic studies performed in order to be able to inform about the genetic risks that exist, as well as to recommend the most appropriate treatment in each case.
When is it necessary to perform a karyotype?
The karyotype is indicated in all couples who attend an assisted reproduction consultation due to infertility problems. However, there are clinics that only send it in the following cases:
- Azoospermia
- Severe oligozoospermia
- Repeated implantation failures
- Repeat abortions

Recommended readings
In addition to everything discussed throughout this article, there are also hereditary genetic diseases that, although they do not cause sterility, prospective parents do not want to pass on to their children. Therefore, PGD will also be necessary to avoid these pathologies: What genetic or chromosomal diseases can PGD detect?
On the other hand, you can learn more about the tests that are performed during pregnancy in order to ensure the health of both the baby and the mother-to-be in the following article: Prenatal pregnancy control.
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Control prenatal del embarazo normal. PROTOCOLOS SEGO. Progresos de Obstetricia y Ginecología 2011;54(6): 330-349
Delhanty, J.D.A. and Handyside, A.H. (1995) The origin of genetic defects in the human and their detection in the preimplantation embryo. Hum. Reprod. Update, 1, 201–215.
Flannigan R, Schlegel PN. Genetic diagnostics of male infertility in clinical practice. Best Pract Res Clin Obstet Gynaecol. 2017 Oct;44:26-37.
Griffin DK, Finch KA (2005). The genetic and cytogenetic basis of male infertility. Human Fertil;8(1);19-26
Hendriks S, Peeraer K, Bos H, Repping S, Dancet EAF. The importance of genetic parenthood for infertile men and women. Hum Reprod. 2017 Oct 1;32(10):2076-2087.
O'Flynn O'Brien KL, Varghese AC, Agarwal A. The genetic causes of male factor infertility: a review. Fertil Steril. 2010 Jan;93(1):1-12.
Rodrigo, L.; Rubio, C.; Mateu, E. y Buendía, P., 2014. Capítulo 14: El laboratorio de diagnóstico genético preimplantacional. Instituto Universitario IVI Valencia. Máster en Biotecnología de la Reproducción Humana Asistida. 9ª Edición (2014-2016). 1213-1277
FAQs from users: 'Is it advisable to perform PGD whenever there is a risk of aneuploidy?', 'What is genetic counseling?' and 'When is it necessary to perform a karyotype?'.
Authors and contributors

More information about Cristina Algarra Goosman







But amniocentesis is dangerous, isn’t it? A relative of mine had it done and the baby’s sac got infected and died.
Hi Colleen,
Amniocentesis, like all invasive diagnostic techniques, has its risks. In particular, the risk of intrauterine death by amniocentesis is about 1%, so it is considered a safe technique.
I recommend that you read this article which explains what the technique consists of and how it is performed: Amniocentesis.
I hope I have helped you,
Best regards.
Hello, I have had several miscarriages and my gynecologist told me that maybe the reason can be found with this test, is this true?
Hello laialaia,
After several miscarriages, the main objective is to identify if there is a genetic problem that prevents the embryo from developing properly and consequently suffer a miscarriage.
The most commonly used test for these cases is the karyotype, in which you can see if there are any genetic abnormalities in both the father and the mother.
Once the results are established, the doctor will inform the next step or treatment to be performed.
I hope I have helped you.
Best regards.