Cancer is a fairly common disease in today's population that is associated with the loss of self-regulation of cells to divide in a controlled manner.
This disease can appear in different stages of life: in childhood, in fertile age or during the senescence of life.
Current advances in science have lead to the survival of numerous cancer patients today. This phenomenon has caused the mentality of doctors to change and to think about both the treatment to cure the patient and the preservation of fertility for the future.
Provided below is an index with the 9 points we are going to expand on in this article.
- 1.
- 2.
- 3.
- 4.
- 5.
- 6.
- 6.1.
- 6.2.
- 6.3.
- 7.
- 8.
- 9.
Fertility preservation for cancer patients
The appearance of cancer at an early age can cause significant damage to the reproductive organs. Therefore, society is trying to raise awareness about the preservation of fertility in ontological patients.
Women who have been treated with chemotherapy and radiation therapy may have failures in ovarian function, increasing the possibility of temporary or permanent infertility. The damage caused depends on the type of treatment and the severity of the injury.
Thanks to a series of techniques developed in the field of reproductive medicine, women of reproductive age who undergo cancer treatments have the option of preserving their fertility before undergoing therapies that could reduce their fertility after treatment.
Options include cryopreservation of embryos, vitrification of eggs and freezing of ovarian tissue. When considering a fertility preservation treatment, the following factors should be evaluated:
- The patient's age
- The time until the start of chemotherapy
- The hormonal treatment that the patient can receive to stimulate her ovaries does not worsen her oncological situation
If you are considering preserving your fertility to have a baby in the future, we recommend that you start by getting a Fertility Report. In 3 simple steps, it will show you a list of clinics that fit your preferences and meet our strict quality criteria. Moreover, you will receive a report via email with useful tips to visit a fertility clinic for the first time.
Therefore, the preservation of ovarian cortex will be the first option in cases of:
- Girls who have not entered puberty yet
- Patients with cancer that may be made worse by hormonal administration and where such treatment is contraindicated
- Patients who do not have time to start ovarian stimulation treatment before chemotherapy treatment
What is an ovarian tissue transplant?
Cryopreservation of ovarian tissue is an alternative for those patients who cannot receive ovarian stimulation to vitrify mature eggs. Ovarian tissue transplantation is a technique that consists of the extraction and freezing of a part of the ovary in order to later re-implant it in the patient.
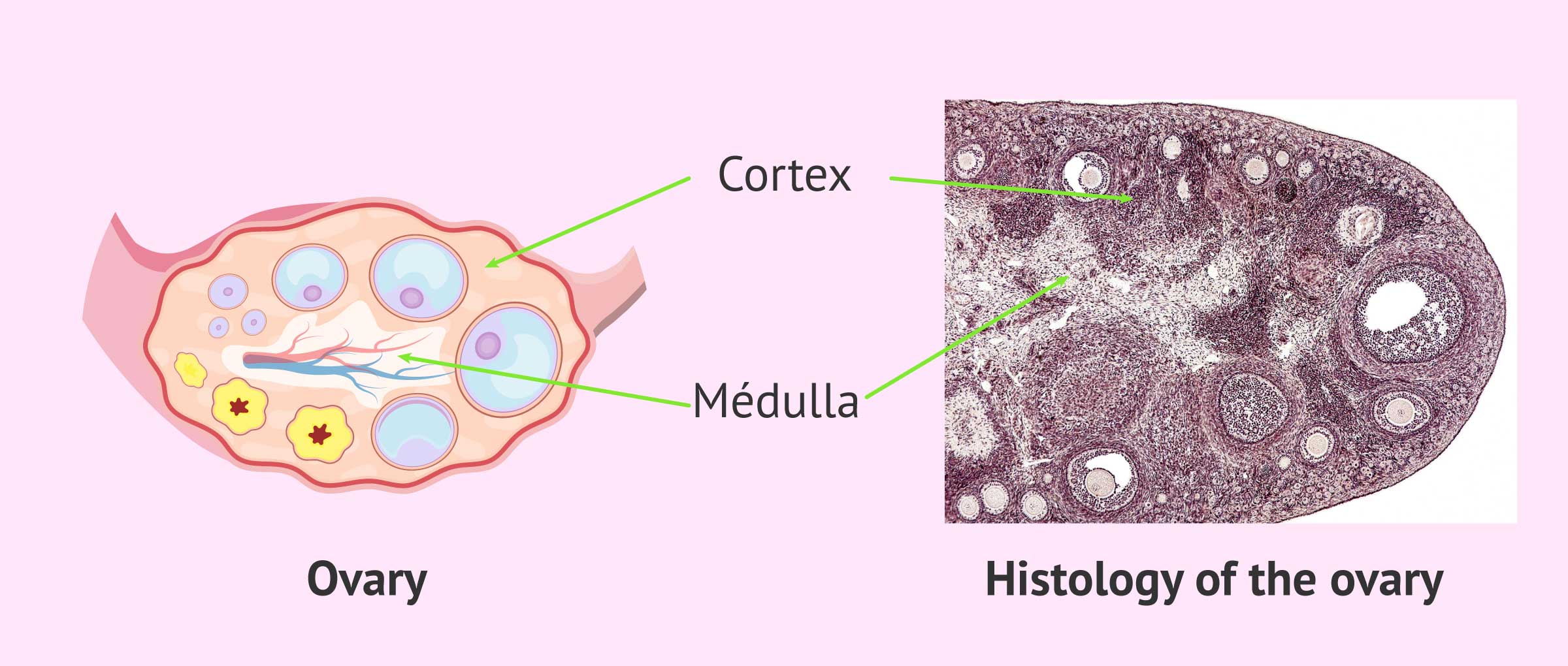
The ovary is composed of two structures, the cortex and the medulla:
- The cortex is the outermost part of the ovary and its function is to house the growing follicles that contain the woman's eggs. During pregnancy, women already have a finite number of primordial follicles in their ovarian cortex. These follicles are the future eggs that will mature monthly in the woman's reproductive years. Primary follicles are susceptible to deterioration in the presence of toxic agents, such as those used in chemotherapy and radiotherapy.
- The marrow is the central tissue that forms the nucleus of the ovary. This structure has blood vessels and arteries that provide blood and nutrients to the ovarian cortex so that it can carry out its function.
This ovarian tissue preservation technique is based on the fact that the primordial follicles, which a girl has from birth, are found in the cortex. The biopsy of this cortex and its cryopreservation can be an insurance to restore the patient's fertility in the future when the cancer treatment has been overcome.
Once the cancer disease has been overcome, the patient's fertility can be restored. By suturing the ovarian tissue as if it were a skin graft, the ability to produce ovarian hormones is restored. In this way the woman will be able to have children naturally or with the help of assisted reproduction.
Cryopreservation process of ovarian cortex
At the time a pre-pubertal girl is diagnosed with cancer, or hormonal ovarian stimulation is not indicated, the patient may have the ovarian cortex removed for freezing.
This surgery can be performed at the same time that the patient undergoes removal of the areas affected by the cancer, if any. In the event that there is no need to subject the patient to an intervention, the extraction of the ovarian tissue could be carried out by means of minimally invasive surgery.
Ovarian tissue can be cryopreserved in different ways, but the most successful and successful method is by freezing strips of the ovarian cortex.
After the ovarian cortex is removed, it is divided into small strips. Performing this technique allows substances that protect the ovarian tissue against damage from freezing, called cryoprotectants, to penetrate more effectively and achieve better results.
The primary follicles found in the ovarian cortex appear to be better preserved in the tissue than mature eggs. Perhaps the success of its survival lies in its smaller size and the absence of cellular structures that are acquired with the maturation of the egg and that are sensitive to low temperatures.
Use of ovarian tissue after cancer treatment
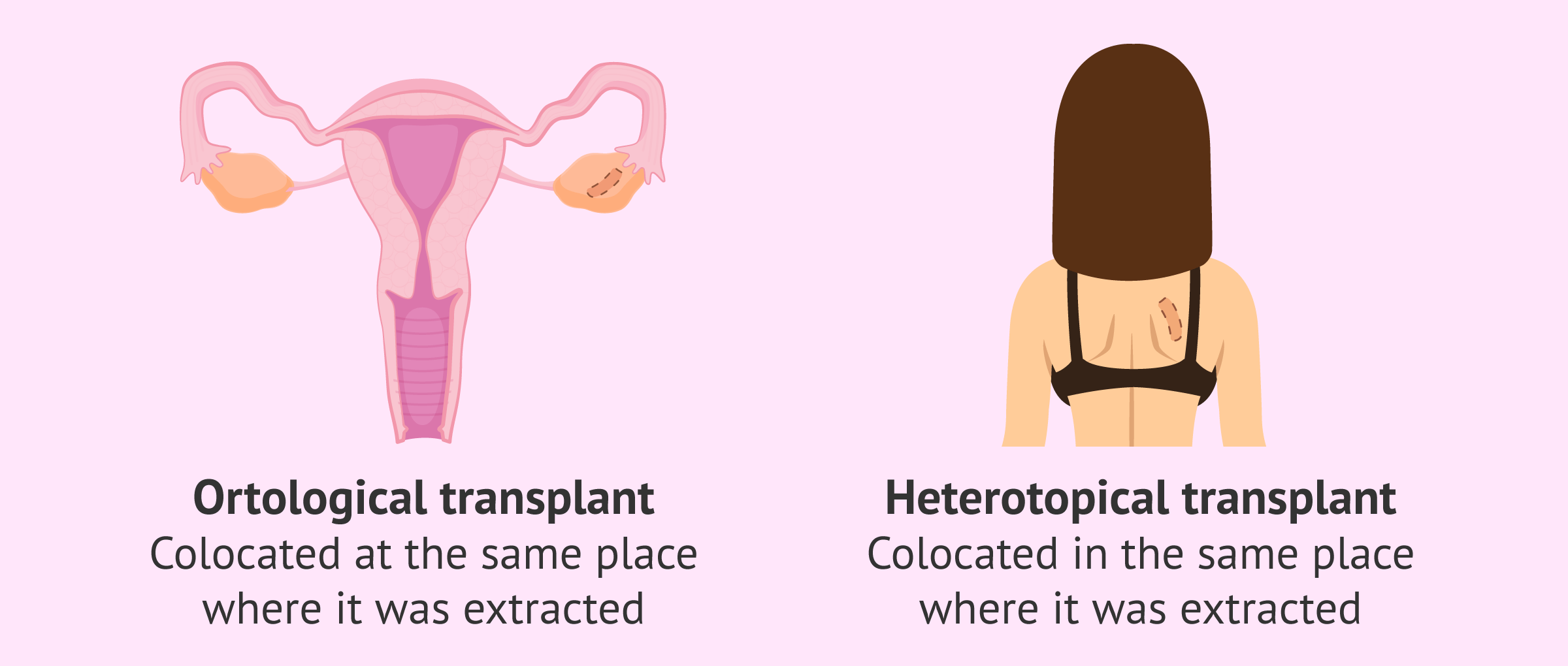
After the thawing of the ovarian tissue, it can be transplanted back to the patient. Despite the fact that this technique is recent and still in the study and experimentation phases, the transplant of ovarian tissue presents good results. Depending on the location where the graft is transplanted again, we can differentiate in
- Orthopic transplant
- when the graft is placed in the same place where it was removed, the ovary. This type of transplants, if carried out successfully, allows the ovary to become functional again and respond to the patient's hormonal cycle. Therefore, by means of this technique it is possible to achieve a natural pregnancy again.
- Heterotopic transplant
- when the graft site is different from the ovary. This new location may be in subcutaneous areas of the forearm, abdomen, or back. To this day, the ideal location for the transplant is still being discussed. Patients undergoing this type of transplant will need to undergo a cycle of assisted reproduction to stimulate and aspirate the eggs. These eggs will be treated and fertilized in an assisted reproduction laboratory by means of in vitro fertilisation (IVF).
Heterologous ovarian cortex transplants are also currently in the research and development phase. These transplants are based on the removal of the ovarian cortex of a donor woman and implantation in a recipient patient. Therefore, the removed tissue is implanted in a different person, resulting in a tissue donation.
The key to a successful transplant is revascularization of the graft once it is placed in the woman. This means that new blood vessels are created in the graft. The primary follicles that it contains are very sensitive and must receive the necessary supply of nutrients and blood supply as soon as possible. Good vascularization in the transplanted area will be vital to the success of ovarian tissue transplant surgery.
Risks and limitations of the technique
Although it is a technique that is yielding results, it should still be recommended as an experimental technique, as there are still many questions that researchers have not managed to answer:
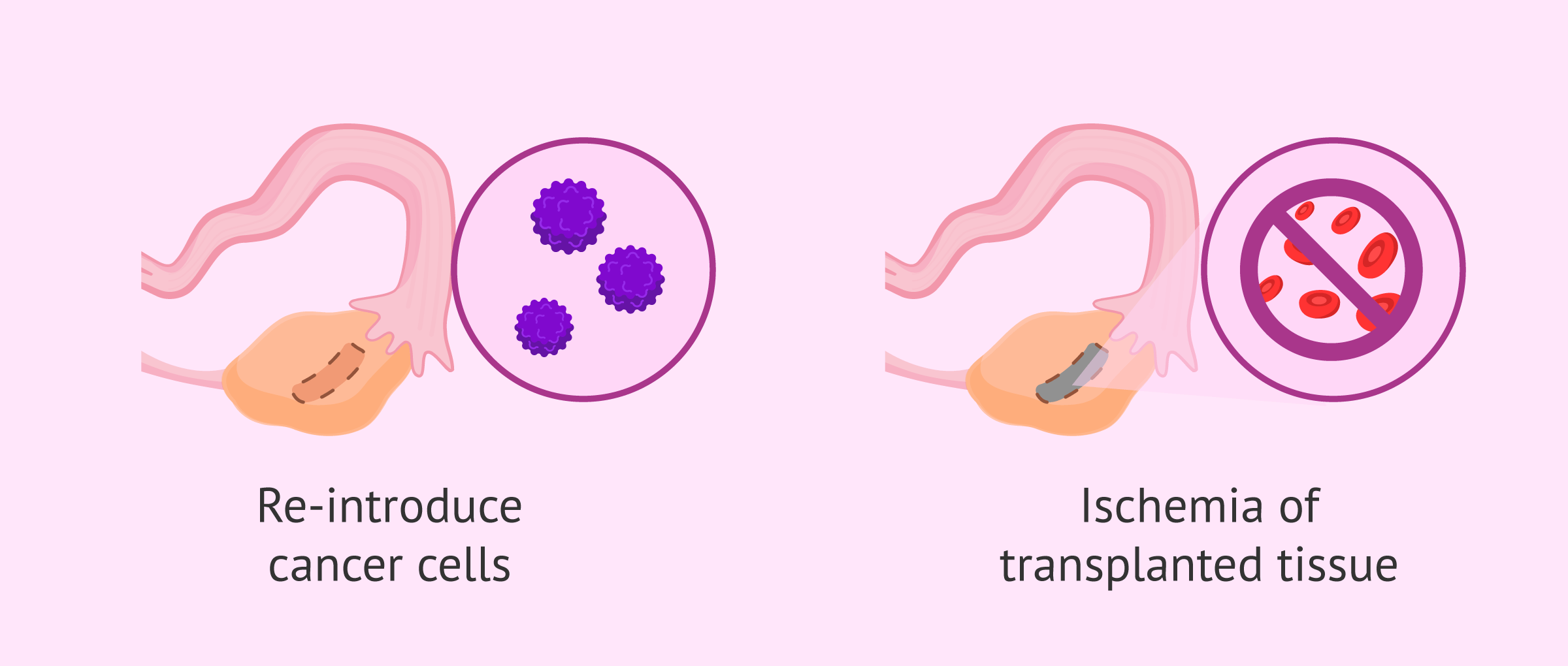
- One of the major drawbacks of this technique is the fear of reintroducing cancer cells into the patient's body through tissue transplantation. This is the case with certain types of cancer, such as some leukemias, where the ovarian graft has reintroduced cancer cells into the patient. This is why several strips of ovarian tissue need to be cut and tested to reduce the number of cancer cells that can be reimplanted. In cases of girls at very early ages, preservation of ovarian tissue remains the preservation technique of choice. This is because it is not ruled out that better techniques for detecting cancer cells in the graft to be transplanted will be developed in the future, or that in vitro oocyte maturation techniques will progress successfully.
- Another problem faced by patients who undergo this technique is the ischemia of the transplanted tissue. This means that after the transplant the tissue does not revascularize correctly and the primordial oocytes die because they do not receive the necessary supply of nutrients and blood. Fo this, the transplant of the entire ovary is being studied, with the aim of reducing ischemia and ensuring that the supply of nutrients and blood reaching the ovary is as necessary.
One option still under study is the extraction of the primordial follicles from the ovarian tissue and their maturation in the laboratory. In vitro maturation (IVM) consists of bringing the primordial oocytes to complete maturation in the assisted reproduction laboratory. This technique offers good hope for those patients who need to preserve their fertility from the time they are children, or cannot receive hormonal stimulation. Despite the fact that this method has taken more than 20 years of experimentation, optimal results have not yet been obtained in order to offer it safely. However, it is hoped that in the future, this technique will be optimized and can be a solution for all those oncology patients who today have their ovarian tissue cryopreserved.
Although today there have already been cases of pregnancy and full-term gestation with transplanted ovarian tissue, this technique is still in the experimental phase. It should be noted that the transplantation of ovarian tissue is a technique with great future projection, so it is recommended to all pre-pubescent cancer patients, while waiting for further progress in this field.
FAQs from users
In which women is the preservation of ovarian tissue indicated?
The freezing of ovarian tissue is part of the fertility preservation techniques that are currently available for those women who, in the face of oncological or surgical treatments, may put their reproductive capacity at risk.
The procedure consists of the surgical extraction of the most superficial layer of one of the ovaries and the conservation in liquid nitrogen with cellular protective means. Once the oncological or surgical process is over, that fragment of ovary will be placed again in the place from which it was extracted.

At present, the speed of programming ovarian stimulation cycles to obtain oocytes for cryopreservation means that the preservation of ovarian tissue is relegated to those cases in which oncological/surgical treatment must be applied immediately, when the patients are girls who have not yet had their first menstruation or in those patients with pathologies in which ovarian stimulation to obtain oocytes is contraindicated.
Is there enough time left to freeze eggs before cancer treatment?
Cancer treatment may occasionally require removal of the ovaries or administration of chemotherapy or radiation therapy. This often results in a loss of fertility. However, in many situations, with adequate planning it will be possible to preserve the fertility of these patients so that they can become mothers in the future. The most important thing in this sense is to consult a fertility specialist as soon as the malignant pathology is diagnosed.
Read more
How do treatments such as chemotherapy or radiation therapy affect a person's fertility?
It has been known for years that cancer treatments damage the male and female germ line. Until recently, the priority in the face of cancer was to be cured. Due to the great advances achieved in the treatment of cancer and the high survival rates that are obtained today in some types of tumours, the importance of controlling the side effects of these treatments is gaining ground. One of them is infertility and, although men have been able to store sperm from the ejaculate for years, today women can also freeze eggs and ovarian tissue.
Suggested for you
Advances in oncology treatments and assisted reproduction have meant that patients who have suffered from cancer can have children after their oncology treatment. If you want to know more about preserving fertility in oncological patients, we recommend the article Fertility Preservation- Cost & Options for Retaining Your Fertility.
Also, don’t miss out on our article How does cancer affect fertility in men and women? to keep you informed about how cancer and its treatments can affect your fertility.
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Remohí J, Bellver J, Ferrando M, Requena A, Pellicer A. Manual práctico de Esterilidad y Reproducción Humana: Aspectos clínicos. 5ª edición. 2018, Editorial Médica Panamericana, S.A.
Peña P. Atención Integral de la Infertilidad: Endocrinología, cirugía y reproducción asistida. 4ª edición. 2020, Editorial Médica Panamericana, S.A.
Anderson RA, Wallace WHB, Telfer EE. Ovarian tissue cryopreservation for fertility preservation: clinical and research perspectives. Hum Reprod Open. 2017; 2017(1): hox001.
GrisJM y Callejo J. Preservación dela fertilidad: estrategias en pacientes sometidas a tratamientos citotóxicos antes de recurrir a la donación de ovocitos. En: Donación de Ovocitos. Nadal J. Ed: Momento Médico Iberoamericana 2010.
GrisJM y Callejo J. Preservación dela fertilidad: estrategias en pacientes sometidas a tratamientos citotóxicos antes de recurrir a la donación de ovocitos. En: Donación de Ovocitos. Nadal J. Ed: Momento Médico Iberoamericana 2010.
Oktay K, Harvey BE, Partridge AH, Quinn GP, Reinecke J, Taylor HS, Wallace WH, Wang ET and Loren AW. Fertility Preservation in Patients with Cancer. DOI: 10.1200/JCO.2018.78.1914
American Society of Clinical Oncology. ASCO Recommendations on Fertility Preservation in Cancer Patients: Guideline Summary. J Oncol Pract. 2006;2(3):143-146.
Metzger ML, Meacham LR, Patterson B, et al. Female reproductive health after childhood, adolescent, and young adult cancers: Guidelines for the assessment and management of female reproductive complications. J Clin Oncol. 2013;31(9):1239-1247.
Nieman CL, Kazer R, Brannigan RE, et al. Cancer Survivors and Infertility: A Review of a New Problem and Novel Answers. J Support Oncol. 2006;4:171-178.
FAQs from users: 'In which women is the preservation of ovarian tissue indicated?', 'Is there enough time left to freeze eggs before cancer treatment?' and 'How do treatments such as chemotherapy or radiation therapy affect a person's fertility?'.
Authors and contributors