Follicular puncture, also known as ovarian puncture, is one of the fundamental steps in In Vitro fertilization (IVF).
It is a surgical intervention whose objective is to obtain the eggs from the interior of the follicles of the ovary. It is a simple and short process that is performed under anesthesia (sedation).
Provided below is an index with the 9 points we are going to expand on in this article.
- 1.
- 2.
- 2.1.
- 2.2.
- 2.3.
- 2.4.
- 3.
- 4.
- 5.
- 6.
- 6.1.
- 6.2.
- 6.3.
- 6.4.
- 6.5.
- 6.6.
- 6.7.
- 6.8.
- 6.9.
- 7.
- 8.
- 9.
What is ovarian puncture?
Follicular or ovarian puncture is a simple intervention that is performed in order to remove the ovules from the woman. It is a short-term process and is performed under anesthesia, so the woman will not feel pain. However, it is possible that the woman notices some discomfort after the ovarian puncture.
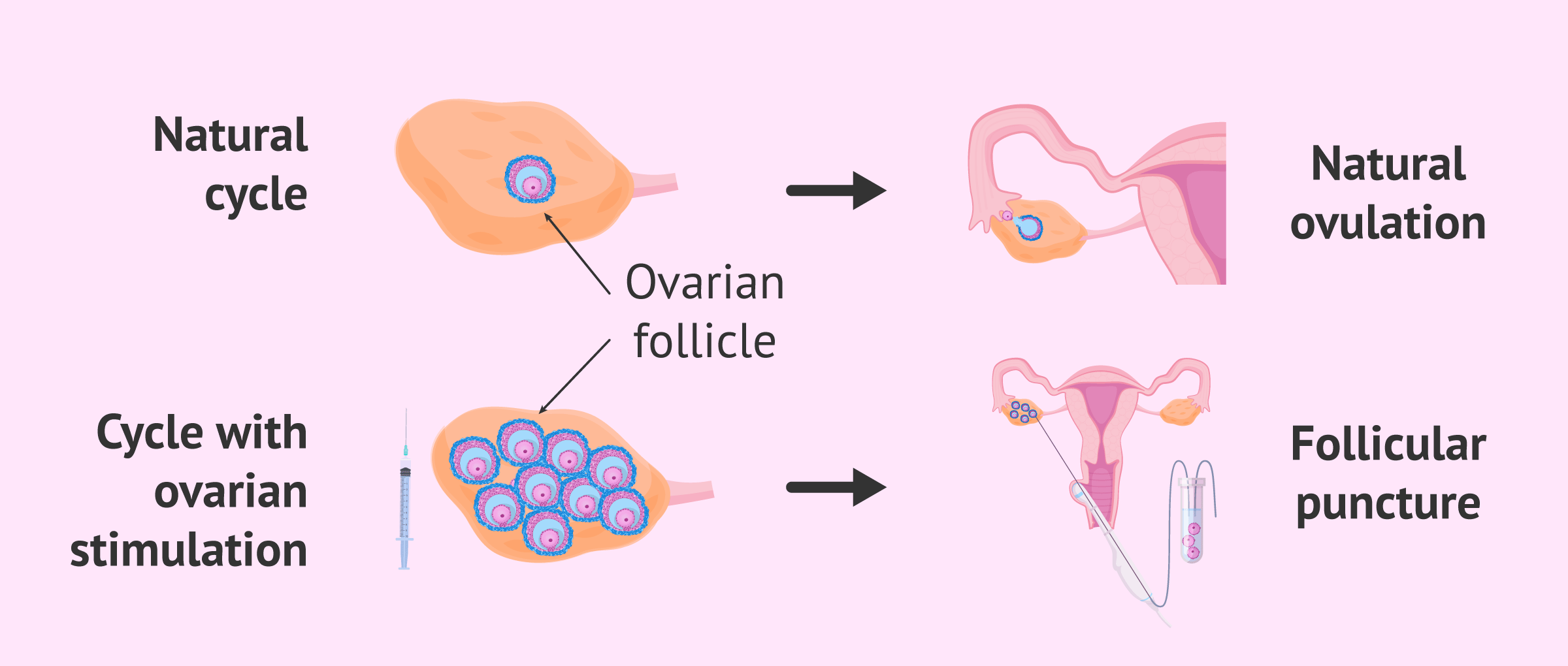
Naturally, each month, an egg is released from the ovary in the process known as ovulation. When we carry out an IVF cycle, the patient receives a hormonal ovarian stimulation treatment to promote the maturation and ovulation of the largest possible number of eggs.
However, in order to fertilize the eggs in the laboratory, we must obtain them before they leave the ovary spontaneously and we are unable to locate them. Therefore, follicular puncture must be performed moments before natural ovulation.
If you would like to learn more about ovarian stimulation, do not forget to visit the following article: What is ovarian stimulation? - Process, medications, and symptoms.
Follicle aspiration procedure step by step
Since the objective is to extract the eggs when they are at a mature stage that allows fertilization (metaphase II), it is essential to schedule the puncture at the right time. To this end, during the ovarian stimulation treatment, follicular growth is monitored by measuring the size of the follicles by transvaginal ultrasound and the concentration of the hormone estradiol in the blood.
The patient should attend these controls approximately every two days. If you want more information about this step you can click here: Controlled ovarian stimulation.
A follicle is said to be mature, that is, it contains a mature egg inside, when it has a diameter greater than 16-18 mm. When it is observed that the follicles have reached this size, the woman is administered the hormone hCG, which favors the final maturation of the eggs and triggers ovulation between 36 and 48 hours after its administration.
Although there may be variations from one center to another, in general, the steps in this process are as follows.
Hospitalization
The patient is admitted to the center the same day the eggs are to be extracted, approximately one hour before the follicular puncture. It is important that the woman brings the preoperative study and the preanesthetic review that the specialists will have done beforehand for the sedation.
The woman should come calm and on an empty stomach to the ovarian puncture, at least during the 6 hours prior to the intervention. It is a simple operation and of short duration (30 minutes approximately) and that same day, she will be able to return home.
Anesthesia
The patient enters the operating room on her own feet and is placed in a gynecological position. The anesthesiologist then administers sedation, i.e. mild anesthesia. Therefore, recovery is quick and the patient remains in the center for a short time after the ovarian puncture.
It is not a complex procedure, but it requires anesthesia to avoid pain and to make the removal more comfortable for the gynecologist.
Follicle aspiration
Once the patient is asleep, the gynecologist proceeds with the ultrasound-guided follicular aspiration. For this purpose, the specialist introduces the ultrasound machine with the aspiration needle incorporated and punctures the ovarian follicles and aspirates the liquid.
The oocytes are floating in this liquid so that when the liquid is aspirated it passes directly into the test tubes, which are at a temperature of 37°C. The tubes are then transferred to the laboratory, maintaining the temperature at all times. Here the embryologists will analyze the follicular fluid for mature eggs.
The mature eggs obtained will be fertilized in the laboratory with the sperm of the male partner or a donor and checked to see if fertilization has occurred.
Recovery and rest
Once the ovarian puncture is finished, that is, when the gynecologist has already punctured all the ovarian follicles, the patient is transferred to a room. There, he will remain a few hours at rest, recovering from the effects of anesthesia.
After this time and after verifying that everything is fine, the patient returns home. It is possible that that same day you will feel small discomfort derived from the intervention, but they will not prevent you from continuing with your usual routines the next day generally.
Potential risks and side effects
Ovarian aspiration is a simple surgery that is performed under mild anesthesia or intravenous sedation. Therefore, the risks that may result are low. The anesthesia may give rise to side effects such as discomfort, dizziness, drop in blood pressure, or vomiting, but this occurs very rarely.
As for the procedure itself, one of the main risks that may result from ovarian puncture is an injury to the pelvic organs, which may, in turn, cause pelvic hemorrhage and infection.
To avoid possible complications, it is important that the gynecologist perform an adequate ultrasound inspection of the pelvis to rule out the accumulation of blood in the fundus of the pouch of Douglas.
Recommendations for puncture
One of the essential requirements for the puncture to proceed normally and not involve secondary or unforeseen effects is absolute fasting. You should not eat or drink for 6 hours before the puncture.
It is recommended that the patient come accompanied to the clinic, since, due to sedation, the woman may feel disoriented after the intervention. The woman can leave the center shortly after the puncture is performed. It is advisable to wait a reasonable time of a few hours to recover from local anesthesia.
In addition, discomfort or small vaginal bleeding may occur after the intervention. The most appropriate thing is to rest that same day and not make great efforts to give the body time to fully recover.
Whether you need to undergo IUI or IVF to become a mother, we recommend that you get your Fertility Report now. In 3 simple steps, it will show you a list of clinics that fit your preferences and meet our strict quality criteria. Moreover, you will receive a report via email with useful tips to visit a fertility clinic for the first time.
Interview to Embryologist María de Las Heras & Dr. Gorka Barrenetxea
María de Las Heras Martínez, BSc, MSc, and Gorka Barrenetxea, MD, Ph.D., explain in this video what is follicle puncture or oocyte retrieval, the improvements achieved today, and the clinical uses of the procedure.
FAQs from users
Is it possible to perform the puncture if there is an endometrioma?
Follicular puncture is a simple procedure performed to extract eggs from patients undergoing controlled ovarian stimulation in assisted reproduction treatments. It is a procedure that is performed under sedation and on an outpatient basis.
Previously, the patient will have attended her check-ups during the stimulation and, once her doctor finds that the follicles that have developed during the cycle have reached a mature size (18-20 mm), the puncture will be scheduled. On this day, the patient will come to the clinic on an empty stomach so that once in the operating room, the anesthesiologist can proceed with the sedation and, by ultrasound, perform the follicular aspiration procedure.
When the follicular puncture is performed by ultrasound, the doctor in charge of performing it will observe if any image compatible with endometrioma is evident, avoiding puncturing this image and proceeding to the aspiration of all the follicles that grew during the stimulation.
Is it advisable to perform ovarian puncture with hyperstimulation?
It should be clarified that ovarian hyperstimulation syndrome occurs after ovulation, usually after the administration of HCG. For this reason, punctures are never performed in hyperstimulation, but rather at the risk of hyperstimulation.
When a patient is at risk of hyperstimulation, it is possible to perform different strategies:
- Lowering or stopping the administration of gonadotropins
- will decrease the ovarian quality, but the probability of hyperstimulation is reduced.
- Avoid administering HCG (Ovitrelle)
- reduces hyperstimulation to practically zero. It is the most widely used strategy today.
- Follicular punction
- reduces ovarian volume, the discomfort associated with hyperstimulation, and may reduce the number of active granulosa cells, thus helping to prevent the syndrome.
What is recommended when only three eggs are obtained in the ovarian puncture of an IVF cycle?
The number of oocytes that will be obtained in an In Vitro Fertilization cycle is predictable, through the antral follicle count and the determination of the AMH hormone prior to the ovarian puncture.
Thus, usually, the fact of obtaining only three follicles (or less) should have been previously discussed with the woman or couple who will undergo the treatment. It is at this point, prior to any treatment, that a joint strategy must be developed between the physician and the patient to manage this low ovarian response.
Once the cycle has been completed, there are two options. The first would be to freeze the oocytes, carry out a new cycle (or several) and accumulate oocytes. Subsequently, an In Vitro Fertilization would be carried out as usual. For example, three cycles with 3 oocytes would mean a treatment in which theoretically 9 oocytes would be used. This means a cost saving, since the laboratory work will only be carried out on one occasion, although it may mean the loss of those oocytes that do not withstand the freezing and thawing process.
The second would consist of concluding the IVF. The probability of gestation may be sufficient, depending on the case (age of the woman, ovarian quality, seminal quality, etc.). Each case must be evaluated individually and by the medical team.
Is there any serious risk associated with the egg retrieval procedure?
Follicular puncture or oocyte retrieval is a mild procedure that involves little risk of complications.
The most severe risks that can occur during or after this procedure are damage to pelvic organs (intestines, bladder...), bleeding, or infections. These complications are very rare, as it is an ultrasound-guided procedure, which means that the gynecologist can monitor the sites being approached.
Other side effects, though less severe, include dizziness and vomiting due to anesthesia, or abdominal pain during the first days after the procedure.
When is egg retrieval required?
Follicle puncture is done only when retrieving the eggs from the ovary is needed, either for in vitro fertilization with own or donated eggs. It is also done for fertility preservation, as it involves obtaining and freezing the eggs for later use.
Is the egg harvesting process painful?
Ovum pick-up is done under anesthesia, and therefore it does not hurt at all. However, it is possible for patients to feel a mild discomfort before the procedure due to an increased ovarian size caused by ovarian stimulation.
Can egg retrieval be done without anesthesia?
It is a possibility, but the procedure would be too painful. Besides, if it hurts, the gynecologist cannot proceed with aspiration accurately, so the results would be poorer, the number of complications would increase, and the process would take longer.
Is it normal to feel abdominal pain after egg retrieval?
Yes, many women feel some mild discomfort around the area of the abdomen and the vagina as a side effect of follicle puncture. Normally, pain only lasts for one or two days, but it diminishes eventually until it disappears completely within a few days.
Is the egg collection procedure carried out in exactly the same way to the ICSI?
Yes, conventional IVF and ICSI differ in the way the egg is fertilized, which is to say, at the moment of fusing the egg and the sperm, but the remaining steps are exactly the same.
Ovarian stimulation, ovum pick-up, embryo culture and embryo transfer do not change at all. More detailed information here: In vitro fertilization and ICSI.
Recommended readings
Once the eggs have been retrieved and fertilized in the laboratory, it is necessary to wait for viable embryos to develop before transferring them to the woman's uterus. If you would like to learn more about this stage of IVF, you can visit the following article: Embryo transfer: when and how it is done.
On the other hand, IVF can be performed conventionally or by intracytoplasmic sperm injection, also called ICSI. The choice of one technique or the other will depend on each particular case. If you would like more information on this subject, we invite you to visit this link: IVF or ICSI: Which is better, what is the difference?
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Bennett, SJ, Waterstone JJ, Cheng WC, Parsons J. Complications of transvaginal ultrasound-directed follicle aspiration: a review of 2670 consecutive procedures. J Assist Reprod Genet 1993;10:72-7.
Borlum KG, Maiggard S. Transvaginal oocyte aspiration and pelvic infection. Lancet 1989;2:53-4.
Dickey RP, Taylor SN, Lu PY, Sartor BM, Rye PH, Pyrzak R (2002). Effect of diagnosis, age, sperm quality, and number of preovulatory follicles on the outcome of multiple cycles of clomiphene citrate-intrauterine insemination. Fertil Steril;78:1088 – 1095.
Dicker D, Ashkenazi J, Feldberg D, Levy T, Dekel A, BenRafael Z. Severe abdominal complications after transvaginal ultrasonographically guided retrieval of oocytes for IVF & ET. Fertil Steril 1993;59:1313-15.
El-Shawarby SA, Margara RA, Trew GH, Lavery SA. A review of complications following transvaginal oocyte retrieval for in-vitro fertilization. Hum Fertil 2004;7(2):127-33.
Hamoda H, Sunkara S, Khalaf Y, Braude P, El-Toukhy T. Outcome of fresh IVF/ICSI cycles in relation to the number of oocytes collected: a review of 4,701 treatment cycles. Hum Reprod 2010;25:147.
Klemetti R, Sevon T, Gissler M, and Hemminki E. Complications of IVF and ovulation induction. Hum Reprod 2005;20(12):3292-300.
Molina Hita Ma. del M, Lobo Martinez S, Gonzalez Varea, Montejo Gadea JM, Garijo Lopez E, Cuadrado Mangas C. Correlation between the number of oocytes and the pregnancy rate in IVF-ICSI cycles. Revista Iberoamericana de Fertilidad y Reproduccion Humana 2008; 25:153 – 159. Spanish.
Paulson RJ. Oocytes from development to fertilization. In: Lobo RA, Mishell DR Jr, Paulson RJ, Shoupe D, editors. Infertility, contraception and reproductive endocrinology. 4th ed. Cambridge: Blackwell Scientific Publications, 1997:174–82.
Paulson RJ, Marrs RP. Ovulation stimulation and monitoring for in vitro fertilization. Curr Probl Obstet Gynecol Fertil 1986;9:497–526.
FAQs from users: 'Is it possible to perform the puncture if there is an endometrioma?', 'Is it advisable to perform ovarian puncture with hyperstimulation?', 'What is recommended when only three eggs are obtained in the ovarian puncture of an IVF cycle?', 'Is there any serious risk associated with the egg retrieval procedure?', 'When is egg retrieval required?', 'Is the egg harvesting process painful?', 'Can egg retrieval be done without anesthesia?', 'Is it normal to feel abdominal pain after egg retrieval?' and 'Is the egg collection procedure carried out in exactly the same way to the ICSI?'.
Authors and contributors

More information about Cristina Algarra Goosman









Hi, tomorrow I am going to have an ovarian puncture for our first IVF cycle, I wonder why they ask me to go on an empty stomach? Thank you
Hi Becky,
Generally going on an empty stomach for an ovarian puncture is for several reasons. This process is still a surgical procedure that requires anesthesia, so it requires that there is no food in the stomach.
Also, if anything were to happen during the operation, the doctors can intervene without having to worry about the blood values, since these will be basal since you have not eaten food in the last few hours.
I hope I have helped you!
Best of luck
Hello, I had an ovarian puncture a few days ago and I have discomfort in the intimate area, especially when having sexual intercourse with penetration, is it normal? I don’t know if I should be worried
Hello Doja,
Having discomfort in the area after an ovarian puncture is considered normal since a surgical intervention has been performed in the area and there may be wounds or injuries.
It is generally recommended to wait to have sexual intercourse with penetration until a couple of weeks have passed and there is no pain in the area.
If the pain lasts more than a couple of weeks I recommend that you go to the doctor to explore you and see if there is a problem.
I hope I have helped you