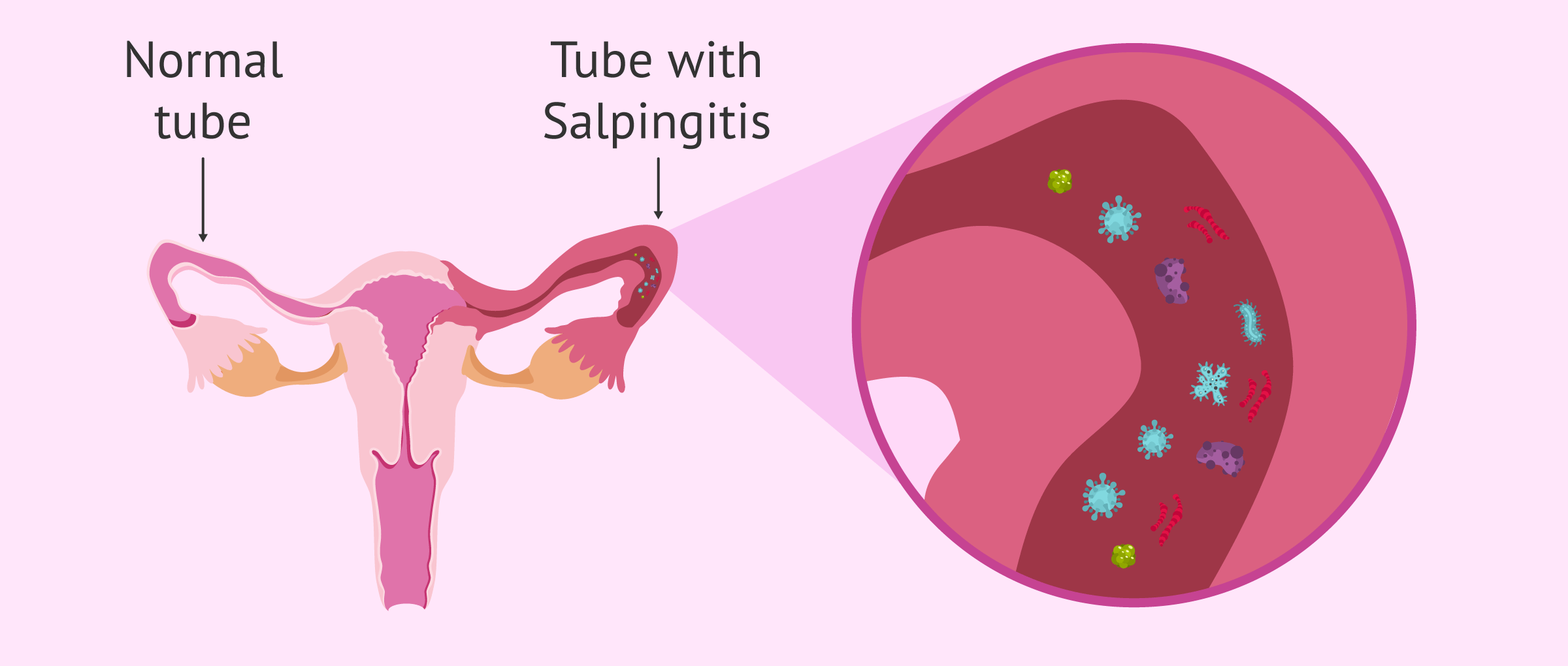
Salpingitis is a type of pelvic inflammatory disease (PID) that involves inflammation of the fallopian tubes.
This inflammation of the fallopian tubes is one of the causes of infertility of tubal origin and increases the chances of ectopic pregnancy, that is, embryonic implantation outside the uterus.
The symptoms of salpingitis can be various, but most symptomatic patients report pain in the pelvic area. The treatment of salpingitis is based on the administration of antibiotics.
Provided below is an index with the 10 points we are going to expand on in this article.
- 1.
- 2.
- 3.
- 3.1.
- 4.
- 4.1.
- 5.
- 6.
- 7.
- 7.1.
- 7.2.
- 7.3.
- 7.4.
- 7.5.
- 7.6.
- 8.
- 9.
- 10.
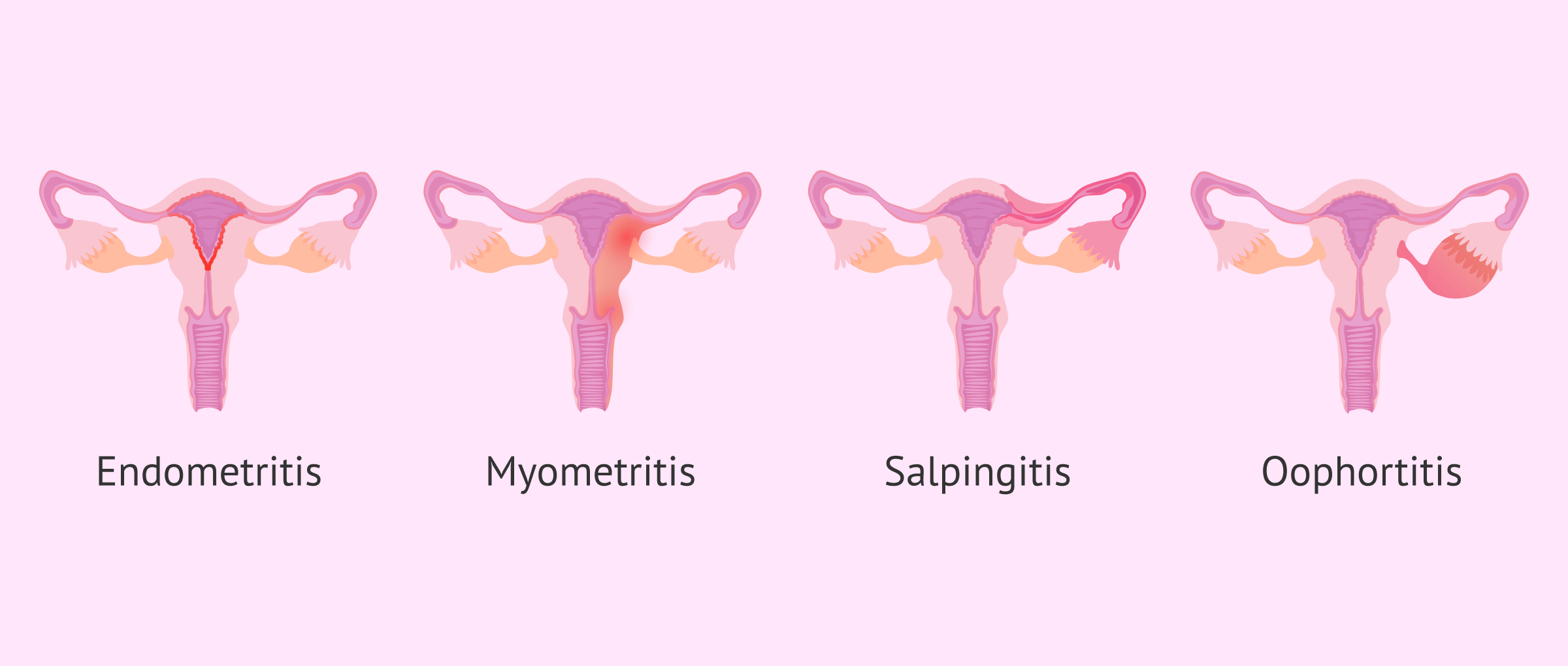
Pelvic inflammatory disease
Pelvic inflammatory disease is inflammation and infection of the upper genital tract. It can affect:
- Endometrium (endometritis)
- Myometrium (myometritis)
- Fallopian tubes (salpingitis)
- Ovaries (oophoritis)
- Parametrium (parametritis)
- Peritoneum (Peritonitis)
Any PID is caused by bacteria from the vagina or cervix that ascend to one of these structures and cause an infection. The most common are chlamydia (Chlamydia trachomatis) and gonorrhea (Neisseria gonorrhoeae), which are sexually transmitted diseases (STDs). Furthermore, infection by one of these pathogens increases the transmissivity of HIV and other STDs.
If you want more information about PIDs, we recommend you visit the following article: What is Pelvic Inflammatory Disease?
Types of Salpingitis
There are two main types of salpingitis:
- Acute Salpingitis
- is the one with the worst symptoms (fever, acute pain in the lower part, etc.).
- Chronic salpingitis
- can go unnoticed (asymptomatic) and mostly occurs after the menstruation.
Depending on whether it affects one or both tubes, a distinction is made between unilateral and bilateral salpingitis, respectively. Approximately 60% of cases are bilateral, i.e. both tubes are affected.
What are the causes of salpingitis?
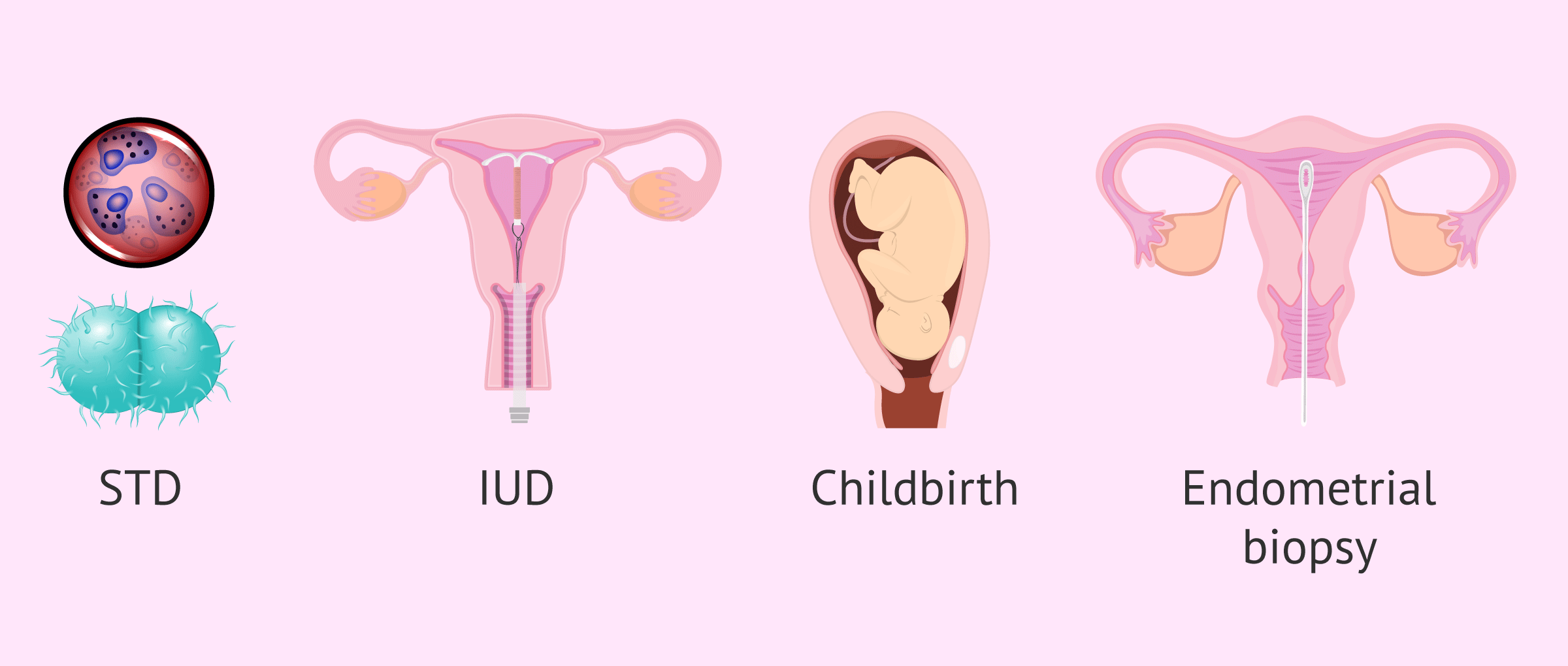
Salpingitis usually affects women of childbearing age and it occurs in 10-15% of sexually active women, as one of the most common causes of inflammation of the tubes are genital infections, especially sexually transmitted infections.
About 40% of sexually transmitted infections end in salpingitis.
In most cases, salpingitis is caused by a type of chlamydia, the Chlamydia trachomatis. Infection usually begins in the vagina and then moves up to the upper genital tract.
Other possible pathogens that are sexually transmitted and cause this type of inflammation are gonococcus (gonococcal salpingitis) and some types of mycoplasma which occur less frequently.
30-40% of cases of salpingitis are of polymicrobial cause and, among the causative microorganisms, we can find some of the vaginal flora.
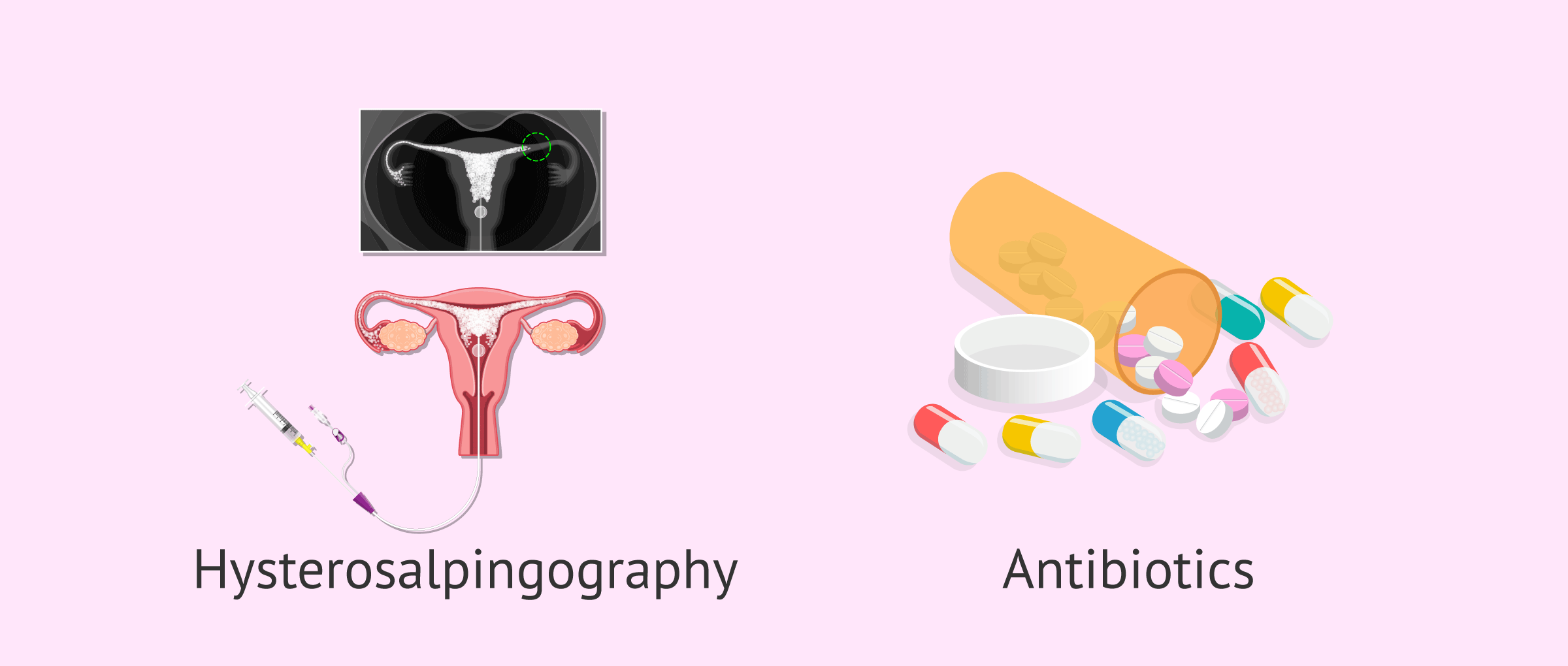
Bacteria can also reach the upper genital tract through medical procedures, such as the placement of an intrauterine device (IUD) or any invasive test that is capable of dragging microorganisms from the vaginal flora. Examples of these techniques include childbirth, miscarriage, endometrial biopsy, hysterosalpingography, and hysteroscopy.
It may also be a bloodborne infection, as in the case of tuberculosis. If the infection is caused by Mycobacterium tuberculosis, we are talking about tuberculous salpingitis.
Risk Factors
There are some situations or factors that may increase your risk of salpingitis. The most common are the following:
- Couple with any type of genital infection, especially gonorrhea or chlamydia.
- Prior pelvic surgery.
- Use of IUD.
- History of pelvic inflammatory disease.
- History of sexually transmitted disease.
- Multiple sexual partners.
- Having sexual activity before age 20.
However, the presence of any of these factors does not mean that the development of salpingitis is 100% probable, it only increases the risk of suffering from this tubal alteration.
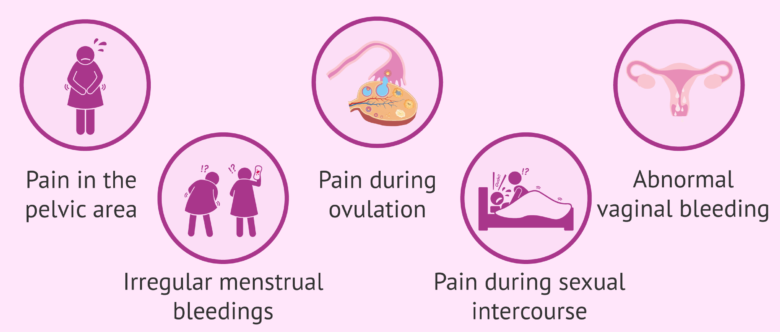
What symptoms does salpingitis cause?
Salpingitis manifests itself over time in a variable way and can go from 2 days to 3 weeks or even months after having had contact with the pathogen.
The fact that there are patients with the infection who have no symptoms makes it easier to become infected and the chances of complications are higher.
The symptoms of salpingitis may vary depending on the microorganism that acts, but the most characteristic of them is pain in the pelvic area.
Other symptoms that may appear are:
- Abnormal vaginal discharge with thick discharge
- Pain during ovulation
- Unpleasant, uncomfortable, and even painful sexual intercourse (dyspareunia)
- Fever
- Nausea and vomiting
- Irregular menstrual Bleeding
- Pain when urinating (dysuria), if accompanied by urethritis (inflammation of the urethra)
- Vaginitis
- Cramps in the pelvic area
In any case, salpingitis symptoms usually appear after menstruation, but they can also appear before menstruation, after childbirth or in cases of miscarriage.
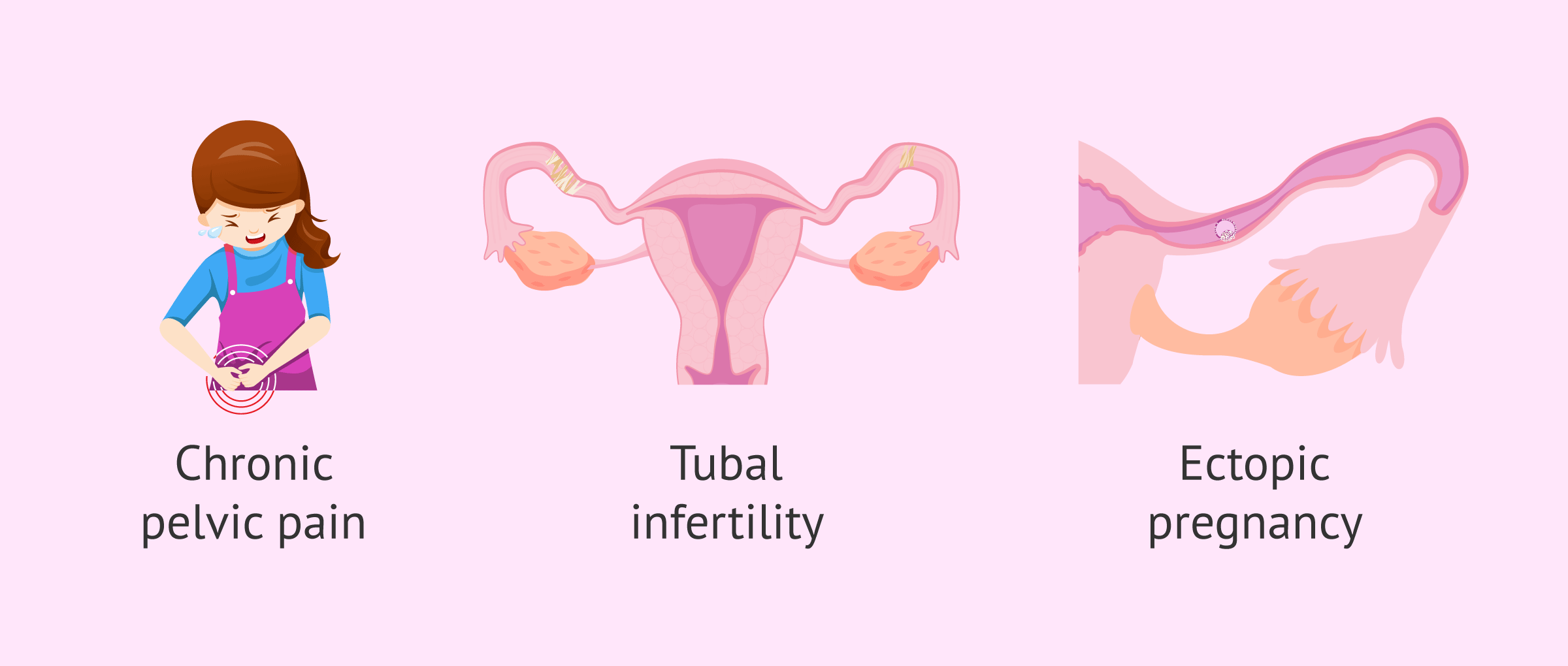
Complications of Salpingitis
Some of the complications that can occur in women suffering from salpingitis are the following:
- Chronic pelvic pain.
- Tubal factor infertility.
- Ectopic pregnancy.
- Recurrent pelvic inflammatory disease.
- Pelvic abscess.
- Generalized sepsis or infection
- Liver and appendix involvement.
However, these complications do not always occur, but it is important to consult with the specialist for any symptoms that appear in order to know how to proceed.
Diagnosis and Treatment
To diagnose salpingitis, the patient's symptoms and sexual history are considered, and a physical examination is performed. Only the most serious cases of salpingitis can be detected by ultrasound, though any other pathology can be ruled out.
A microbiological analysis of vaginal secretions can also be performed to detect and identify any pathogen infection.
Generally, if the diagnosis is made early, the inflammation subsides with medication. However, a late diagnosis can lead to more serious complications requiring more invasive treatment and sequels are more likely.
As this is an inflammation normally caused by a bacterial agent, the treatment of choice is the pharmacological one, which consists of antibiotic and anti-inflammatory pain medication.
The antibiotic used will depend on the microorganism that causes the infection. Some of those users are doxycycline, azithromycin, erythromycin, or levofloxacin.
The patient's partner should also be treated with antibiotics and it is advisable to avoid sexual intercourse until one week after the end of the treatment.
In the most severe cases, if outpatient treatment is not effective, hospitalization of the patient may be necessary.
If the infection of the fallopian tubes becomes complicated, surgical treatment will be undertaken. If a pelvic abscess develops with a collection of pus, drainage surgery may be necessary. In more severe cases, salpingectomy (removal of the tubes) may also be required.
Salpingitis, sterility and infertility
The fact that a large percentage of patients have subclinical (symptomless) chlamydial infection means that it remains untreated and spreads to the upper genital tract. These subclinical cases are the origin of most cases of sterility (difficulty in conceiving) due to tubal factor.
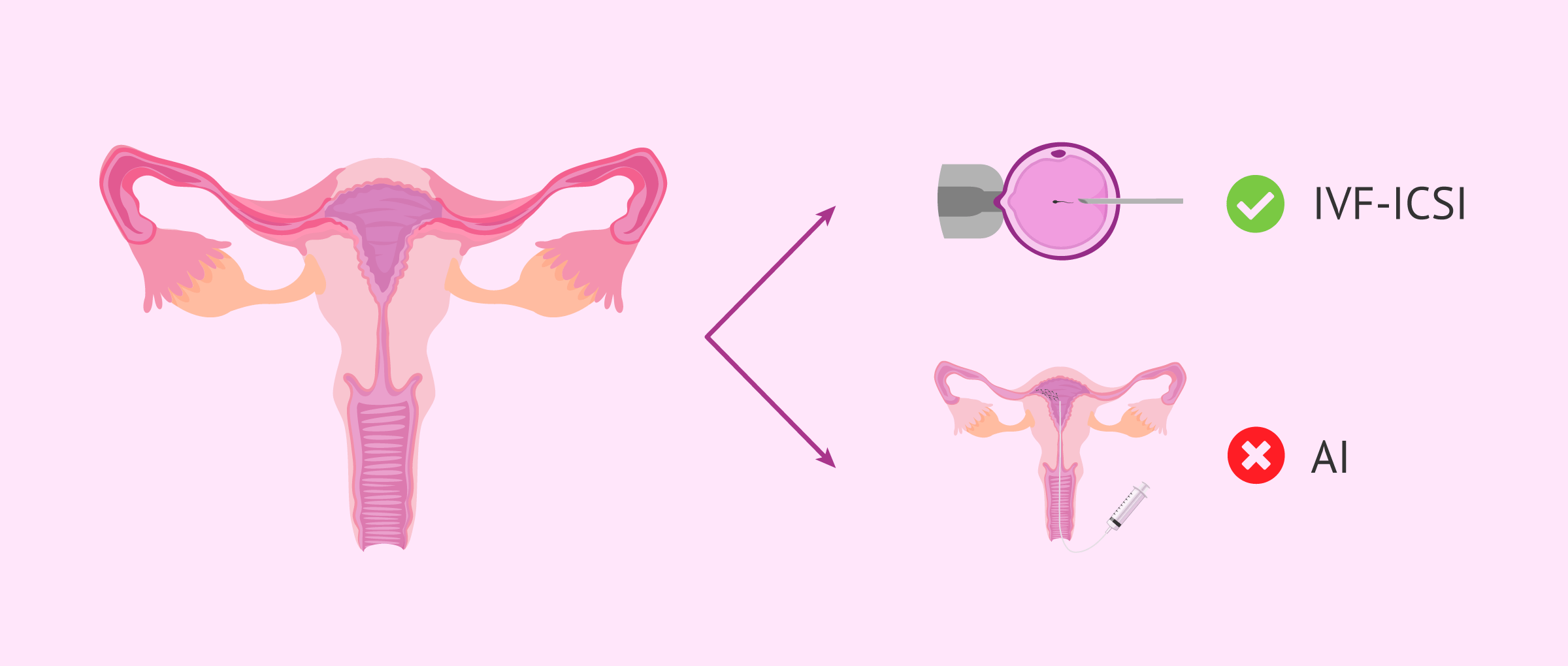
The inflammation of the structures of the fallopian tubes causes the permeability of the tubes to be altered. This causes a mechanical obstacle in the path of the egg to the uterus, making it difficult for it to meet the sperm. Therefore, it prevents fertilization from happening.
Furthermore, in 50% of ectopic pregnancies this clinical background exists. It has also been shown that approximately 20% of abortion patients are infected with chlamydia. Therefore, it is also a cause of infertility (difficulty in carrying a pregnancy to term).
If the tubes are still altered after treatment and there is a desire to gestate, the indication will be an in vitro fertilization (IVF) treatment, since with artificial insemination, due to this alteration, pregnancy would not be achieved.
Assisted procreation, as any other medical treatment, requires that you rely on the professionalism of the doctors and staff of the clinic you choose. Obviously, each clinic is different. Get now your Fertility Report, which will select several clinics for you out of the pool of clinics that meet our strict quality criteria. Moreover, it will offer you a comparison between the fees and conditions each clinic offers in order for you to make a well informed choice.
If pregnancy is achieved without treating the chlamydia infection, it can lead to premature delivery and infections in the newborn that can cause conjunctivitis and pneumonia.
FAQs from users
Can salpingitis become really serious?
Only in a minority of cases of salpingitis does peritonitis or pelvic abscess develop, manifesting itself with more intense pain and general symptoms such as fever. If this degree is reached, surgery is sometimes necessary to cure the disease, and the tubes and even the ovaries have to be removed.
In the most severe cases, the process can extend to other abdominal organs such as the liver or even pass into the blood (sepsis), posing a risk to the woman's life.
Read more
Is it necessary to treat salpingitis before starting IVF?
Salpingitis is defined as inflammation/infection of the fallopian tubes, these are tubular structures that communicate the ovaries with the uterus, allowing the ascent of the sperm to fertilize the ovum collected by the ampullary portion, and lead it to the endometrium where it must be implanted.
Inflammation of this anatomical structure in direct communication with the endometrium alters endometrial receptivity and therefore reduces the chances of blastocyst implantation.
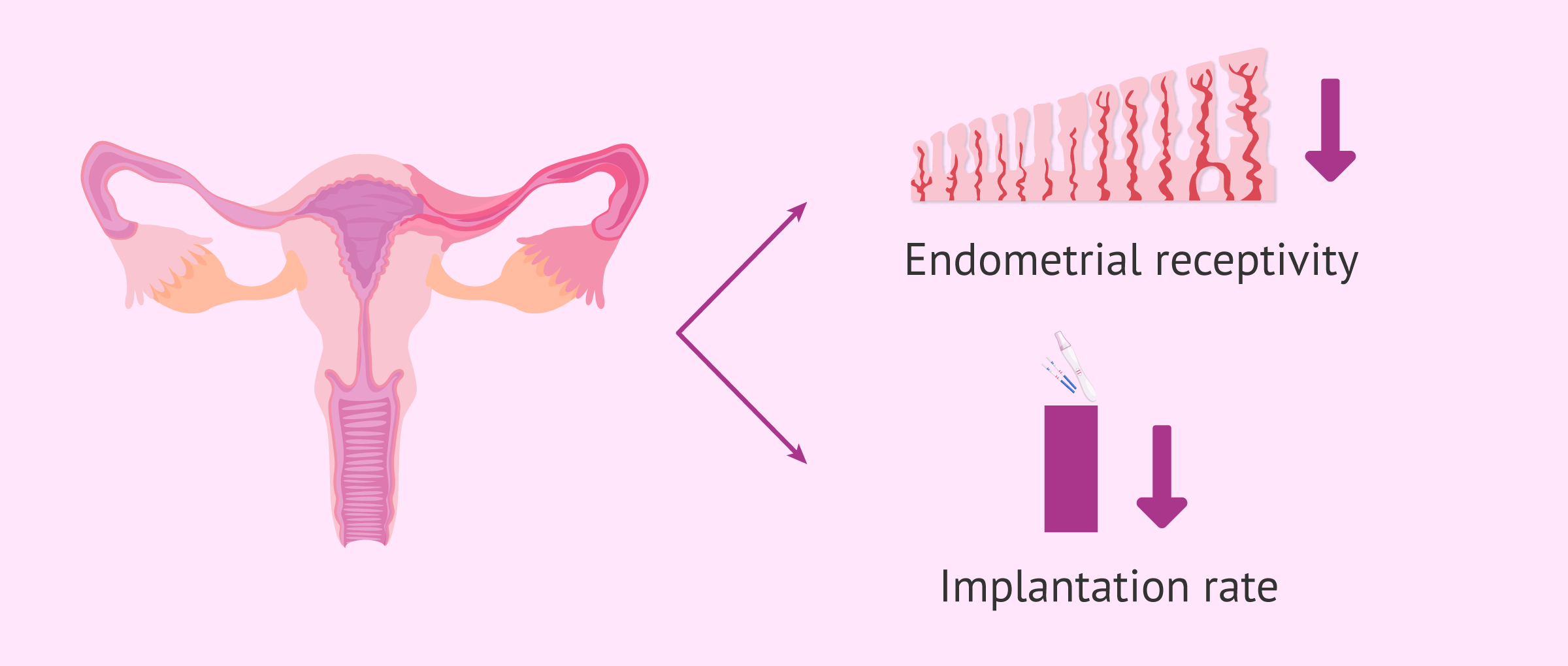
In this case, salpingitis must be treated prior to the start of IVF, or prior to embryo transfer. In most cases, it involves bilateral salpingectomy, removal of both fallopian tubes.
Is there a natural treatment for salpingitis?
In the treatment of salpingitis, absolute rest and a mild nutrition are recommended, but it is also essential to follow an antibiotic treatment, since the complications of this pathology can be very serious.
Do contraceptives protect against salpingitis?
Only barrier contraceptives, such as condoms, can protect against sexually transmitted diseases, which are the main cause of salpingitis.
However, oral contraceptives have been shown to reduce the incidence of these: they cause an increase in the viscosity of cervical mucus, which makes it difficult for microorganisms to enter.
On the other hand, as already mentioned in the article, the IUD is a risk factor for this pathology.
I'm a virgin. Can I still get salpingitis?
It is very rare for these infections to occur without sexual intercourse, but they can also be caused by some medical procedures, such as hysteroscopy.
What is salpingitis isthmica nosoda?
Salpingitis isthmica nosoda, also known as diverticulosis of the Fallopian tube, consists of a nodular thickening of the isthmic portion of the fallopian tubes, although it can also affect their entirety.
It is a progressive and irreversible process that causes infertility and an increased risk of ectopic pregnancy.
The exact cause of this alteration is unknown, although it is most likely to be of an inflammatory origin.
Recommended readings
We've discussed STDs as the most common cause of salpingitis. If you want to know more about the types of sexual infections that exist, you can read more here: Sexually transmitted diseases (STDs) in men and women.
Do you want to learn more about disorders in the fallopian tube? Read more about those disorders as a cause for sterility here: Female tubal factor infertility.
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Dun EC, Nezhat CH. Tubal factor infertility: diagnosis and management in the era of assisted reproductive technology. Obstet Gynecol Clin North Am. 2012 Dec;39(4):551-66 (see)
Hafner LM. Pathogenesis of fallopian tube damage caused by Chlamydia trachomatis infections. Contraception. 2015 Aug;92(2):108-15.
Holmes KK, Eschenbach DA, Knapp JS. Salpingitis: overview of etiology and epidemiology. Am J Obstet Gynecol. 1980 Dec 1;138(7 Pt 2):893-900.
Kurtoglu E1, Kokcu A, Celik H, Kefeli M. Salpingitis isthmica nodosa and recurrent ectopic pregnancy. J Obstet Gynaecol. 2015 Feb;35(2):217-8.
Mårdh PA, Svensson L. Chlamydial salpingitis. Scand J Infect Dis Suppl. 1982;32:64-72.
Sweet RL. Chlamydial salpingitis and infertility. Fertil Steril. 1982 Nov;38(5):530-3.
FAQs from users: 'Can salpingitis become really serious?', 'Is it necessary to treat salpingitis before starting IVF?', 'Is there a natural treatment for salpingitis?', 'Do contraceptives protect against salpingitis?', 'I'm a virgin. Can I still get salpingitis?' and 'What is salpingitis isthmica nosoda?'.
Authors and contributors

More information about Cristina Algarra Goosman





Hello, I have had salpingitis and I would like to know if I will be able to have a normal pregnancy.
Hi Cheyenne,
Salpingitis can have different complications, including tubal infertility. This can affect fertility complicating the achievement of a natural pregnancy.
If such a pregnancy is achieved, it is important to monitor the first few weeks as women who have suffered from salpingitis are more at risk for ectopic pregnancy.
I recommend that you see your doctor before seeking pregnancy so that he/she can examine you and determine if there is any type of malformation or detail that may complicate the pregnancy.
I hope everything goes well,
Best regards
Hi, I have been treated for salpingitis, I have taken antibiotic medication I think, but I don’t think the inflammation or infection has gone away. What should I do?
Hi Jade,
With salpingitis, it is important to take the medication prescribed by the doctor for as long as prescribed. This is the time required to kill the infection and decrease the inflammation.
After the treatment, the most normal thing is that the doctor will see you again for a scan and check that the salpingitis has subsided, if not, another treatment should be prescribed until the infection is not present because if it is not treated it can damage and even require surgery to remove the tissue.
I hope I have helped you,
Best regards
Hey! How are you all? Well, I suffer from endometriosis, but I have all those symptoms you’ve mentioned here, so I think I have also PID. My question here is if endometriosis can be the origin of salpingitis and, if so, why? Thanks!