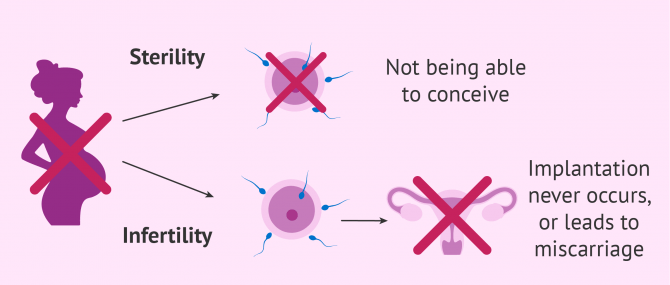
Infertility and sterility are two terms that make reference to the inability to have children. However, and although they are often used synonymously, even by a number of professionals, their meaning is not exactly the same. Subfertility, on the other hand, is defined as the condition of being capable of conceiving, yet less fertile than normal.
In short, the main difference between being infertile and being sterile lies in the precise moment when the problem that prevents pregnancy appears. A subfertile couple are not infertile, but will find conception more difficult. The purpose of this article is to define each one of these concepts in detail.
Provided below is an index with the 8 points we are going to expand on in this article.
- 1.
- 1.1.
- 1.2.
- 2.
- 2.1.
- 2.2.
- 3.
- 4.
- 5.
- 5.1.
- 5.2.
- 5.3.
- 5.4.
- 5.5.
- 5.6.
- 6.
- 7.
- 8.
Meaning of 'sterility' and 'infertility'
The term sterility is defined as the inability to achieve a pregnancy because the fusion between the egg and the sperm, that is, fertilization never occurs.
On the other hand, by infertility we mean the inability to carry a pregnancy to term due to a problem that develops when fertilization has already taken place. In this case, even though the egg-sperm binding does occur, the resulting embryo is unable to implant or cannot develop till the end of the pregnancy, that is, delivery.
In short, the purpose of having a baby cannot be fulfilled in any case. Nevertheless, in cases of infertility, the chances of creating a family are a little bit higher than in cases of sterility, although it might not be possible either.
In everyday language, some examples of words or terms used as synonyms of infertile and sterile include the adjectives barren and unproductive.
Primary and secondary sterility
It should be noted that the concept of sterility can be split into two different types:
- Primary sterility
- A couple whose gametes (egg and sperm) have never been able to cause a pregnancy.
- Secondary sterility
- A couple who have been able to have children previously, but conception does not occur when trying to conceive another child.
Primary and secondary infertility
Also, in the case of infertility, there exist two different types as well, which are defined hereunder:
- Primary infertility
- Those couples who have never achieved a full-term pregnancy.
- Secondary infertility
- The couple have already had a child, but is unable to achieve a full-term pregnancy again.
Causes of sterility in humans
Even though both sterility and infertility are two-way things, the cause behind it might be related to the man, the woman, or both members of the couple. The following is a detailed explanation of the most common causes of sterility and infertility in males and females:
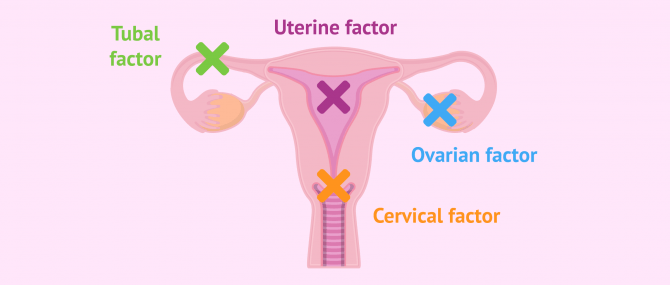
Female sterility
There are several reasons why a woman's reproductive capacity may be affected. The most common reasons for female infertility are as follows:
- Endocrine factor
- refers to problems related to hormonal control of the menstrual cycle and ovulation. This can lead to alterations such as poor oocyte quality, anovulation, amenorrhoea, premature ovarian failure, etc.
- Tubal factor
- these are disorders at the level of the fallopian tubes, which is the place where the egg and sperm unite to create the embryo. Tubal obstruction, endometriosis or salpingitis are some of the tubal disorders that most affect a woman's fertility.
- Cervical factor
- functional and/or anatomical alterations of the cervix can hinder the ascent of the sperm and thus prevent fertilization.
- Uterine factor
- malformations, myomas, synechiae, endometritis, polyps, etc., can prevent the sperm from reaching the egg.
These causes can also be a reason for infertility, because in some cases, despite these disorders, fertilization occurs but the embryo doesn’t develop afterwards.
If you want to learn more, we recommend you to read the following post: Female factor infertility.
Male sterility
Regarding the causes that generate sterility in men, we can talk about the following factors:
- Pre-testicular or endocrine factor
- as in the case of women, alterations in the hormones that regulate spermatogenesis (sperm production) can negatively influence the formation of spermatozoa and thus affect their ability to fertilize.
- Testicular factor
- pathologies such as orchitis, hydrocele, cryptorchidism, trauma or varicocele are some of the most common.
- Post-testicular factor
- even if sperm production is not altered, it is possible that the sperm may have difficulty getting out during ejaculation. Sexual impotence, retrograde ejaculation, obstruction of the Some examples of post-syndromic alterations are: ducts, infections, etc.
- Sperm factor
- it may happen that the quality of the sperm is not good enough to achieve a natural pregnancy. Problems related to motility, morphology or concentration of sperm in the ejaculate can prevent spontaneous gestation.
As in the previous case, although these factors are basically aspects related to sterility, it is possible that, in spite of this, fertilization is achieved but not evolutionary pregnancy. We would therefore be dealing with a case of male infertility.
Are you interested in learning more about fertility issues in men? Then do not miss the following article: Male factor infertility.
'Infertility' versus 'subfertility'
As explained earlier, infertility allows the couple to go one step further in the journey toward pregnancy. In this case, the fusion between the egg and the sperm does occur and results in an embryo. However, the problem with infertility is that the embryo is unable to attach to the maternal uterus or to develop properly until childbirth.
For this reason, one can define the term infertility as the inability to achieve a full-term pregnancy, and bring a healthy baby home. On the other hand, by subfertility we refer to a couple being able to achieve a successful pregnancy, but with more difficulty.
For example, a woman in her 40s is considered to be subfertile, as the chances for pregnancy exist, but are lower in comparison to younger females.
In addition to the reasons listed above, which sometimes can lead to sterility and, in others, to infertility, there exist other causes related to the embryo and its development/growth. The most common ones include:
- Implantation failure
- This abnormality prevents the woman from having a full-term pregnancy, as the embryo is unable to implant into the endometrial lining.
- Miscarriage or pregnancy loss
- Pregnancy occurs, but stops at some point of fetal development, which causes the woman to miscarry.
In short, the cause that prevents full-term pregnancies can appear at early pregnancy, such as in cases of implantation failure, in which embryo implantation is not possible.
Pregnancy might also stop progressing at more advanced stages of fetal development, which leads to miscarriage as well.
Conversely, common causes of subfertility include endometriosis, tubal disease, ovulatory disorders, sperm abnormalities, advancing female age, uterine abnormalities, and peritoneal adhesions.
Male factor infertility, female factor infertility, or even both can be what causes a couple to experience trouble conceiving. Sometimes, however, the cause remains unknown, which is known as unexplained infertility.
Fertility treatments and costs
Nowadays, fertility treatments such as artificial insemination (AI) or in vitro fertilization (IVF), either conventional or by ICSI (intracytoplasmic sperm injection), allow many couples to have children despite having a problem that affects their fertility.
AI is the most economical reproductive technique. Its cost ranges from $300-$1.000, while IVF costs between $10,000 and $15,000.
In the most serious cases of sterility or infertility, there is the possibility of resorting to egg donation and sperm donation in order to start the appropriate reproductive treatment to achieve evolutionary pregnancy, that is to say, to achieve the birth of a healthy child.
The cost of egg donation in the US is between $20,000 and $40,000. Sperm donation, on the other hand, has a more affordable cost because it is a simpler technique. The price of artificial insemination with donor sperm (AID) is between $900-1,000 for one vial of donor sperm and the procedure itself about $200 to $400.
If you need to undergo IVF to become a mother, we recommend that you generate your Fertility Report now. In 3 simple steps, it will show you a list of clinics that fit your preferences and meet our strict quality criteria. Moreover, you will receive a report via email with useful tips to visit a fertility clinic for the first time.
Although mild cases of sterility or infertility can be cured in some cases, it is not always possible to solve the problem. In these situations, assisted reproductive technologies may be the solution to fulfill the dream of having a baby.
FAQs from users
To what extent do lifestyle factors affect fertility?
Whether you're thinking about getting pregnant or have already been trying, it's never too early or too late to evaluate your lifestyle choices. Starting healthy habits or getting rid of bad ones can improve your overall health. And some lifestyle changes may promote fertility in both you and your partner. For example, Smoking cessation, reducing alcohol consumption, eliminating Street drugs, practicing safe sex, avoiding overheating (male), limiting caffeine intake, and exercising regularly.
Is sterility the same as infertility?
Sterility and infertility are different concepts; to understand fertility, one of the key concepts to know is that, in general conditions, the human species has a low reproductive efficiency with only between 20 and 25% of monthly pregnancy possibility in fertile couples and without any problem, reaching 80% of accumulated pregnancy rate throughout a year of searching and 90% after 2 years of searching for gestation.
Sterility is defined as the inability of a couple to conceive naturally within one year. Within this term, a distinction can be made between primary sterility, if the couple has never become pregnant, and secondary sterility, if the couple has already achieved a pregnancy previously, but at the present time is unable to become pregnant.
Infertility, on the other hand, is understood as the inability to achieve a live birth, this being the case of couples who achieve pregnancy but subsequently miscarry.
Therefore, although sterility and infertility are often referred to interchangeably, they are different concepts, although they have in common the inability to achieve an evolving pregnancy and a newborn.
Is infertility hereditary?
No, it is not. There are, however, medical conditions that are hereditary, and might interfere with a person's fertility. Polycystic ovary syndrome (PCOS), endometriosis, thyroid disorders, etc. are some examples.
What is tubal infertility?
Tubal sterility is defined as the inability of natural fertilization to occur due to obstruction of the fallopian tubes.
This obstruction can be spontaneous due to infection, pathology or malformation or it can also be intentional, that is, caused by the woman's will to cause sterility as a method of contraception. This is known as tubal ligation.
Are impotence and infertility linked?
To some extent, yes. As a matter of fact, as mentioned earlier, impotence is a post-testicular cause of male infertility. However, a man with the impotence problem can produce normal sperm and his sperm count be okay, and the same applies the other way round: it is not necessary for an infertile person to have erection problems.
Impotence can be cured with medications such as Viagra, but infertility might require the use of fertility treatments such as IVF or ICSI to produce offspring.
What is Y chromosome infertility?
It is a condition that affects sperm production (i.e. spermatogenesis), making it very difficult for these males to father children naturally. An affected man may produce:
- No sperm cells (azoospermia)
- A smaller-than-usual number of sperm cells (oligospermia)
- Abnormally shaped sperm cells (teratospermia)
- Sperm cells that do not move properly (asthenozoospermia)
Suggested for you
If you want to learn more about what causes male and female infertility, the most common symptoms, treatments, and more, our advice is that you visit any of the following links:
- Guide to male infertility: causes, symptoms, treatment and statistics
- Guide to female infertility: definition, causes, signs and treatment
To learn the details of all fertility treatment options available nowadays for you, do not miss this: Infertility treatments: definition and options available.
When infertility cannot be solved with infertility treatments, couples still have the option to fulfill their dream of having a family via donor conception and/or surrogacy. Do you want to find out what are your options? Check this out: Guide to third-party reproduction.
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Gnoth C., Godehardt E., FrnkHerrmannP., Friol K., Tigges J., Freundl G. Definition and prevalence of subfertility and infertility. Hum Reprod. 2005 ;20(5):1144-7.
Matorras R, Hernández J (eds) (2007): Estudio y tratamiento de la pareja estéril: Recomendaciones de la Sociedad Española de Fertilidad, con la colaboración de la Asociación Española para el Estudio de la Biología de la Reproducción, de la Asociación Española de Andrología y de la Sociedad Española de Contracepción. Adalia, Madrid.
World Health Organization (WHO) (2000). WHO Manual for the Standardized Investigation, Diagnosis and management of the infertile male. Cambridge: Cambridge University Press.
Guzick DS, Overstreet JW, Factor-Litvak P, Brazil CK, Nakajima ST, Coutifaris C, et al. (2001). Sperm morphology, motility, and concentration in fertile and infertile men. N Engl J Med 2001; 345: 1388-1393.
G.R. Dohle, T. Diemer, A. Giwercman, A. Jungwirth, Z. Kopa, C. Krausz (2010). Guía clínica sobre la infertilidad masculina. European Association of Urology 2010 (actualización en abril de 2010)
Carvajal R, Alba J, Cortínez A, Carvajal A, Miranda C, Romero C, Vantman D. Niveles de hormona antimüllerina y factor neurotrófico derivado del cerebro como predictores de función ovárica. Rev Hosp Clín Univ Chile 2012; 23: 159-67.
E.B. Hook. Rates of chromosome abnormalities at different maternal ages. Obstet Gynecol, 58 (1981)
Pellerito JS, McCarthy SM, Doyle MB, Glickman MG, DeCherney AH. Diagnosis of uterine anomalies: relative accuracy of MR imaging, endovaginal sonography, and hysterosalpingography. Radiology 1992; 183:795-800.
Prof. Mary Wingfield (2017). The Fertility Handbook: Everything You Need to Know to Maximise Your Chance of Pregnancy, Gill & Macmillan Ltd, May 29, 2017
Ramalho de Carvalho B, Gomes Sobrinho DB, Vieira AD, Resende MP, Barbosa AC, Silva AA, Nakagava HM. Ovarian reserve assessment for infertility investigation. International Scholarly Research Network. ISRN Obstetrics and Gynecology. Volume 2012, Article ID 576385, 10 pages. doi:10.5402/2012/576385.
Romero Guadix B, Martínez Navarro L, Arribas Mir L. Esterilidad: manejo desde la consulta del médico de familia. AMF. 2002; 8 (6): 304-311.
Royal College of Obstetricians and Gynaecologists. Fertility: assessment and treatment for people with fertility problems. NICE Clinical Guideline. February 2013.
FAQs from users: 'To what extent do lifestyle factors affect fertility?', 'Is sterility the same as infertility?', 'Is infertility hereditary?', 'What is tubal infertility?', 'Are impotence and infertility linked?' and 'What is Y chromosome infertility?'.
Authors and contributors








hello
II need your help.. I have been smoker for 10 years and doctors told me my fertility problems were attributed to heavy smoking.
So do I just have to quit smoking to restore fertility or is it already to late?
Hello Bud,
actually, changing unhealthy habits and adopting a healthy lifestyle can make a huge difference when trying to conceive. If you quit smoking, chances are that your sperm quality is restored after few months of being abstinent and a natural pregnancy would be possible.
Read more about how habits can affect fertility in men and women here: To What Extent Do Lifestyle Factors Affect Reproductive Health?
Hope this helps,
Best regards
This article talks about infertility vs. sterility but how would I know if I was infertile? Do I need to see my OB/GYN? Or go to a fertility clinic?
Hello Karen,
both men and women can undergo a series of tests in order to know their reproductive status.
Among the most common fertility tests for women available are hysterosalpingography, hormone tests, gynecological exams and chromosome testing. Should the results of any of these tests be altered, the doctor can ask you to undergo some additional screening tests, including an endometrial biopsy and a hysteroscopy. Read more about those tests in detail here: Female Fertility Tests – How Do You Know if You Can’t Get Pregnant?
Men, on the other hand, are required to undergo a hormone test and a physical exam as well and, besides, need to get their sperm tested by means of a semen analysis. Through this sperm test, he will learn about his sperm count and the quality of his sperm produced. Here, you find all information necessary when it comes to test a man’s fertility: Male Fertility Testing – How Do You Know if You Are Infertile?
Hope this answers your question,
Best regards