Female sterility is the inability to conceive due to problems related to the eggs that impede fertilization and, therefore, pregnancy. The alteration of the reproductive capacity can happen due to a variety of causes. The symptoms the woman experiences will be more or less noticeable depending on the cause.
For this reason, there may be situations in which the woman is not aware of her sterility until she undergoes the relevant fertility tests.
There are two main types of sterility:
- Primary sterility
- appears in women who have never been pregnant before.
- Secondary sterility
- When a couple is unable to achieve a pregnancy even though they already have one or more children in common. In other words, sterility appears after having been fertile previously.
Although they are two different types of infertility, the common point between them is the difficulty in achieving the desired pregnancy.
Provided below is an index with the 9 points we are going to expand on in this article.
- 1.
- 2.
- 2.1.
- 2.2.
- 2.3.
- 2.4.
- 2.5.
- 3.
- 4.
- 5.
- 6.
- 6.1.
- 6.2.
- 6.3.
- 6.4.
- 6.5.
- 6.6.
- 7.
- 8.
- 9.
Infertility and sterility in women
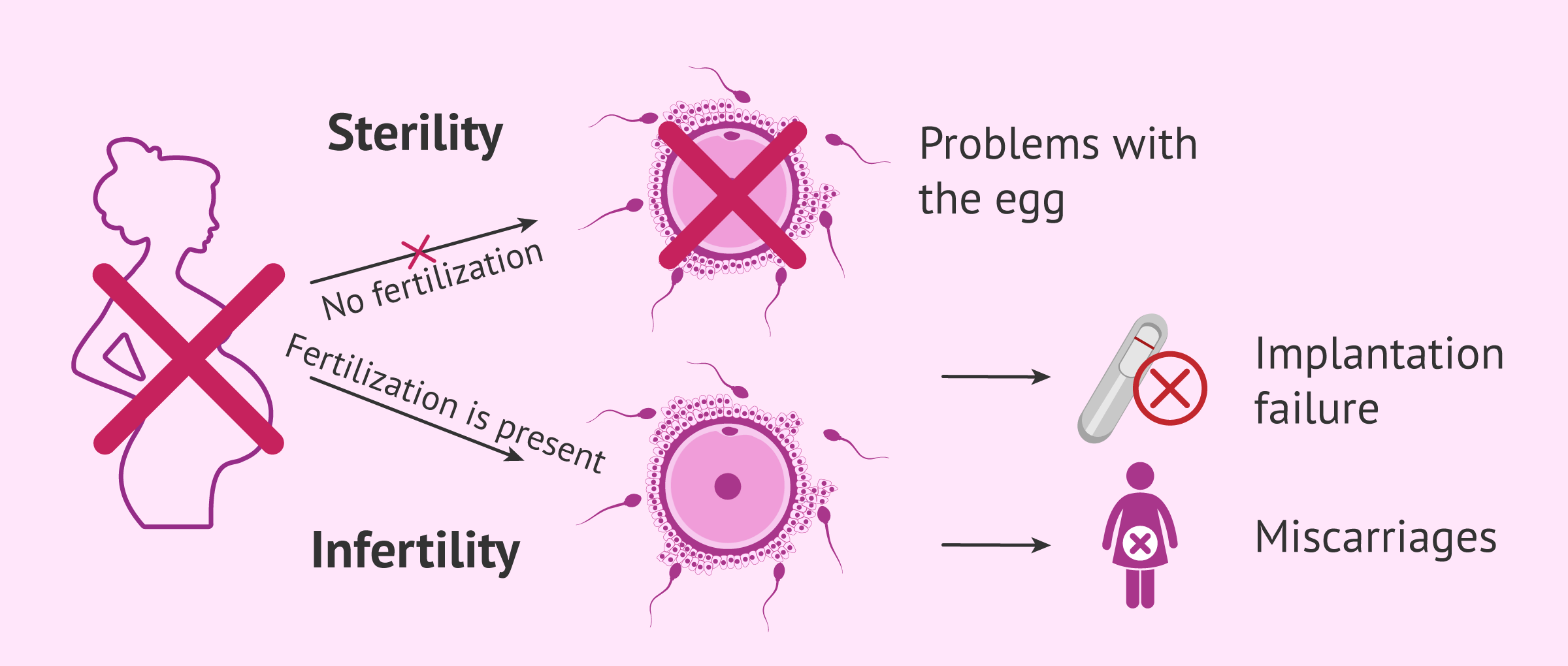
Although the terms sterility and infertility are commonly used as synonyms, both by society in general and professionals in this field, it should be noted that their meaning is not exactly the same:
- Female sterility
- The fusion between the egg and the sperm, i.e. fertilization, cannot take place due to problems related to the egg cell. Also, we talk about sterility when fertilization does occur, but still, the embryo is unable to attach to the endometrial lining. To sum up, it refers to every situation in which pregnancy cannot take place.
- Female infertility
- Although fertilization occurs and an embryo is obtained as a result of the egg-sperm binding, it cannot continue to develop fully, so a full-term pregnancy would never occur. It causes the woman to miscarry.
Be it as it may, both types hinder a woman's capacity to have a child, and therefore, are used interchangeably when talking about the causes, the signs, and the potential treatments to achieve a successful pregnancy.
Causes of infertility in women
Infertility problems in women can appear due to one or a combination of the following alterations:
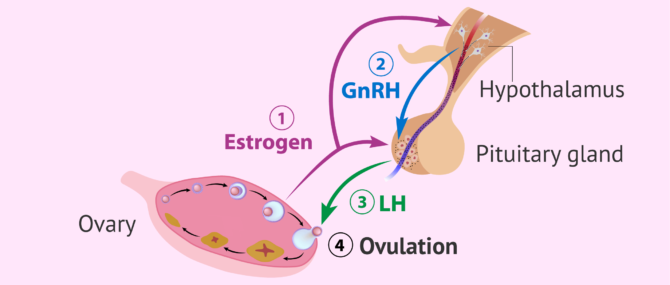
Problems with egg production
A leading cause of female infertility is associated with the ovulation cycle. It is known as endocrine factor infertility because the menstrual cycle is regulated by a set of hormones such as GnRH (gonadotropin-releasing hormone), FSH (follicle-stimulating hormone), LH (luteinizing hormone), progesterone, and estradiol.
Variations in hormone levels can lead to:
- Anovulation or absence of ovulation (egg release)
- Ovulation taking place earlier or later than expected
- Egg production failure
In normal menstrual cycles, without endocrine alterations, ovulation takes place halfway through the menstrual cycle (on day 14 approximately), considering as day 1 the day when the menstrual period begins.
For this reason, the most fertile days are the closest to ovulation, that is, the moment when the egg is released by the ovary so that the sperm hopefully reaches and fertilizes it inside the Fallopian tube.
Should a woman present any of the above-listed problems related to ovulation, pregnancy is unlikely to be achieved even if she tried to conceive during her most fertile days.
It should be noted that a sudden alteration in a woman's menstrual cycle does not automatically translate into female sterility. A woman is considered to be sterile when the problem persists over time.
For more information on this topic, please visit the following link: Female infertility due to endocrine-ovarian factor.
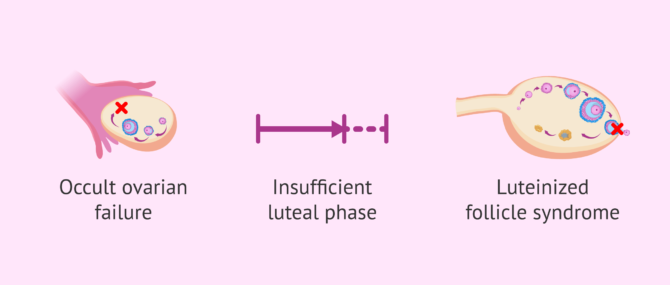
Ovulation abnormalities
The absence or the presence of alterations in the ovulation cycle leads to menstrual irregularities or even to amenorrhea (absence of menstrual periods). However, there are certain cases in which menstrual periods are apparently normal even though there are a series of problems related to hormones that hinder a woman's chances to become pregnant:
- Occult form of premature ovarian insufficiency (POF)
- a type of premature ovarian failure (POF) that prevents ovulation.
- Luteal phase defect (LPD)
- after ovulation, during the luteal phase of the menstrual cycle, the releasing of progesterone takes place, and its main function is to promote the growth of the endometrium to create an adequate environment for embryo implantation and pregnancy. Sometimes, the endometrial lining does not grow properly due to a poor production of progesterone, which makes pregnancy unachievable.
- Luteinized unruptured follicle (LUF) syndrome
- the follicle, which is home to the egg before ovulation, continues developing until the luteal phase begins even though no egg has been released within. Fertilization will not occur, as no oocyte has been released from the ovary.
Some causes of the hormonal imbalances that affect the endocrine system's regulation of ovarian cycles are stress, obesity, anorexia, thyroid problems, certain medications, chemotherapy, radiotherapy, environmental factors and so on.
Assisted procreation, as any other medical treatment, requires that you rely on the professionalism of the doctors and staff of the clinic you choose. Obviously, each clinic is different. Get now your Fertility Report, which will select several clinics for you out of the pool of clinics that meet our strict quality criteria. Moreover, it will offer you a comparison between the fees and conditions each clinic offers in order for you to make a well informed choice.
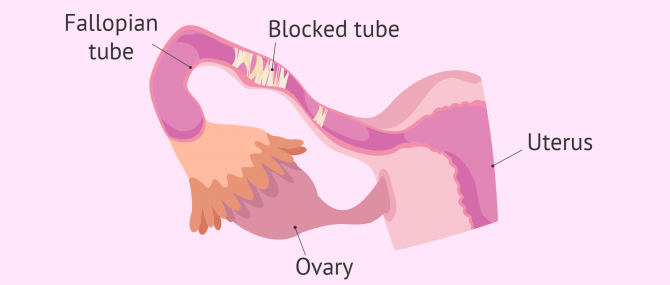
Fallopian tube problems
We use the term tubal factor infertility when referring to alterations or problems in the Fallopian tubes, the part of the female reproductive system where fertilization takes place.
During ovulation, an egg is released from the ovary and travels to the Fallopian tubes, so that a sperm reaches and fertilizes it. After fertilization, the resulting embryo travels through the tubes toward the uterus, where it will implant and give rise to a new pregnancy.
In order for these steps to take place, tubal patency in both Fallopian tubes, or at least in one of them, is necessary. They have to be functional as well. If both tubes are blocked, we consider that the woman suffers from tubal factor infertility.
Abnormalities related to tubal patency can be caused by infections, endometriosis, salpingitis, tubal malformations, hydrosalpinx, surgery and pelvic inflammatory disease (PID).
Hysterosalpingography (HSG) is a diagnostic test that allows us to evaluate the functionality of the uterine tubes.
If you want to learn more then please visit the following article: Tubal factor infertility.
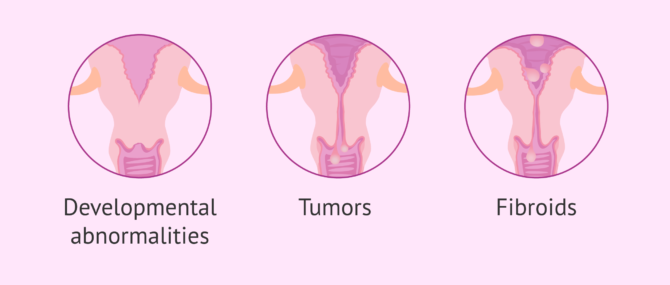
Cervical factor
The cervix the first place that sperm must pass through on their way to the egg. There may be obstructions in the form of tumors or fibroids that hinder fertilization.
On the other hand, the cervical mucus also helps the spermatozoa to move through the uterine interior, providing them with a medium through which to travel.
Some of the causes that cause infertility in women because they prevent the sperm from reaching the fallopian tubes to fertilize the egg are inflammations, infections or pH changes.
If you are interested in this topic, we invite you to read the following article: Female infertility due to cervical abnormalities.
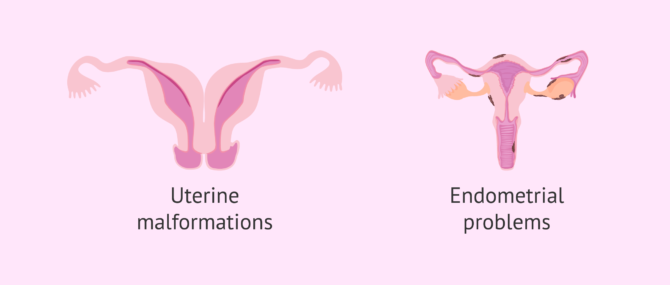
Infertility of uterine origin
There exist two main causes behind female infertility due to uterine abnormalities: on the one hand, uterine malformations, and on the other hand conditions related to the endometrium.
The endometrium or endometrial lining is the inner layer of the uterus where the implantation and attachment of the embryo take place.
Uterine abnormalities can be congenital, that is, from birth, or appear later in life as a consequence of fibroids, myomas, or cysts.
Also, it should be taken into account that endometriosis is infertility of uterine origin as well. It is a condition caused by the inflammation of the endometrial tissue, which grows outside the uterine cavity. Depending on the severity, it can be more or less perjudicial to a woman's fertility.
Click here if you want to get further information about this subject: Female infertility due to uterine abnormalities.
Other causes of infertility
There are other factors that affect sterility, but they can occur in both sexes, such as the following:
- Unexplained infertility
- in spite of having ran numerous fertility tests in the female and the male, no particular disorder causing infertility is detected.
- Immune infertility
- the most common cause of immune sterility is the presence of anti-sperm antibodies, either created by the female or the male, as well as the Antiphospholipid Syndrome (APS), which generates in the woman's body a hypercoagulable state that prevents the placenta working properly and leads to miscarriage.
- Psychological distress
- emotions, sensations, and feelings play a major role in a female's reproductive capacity. It is not uncommon for us to see cases of couples who were once infertile, but have achieved a natural pregnancy on the second attempt. A number of experts have linked this situation to the relaxation and elimination of the stress usually derived from infertility.
- Vaginal conditions
- vaginismus prevents penetration and ejaculation due to the contraction of the perivaginal muscles.
- Genetic causes
- Certain genetic and chromosomal alterations can make it difficult or impossible for a couple to conceive. Moreover, they can affect the normal development of a pregnancy, thereby leading to the loss of pregnancy.
Research advances in the field of human fertility lead day by day to the discovery of new causes of sterility, so that it is possible to outline new treatments and drugs to combat all these problems.
Symptoms of infertility in females
Female infertility can go unnoticed or, conversely, certain signs can make it quite obvious.
For example, in cases of female sterility due to endocrine factors, hormonal alterations usually lead to amenorrhea or menstrual irregularities, signs that some kind of problem exists, and are reasons for a woman to visit a fertility specialist.
Also, a blockage in the Fallopian tubes or the presence of myomas in the uterine cavity can cause the woman to feel pain or at least some sort of discomfort. There are, however, cases in which the patient has no noticeable symptoms, and is therefore totally unaware that there is a fertility issue that needs to be supervised by a duly qualified specialist.
Due to this wide range of signs, females, in general, are recommended to attend every routine gynecological consultation, and not to visit the specialist only in case of pain, discomfort or menstrual alterations.
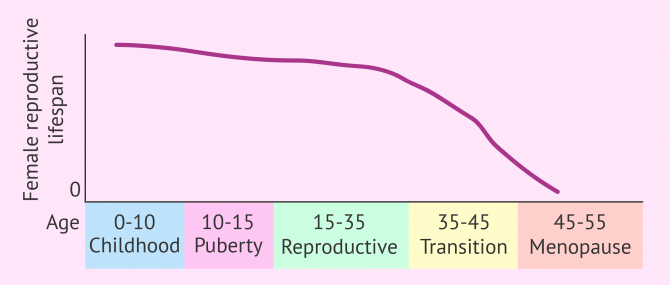
Fertility of women according to age
Contrary to what happens in men, women do not produce eggs de novo but are born with a finite number of eggs. From puberty and until menopause, ovulation of a large part of them will occur and the rest will degenerate on the maturation path to ovulation.
A woman's fertile period ranges from approximately 16 to 30-35 years of age. From this age, and especially from the age of 40, a woman's fertility progressively decreases until the complete depletion of the egg reserve at menopause.
In fact, Dr. Gorka Barrenetxea, a specialist in Gynecology and Obstetrics, tells us that:
The average age of the women who come to our center is 37-38 years old.
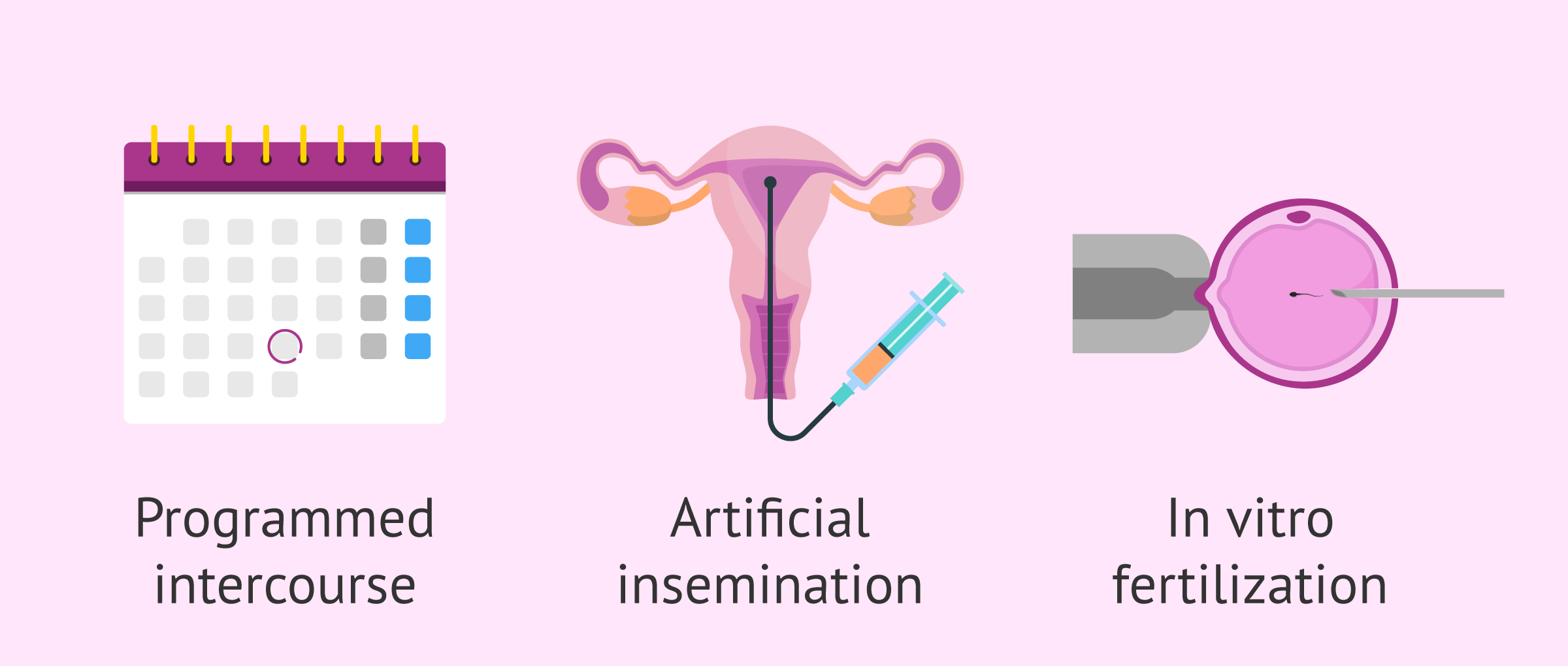
Treatments
In a situation of female infertility, the treatment necessary to achieve pregnancy will depend on its cause. Therefore, specialists recommend that each case be approached individually and that a personalized treatment protocol be developed.
In addition to the origin of the infertility, there are other factors that will influence the choice of the most appropriate treatment, such as the age of the woman and the male factor, mainly.
Once each case has been analyzed and all the necessary diagnostic tests have been performed, the fertility treatments that a woman or couple can use to have a child are as follows:
- Scheduled intercourse
- for cases of mild infertility, such as anovulation in young women. For this purpose, ovulation-inducing drugs are administered and intercourse is scheduled.
- Artificial insemination (AI)
- is the first assisted reproductive technique to be used when the woman is young and the partner's sperm is of good quality.
- In vitro fertilization (IVF)
- for more severe female or male infertility, or when AI has not worked after several attempts.
- IVF with preimplantation genetic diagnosis (PGD)
- in cases of infertility due to genetic causes or when there is a risk of transmission of a hereditary disease.
- Ovodonation
- when the woman does not have good quality eggs in her ovarian reserve, it will be necessary to resort to donor eggs.
Each of these treatments should be adapted to each woman according to her specific characteristics and causes of infertility. If you need more detailed information about this, you can continue reading in the following post: Techniques and treatments to combat female infertility.
FAQs from users
Could I have fertility problems because of my age?
Answered by Fertility Madrid
Yes, unfortunately the passage of time has a very negative influence. The fertile age is between puberty and menopause. Within this period, the best conditions are usually up to 35 years of age. As a woman's age increases, her ovarian reserve and the quality of her eggs decreases.

In short, the older a woman gets, the lower her fertility not only translates into a lower probability of pregnancy, but also into an increase in the number of miscarriages due to chromosomal abnormalities and complications during pregnancy.
When is a woman said to be infertile?
A woman is said to be infertile when she is unable to become pregnant within 1 year of having unprotected sexual intercourse regularly, after ruling out male causes.
There are a great variety of causes of greater or lesser severity. That is why in many cases it may happen that the woman is not aware of her problem until the necessary sterility tests are performed, since in many cases she does not show any symptoms.
There are 2 types of sterility:
- Primary
- is when we have never been able to get pregnant.
- Secondary
- is when we do not achieve gestation despite having one or more previous children with the same partner.

To know the state of our ovarian reserve, it is best to perform an ultrasound to assess the antral follicle count, and a hormone analysis to determine the levels of FSH and antimullerian hormone.
And finally, it is necessary to know that the period of greatest fertility in women is from 16 to 30-35 years of age approximately, with fertility being clearly affected from the age of 40 onwards.
Is pregnancy possible after oophorectomy?
Yes, it is possible. However, there are differing opinions when reviewing the literature regarding ovarian-hormonal function after oophorectomy.
Some studies indicate a lesser effect on female fertility when the procedure is performed at a younger age. Other studies point out that patients with only one ovary respond less to ovarian stimulation with lower oocyte collection and have a higher follicle stimulating hormone (FSH), an indicator of a low response to stimulation in in-vitro fertilization (IVF) protocols.
Up to what age can you become a mother?
It will depend on each woman and her ovarian reserve. A woman can be a mother naturally until she reaches the menopausal stage. However, as she approaches this stage, reproductive capacity decreases.
In any case and in general terms, we can say that from the age of 35 onwards, female fertility gradually decreases and it does so more markedly from the age of 40 onwards.
How do you know if a woman is infertile?
In order to know the fertility status of a woman, there are a series of medical tests that help to measure the woman's ovarian reserve and to study her reproductive capacity.

Among them are cytology, physical examination of the female reproductive system, the analysis of hormones such as FSH or AMH, etc.
How can pregnancy with infertility/sterility be achieved?
Depending on the cause of infertility, one solution or another will be provided to achieve pregnancy. Assisted reproduction offers a wide range of techniques and treatments so that women with infertility can become pregnant and fulfill their desire to become mothers.
The most common techniques are artificial insemination, in vitro fertilization (conventional or ICSI), PGD (preimplantation genetic diagnosis), egg and sperm donation, etc.
Recommended reading
Sterility or infertility in women arises from some alteration in the proper functioning of the entire reproductive system for all the reasons we have already discussed. First of all, if you want to know what a woman's fertility consists of and what her ideal development should be like, we recommend you to visit the following post: Fertility in women.
A woman's menstrual cycle is key to achieving pregnancy. To get all the information about what happens in each of its stages, you can read the following article: What is the menstrual cycle?
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Al-Badawi IA, Fluker MR, Bebbington MW. Diagnostic laparoscopy in infertile women with normal hysterosalpingograms. J Reprod Med 1999; 44:953-7.
Brodin T, Hadziosmanovic N, Berglund L, Olovsson M, Holte J. Antimüllerian Hormone Levels Are Strongly Associated With Live-Birth Rates After Assisted Reproduction. J Clin Endocrinol Metab. March 2013, 98(3):1107–1114 (View)
Carvajal R, Alba J, Cortínez A, Carvajal A, Miranda C, Romero C, Vantman D. Niveles de hormona antimüllerina y factor neurotrófico derivado del cerebro como predictores de función ovárica. Rev Hosp Clín Univ Chile 2012; 23: 159-67 (View)
Celik H, Bıldırcın D, Güven D, Cetinkaya MB, Alper T, Batuoğlu S. Random anti-Müllerian hormone predicts ovarian response in women with high baseline follicle-stimulating hormone levels Anti-Müllerian hormone in poor responders in assisted reproductive treatment. J Assist Reprod Genet, 2012; 29:797–802 (View)
Guzman L, Ortega-Hrepich C, Polyzos NP, Anckaert E, Verheyen G, Coucke W, Devroey P, Tournaye H, Smitz J, De Vos M. A prediction model to select PCOS patients suitable for IVM treatment based on anti-Müllerian hormone and antral follicle count. Human Reproduction, 2013, 28 (5): 1261–1266 (View)
Pellerito JS, McCarthy SM, Doyle MB, Glickman MG, DeCherney AH. Diagnosis of uterine anomalies: relative accuracy of MR imaging, endovaginal sonography, and hysterosalpingography. Radiology 1992; 183:795-800 (View)
Prof. Mary Wingfield (2017). The Fertility Handbook: Everything You Need to Know to Maximise Your Chance of Pregnancy, Gill & Macmillan Ltd, May 29, 2017
Romero Guadix B, Martínez Navarro L, Arribas Mir L. Esterilidad: manejo desde la consulta del médico de familia. AMF. 2002; 8 (6): 304-311 (View)
Royal College of Obstetricians and Gynaecologists. Fertility: assessment and treatment for people with fertility problems. NICE Clinical Guideline. February 2013.
FAQs from users: 'Can abortion cause infertility in the future?', 'Could I have fertility problems because of my age?', 'Can I get pregnant without Fallopian tubes?', 'When is a woman said to be infertile?', 'Is pregnancy possible after oophorectomy?', 'Can Mirena cause infertility after removal?', 'Up to what age can you become a mother?', 'How do you know if a woman is infertile?', 'Does infertility cause divorce?', 'How can pregnancy with infertility/sterility be achieved?', 'Can an infertile woman get pregnant with homeopathy?' and 'Can an infertile woman have periods?'.
Authors and contributors


More information about Michelle Lorraine Embleton






Hello,
Me n my husband are 35 yrs old and we are planning for a baby. I did check ovulation tests from 8th day to 15th day of my periods. But tests are coming negative. Does it mean I am not ovulating?
Dear Prachi,
If it happened just this month, it might be due to a temporary hormonal imbalance, so in principle it’s not a concerning issue. On the other hand, there’s also the possibility that you have ovulated, but the level of the hormone responsible for ovulation was not enough as to be detected through an ovulation test. My advice is that you monitor your menstrual cycles, especially your ovulations, and if this continues to happen and you detect anovulation or any other kind of irregularity, visit your gynecologist.
I hope this helps,
Best
Hello,
Thank u for replying,
I did this test this month only. I will surely monitor it next month too. But are these tests 100% accurate?
Hello again Prachi,
You are welcome. Ovulation tests are 99% accurate in detecting the LH surge that precedes ovulation – they work similarly to home pregnancy tests.
Best of luck!
Thank u so much for replying
You’re welcome!
Should you have any further questions, do not hesitate to ask.
Best wishes
Hello,
Im married since 11 months.
My hormones are great. I am thin, im also very healthy, i exercise daily. But im really stressed because im not pregnant yet.
They diagnosed me with PCO since my cycles are not regular.
What shall we do?
Hello Sami,
My recommendation is that you visit the following website: polycysticovarysyndrome.info There you will find information about polycystic ovaries (PCO) and PCOS, including information about how to achieve pregnancy in spite of it.
I hope that helps,
Regards
HI, ladies!
My name is Sofia and I am a 31-year-old woman living in Australia. have been working on pregnancy from last few years. 3 years ago I met with my soulmate and married him. I truly believe that it was one of the great days of my life.
Now I am trying to conceive and trying to make my family with him. I want to make him one of the happiest person on the earth. It’s really hard to notice that someone is working really hard for me but I am not able to give him a child.
Infertinity really sucks! It really annoying and fustrating. I want to get out of it and want to get a baby. I hope this helps.
Hello there, I’m Katie. I’m 26 years old. I enjoy very good health and use to practice yoga daily. Yoga is the cause of my mental stability till now. Otherwise, I’m very depressed and frustrated. I got married three years ago. I had a pregnancy which lasted about 3 months and then I had a miscarriage due to some suspicious reasons. We were trying to conceive for more than a year but no success. When doctor declared me infertile, I remained
shocked. I considered it as the end of the world but life keep on going. We also adopted a child but he left us two months ago. Sometimes I feel very guilty and ashamed of me in front of others. I known it won’t be helpful in any regard but all I want is to have a baby, who can strengthen our relationship. But I have no idea what I should do now. I’m here for your expert advice. This means a lot to me. Thanks!
Hi @katiespencer, I’m sorry you’re going through this..May god help you, poor thing.
Here’s a couple of things to share. I’m 37 yrs oldie. we ttc 2 yrs. Soon diagnosed with blocked fallopian tubes. Did the surgery which opened my right tube. Tried clomid iui #1 with no luck. Followed medicated cycles with monitoring, no baby. Did another lap surgery. Again tried 2 IVF shots home. #1 ER 10 eggs, 6 fertilized – bfn. #2 FET – beta confirmed but then strated dropping dramatically. Both times transferred 3-day embies. Actually I do think my little beans weren’t strong enough to implant. We decided to switch the clinic where we passed donor egg IVF cycle. Our clinic performs 5day transfers only. Moreover, they guarantee at least 3 A grade blasts for the ET. so I’m sure this improved our situation. Hoping for you.
Good morning, I wanted to know what it means to have a prolactin of 90.35 ng/ml out of a range of 4.79 – 29.9. Thanks
Hi GraceE
First of all, we need to know the phase of the menstrual cycle in which the analysis was done. The prolactin hormone has higher values in the luteal phase than in the proliferative phase.
Such a high prolactin level is indicative of hyperprolactinemia. This occurs during pregnancy, lactation or if there is any alteration due to the intake of antidepressants, anxiolytics, etc.
Other pathologies that lead to hyperprolactinemia are: hypothyroidism, hyperandrogenism, anorexia nervosa, chronic renal insufficiency, polycystic ovarian syndrome, etc.
You can obtain more information in the following link: What is hyperprolactinemia? – Causes symptoms and treatments.
I hope I have helped you.
Best regards