IVF is the medical abbreviation for in vitro fertilization, a challenging Assisted Reproductive Technology (ART) from the technical viewpoint that is used to help couples or women who have trouble conceiving.
The success rates of IVF depend on multiple factors, but undoubtedly age is a key factor. Also, the quality of the sperm used plays a major role when it comes to determining the chances of getting pregnant with IVF.
The total cost of in vitro fertilization procedures is considerably high due to two main aspects: on the one hand, the hormonal medications used to induce ovulation, and on the other hand, the varied range of modern technologies and lab equipment used.
Provided below is an index with the 13 points we are going to expand on in this article.
- 1.
- 2.
- 3.
- 3.1.
- 3.2.
- 4.
- 4.1.
- 4.2.
- 5.
- 6.
- 7.
- 7.1.
- 7.2.
- 8.
- 9.
- 9.1.
- 9.2.
- 9.3.
- 10.
- 10.1.
- 10.2.
- 10.3.
- 10.4.
- 10.5.
- 10.6.
- 10.7.
- 10.8.
- 10.9.
- 11.
- 12.
- 13.
Definition of IVF
In vitro fertilization is an Assisted Reproductive Technology (ART) that involves the collection of eggs from the woman's ovaries by means of follicle puncture (ovum pick-up). Then, they are fertilized at the laboratory using the husband's or partner's sperms. The development of the resulting embryos is monitored until the embryo or embryos selected are transferred back to the woman's uterus. The ultimate goal is to achieve a healthy pregnancy.
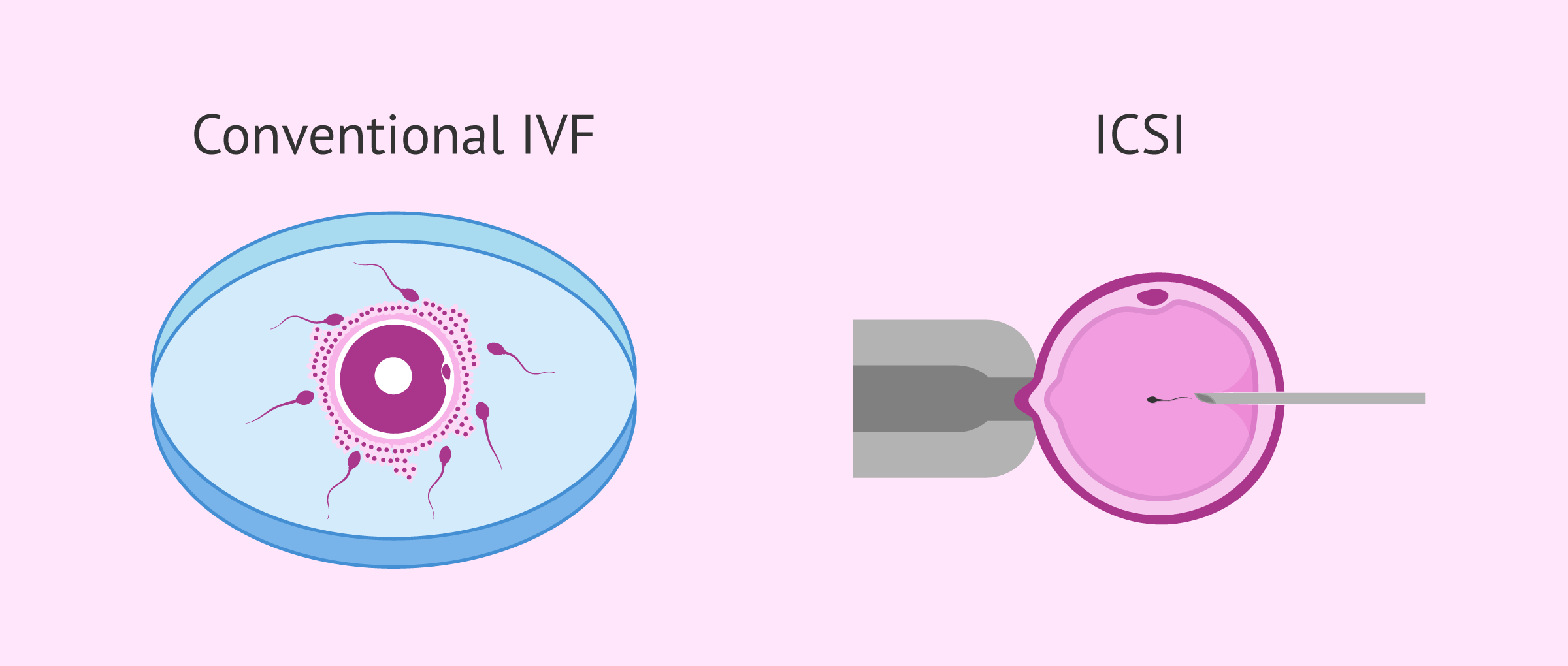
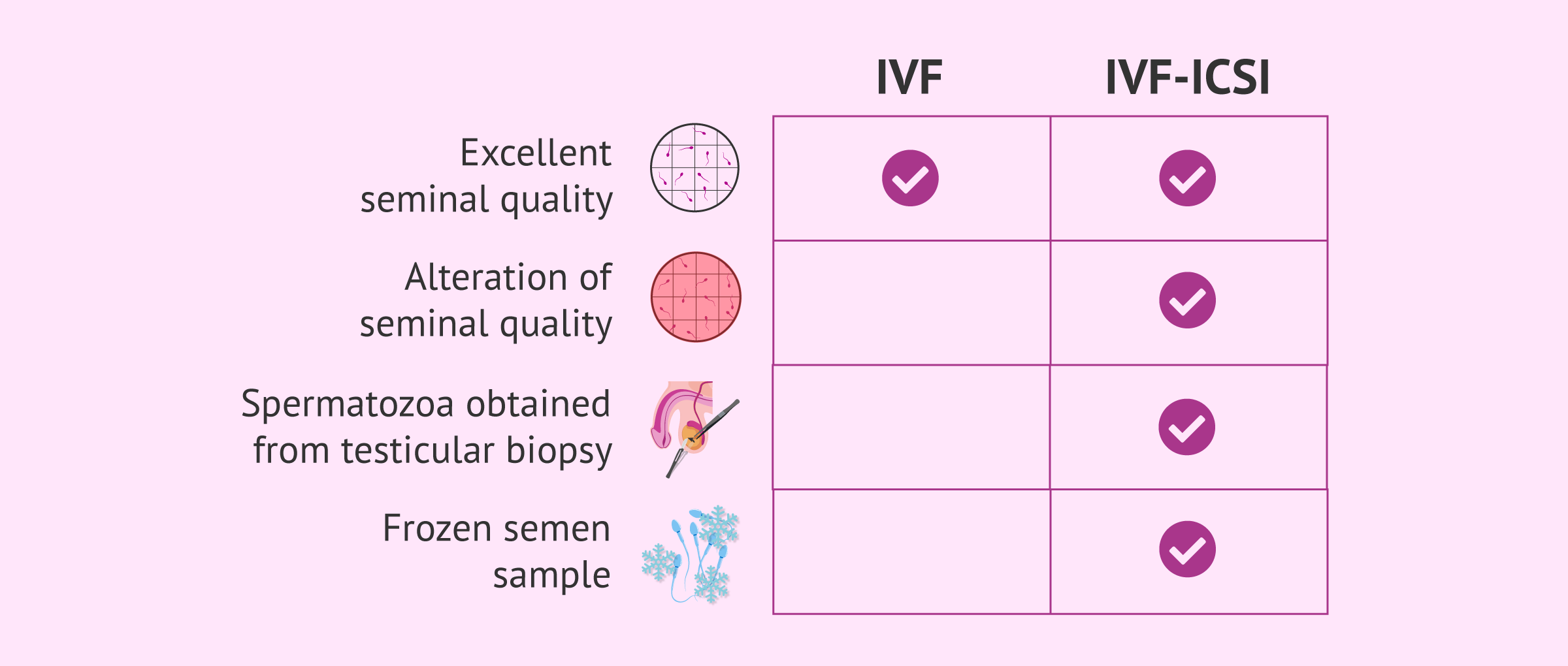
Depending on how the egg and the sperm cell are fused together, we can distinguish between two types of IVF:
- Conventional IVF: Both reproductive cells are put in contact in a petri dish and are expected to fuse together by themselves.
- ICSI: It stands for Intracytoplasmic Sperm Injection. The sperm is manually inserted inside the egg cell by microinjection.
Choosing between the former or the latter depends on what is causing female and/or male infertility in the couple, as well as the particularities of each fertility clinic. Still, even though the fertilization process varies, the previous steps are the same.
If you want to know more details about the differences between one and the other way of gamete fusion, you can read this article: IVF or ICSI: What is the difference? Which is better?
Difference between IVF and IUI
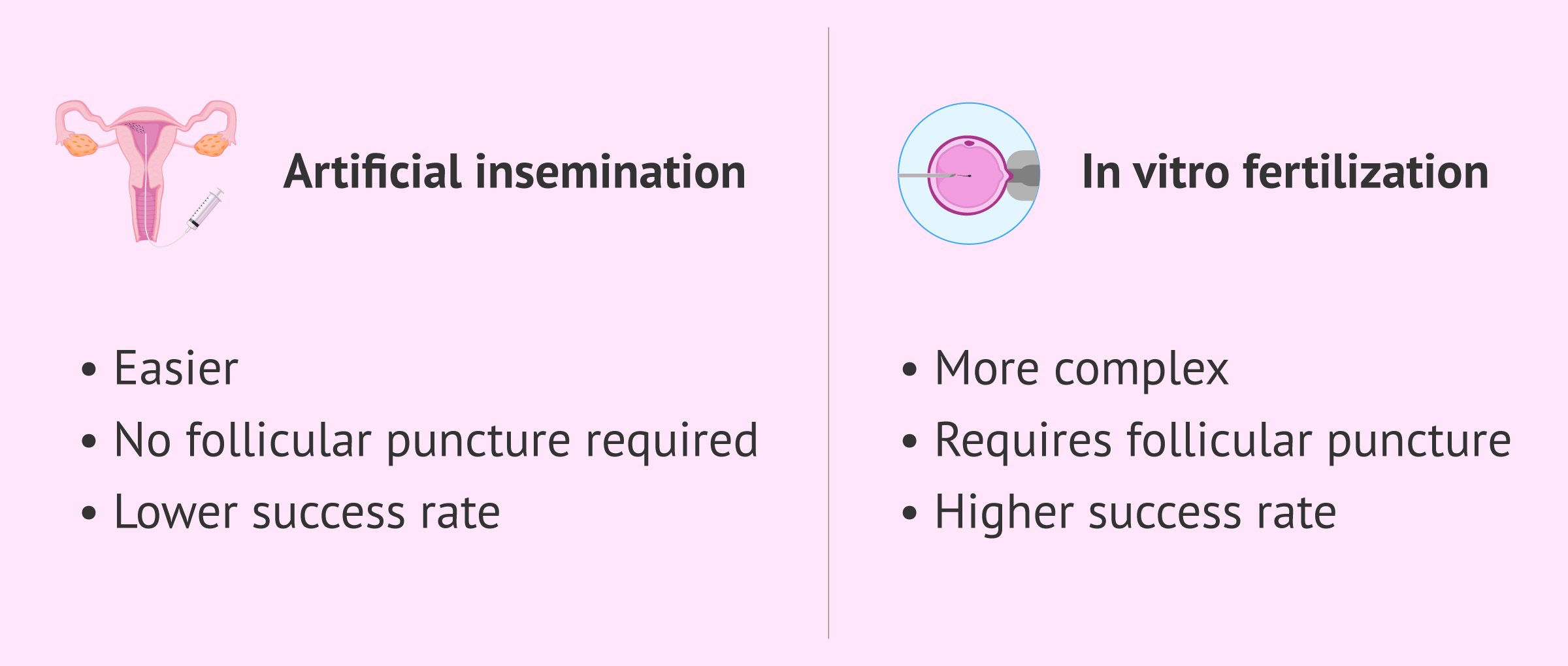
Artificial insemination (AI), better known as intrauterine insemination or just IUI, is another infertility treatment, though less technically challenging than IVF. With IUI, the partner's sperm is inserted into the female's uterus, and fertilization occurs inside the female reproductive tract as it would with sexual intercourse, without further medical involvement.
So, as one shall see, IVF involves a higher degree of complexity than artificial insemination (AI)—not only the number of steps to follow is higher, but also the involvement of the specialist. In fact, IVF requires a simple surgical procedure to retrieve the eggs, while with IUI this step is unnecessary.
Its success rates, however, are higher, and this is the reason why it is the treatment of choice in the majority of the cases.
You may hear terms such as in vitro insemination, which actually is incorrect as you may have understood with the definition of each technique given above.
The following post contains further info on this topic: Artificial insemination vs. in vitro fertilization.
When is IVF used?
A couple may need IVF treatment to have a baby due to a wide range of causes. Male infertility, female infertility or both may be the reason why this infertility treatment is recommended.
The following are the most common indications of in vitro fertilization:
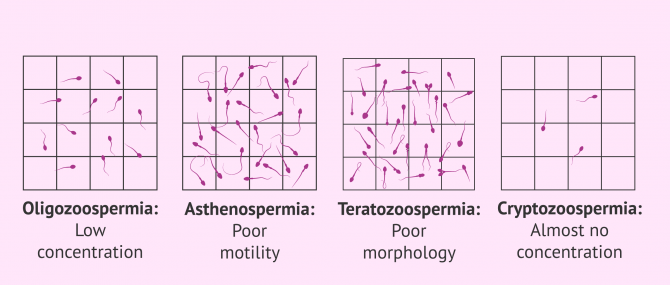
Male infertility
Moderate-to-severe cases of male infertility can be treated by means of IVF:
- Oligozoospermia
- few sperm in the ejaculate.
- Asthenozoospermia
- slow or immotile spermatozoa.
- Teratozoospermia
- Abnormally shaped sperm in the head, neck and/or tail.
- Cryptozoospermia
- the concentration of sperm is almost zero.
- Oligoastenoteratospermia
- a combination of several alterations.
If you are interested in further reading about this topic, we recommend you read the following article: What Causes Male Infertility? - Symptoms & Treatment.
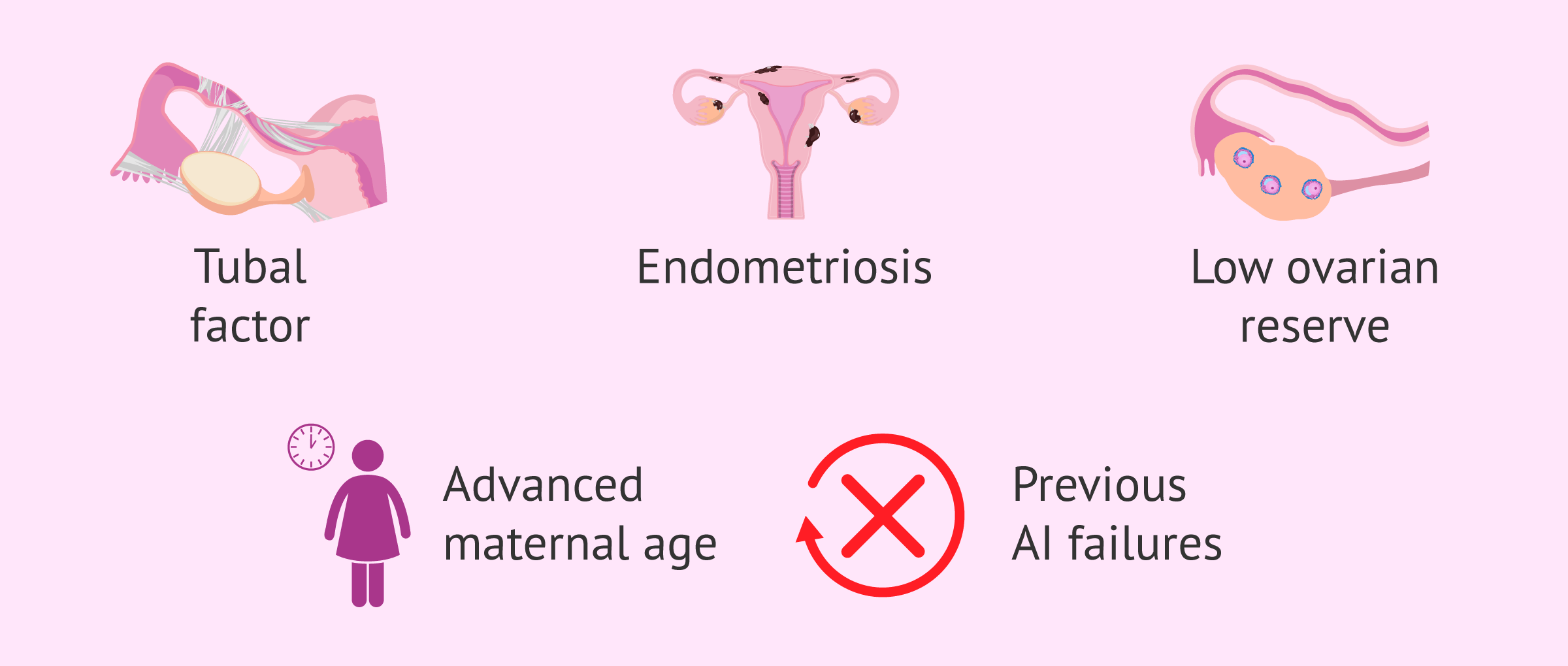
Female infertility
In the case of women, fertility problems are often linked to the following factors:
- Endocrine ovarian factor infertility
- Problems with ovulating caused by endocrine disorders, such as anovulation.
- Tubal factor infertility
- alterations in the fallopian tubes that cause an obstruction.
- Uterine factor infertility
- Uterine malformations, tumors such as polyps or fibroids, endometriosis, etc.
- Cervical factor infertility
- changes in the cervix that prevent the passage of sperm into the uterine cavity.
- Controlled ovarian stimulation: Patients take fertility drugs to induce ovulation for around 10 days. The purpose is to obtain a higher number of eggs. This way, the moment of ovulation can be monitored, which helps increase the odds for the eggs collected to be mature, with a good fertilization potential.
- Ovum pick-up or follicle puncture: It is a surgical intervention for the collection of mature oocytes. It is done through aspiration, which takes 20-30 minutes and requires anesthesia.
- Semen collection and capacitation: Samples are collected through masturbation, although it can be done through epididymal sperm aspiration or testicular biopsy. Samples go through a sperm washing process to increase their fertilization potential.
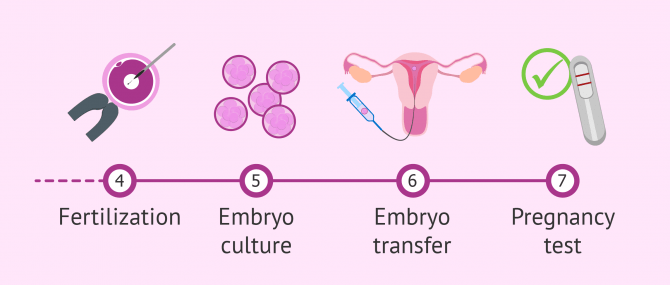
- Fertilization: The egg and sperm binding takes place at this point, either for themselves (conventional IVF) or through microinjection (ICSI). For more information about the differences between both ways of fusing gametes, we recommend that you read the following post: IVF vs ICSI.
- Embryo culture: Once the oocyte has been fertilized, the embryo development is monitored to check whether everything is going as expected. Embryo implantation in the mother's uterus will take place within seven days post insemination. Until then, the embryos are cultured in incubators that simulate optimal development conditions at the IVF laboratory.
- Preparing uterus for embryo transfer: Women are given estrogen and progesterone for the pattern and the thickness of the endometrial lining (the uterine layer where embryos implant) to be adequate and the odds for embryo implantation to rise.
- Embryo transfer: After being cultured, the best quality embryos are selected. The most viable embryos will be the ones chosen for the transfer. Usually, between 1 or 2 embryos are transferred, although 3 or more can be used depending on what is established by law in the country where the transfer is taking place.
- Embryo freezing: High-quality unused embryos are cryopreserved by vitrification for later use.
- Pregnancy test: Within 10 to 15 days (two-week wait) post embryo transfer, women can take a pregnancy test to detect their hCG levels in case embryo implantation has been successful.
- 40% in women under 35
- Between 27-36% in women between 35 and 37
- Between 20-26% in women between 38 and 40
- Between 10-13% in women over 40
- Consistently high success rates.
- Couples with severe infertility problems have the chance to become parents. In particular, ICSI offers the possibility of attaining fertilization even in cases of severe male infertility, such as obstructive azoospermia.
- Using both donor eggs and donor sperm is possible, something that increases the number of infertile patients who can become parents thanks to IVF.
- In general, the potential side effects associated are not severe.
- Patients have to self-administer fertility drugs, which can lead to the appearance of complications.
- Surgery under anesthesia is necessary. Even though it is a simple procedure that does not take too long, some risks exist.
- The cost of IVF is higher if compared to other techniques such as IUI.
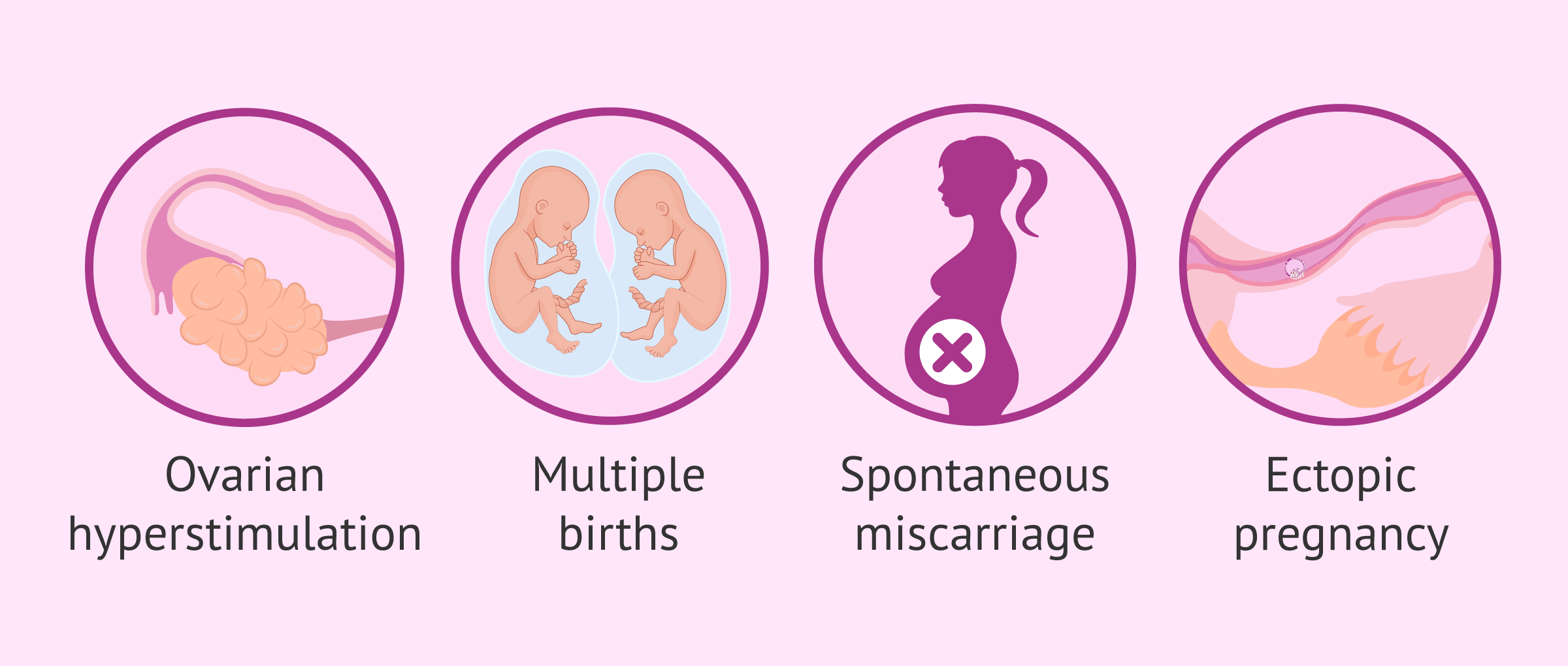
- Ovarian Hyperstimulation Syndrome (OHSS): It translates into a super stimulation of the ovaries. It causes ovarian enlargement and extravasation of liquids due to an increase in blood vessel permeability. The function of the liver, hematologic, renal, and respiratory systems may be compromised in the most severe cases.
- Multiple births: The risk for a twin pregnancy with a single embryo transfer (SET) is almost non-existent. However, in those cycles where two embryos are transferred, the probability of having twins is 6%. If three embryos are transferred, the chances rise up to 12%, while triplet pregnancies occur in 3% of the cases. Still, these rates depend also on factors such as maternal age and the quality of the uterine lining.
- Miscarriage: Almost 20% of pregnancies end up in a miscarriage, and it tends to happen during the early stages of pregnancy. It depends on factors such as the patient's age and the particularities of each woman or couple.
- Ectopic pregnancy: It occurs when the embryo implants in a place other than the uterine cavity. Between 2% and 5% of women who undergo an IVF treatment may have an ectopic pregnancy as a result. This figure contrasts with the approximate 1% of this type of pregnancy when it occurs as a result of a natural conception.
- They have never had IVF treatment before
- There is no evidence of low ovarian reserve
- They have talked with their doctor about the risks of IVF and pregnancy at this age
- Registration fee: from $300
- Administration fee: from $650
- Drug costs: from $3,000
- Embryo cryopreservation: from $1,000
- Ongoing storage of embryos: from $250
- Thawing and replacing frozen embryos (FET): from $1,300
- Additional procedures such as Preimplantation Genetic Diagnosis (PGD), assisted hatching, ICSI, oocyte cryopreservation, etc. would contribute to increase the sum above.
In addition, IVF would also be indicated in case of previous failures in artificial insemination (IUI).
Requirements for IVF
Although the in vitro fertilization technique is a widespread technique that can help many patients, the truth is that it has some requirements.
Requirements in the woman
In order to perform in vitro fertilization, it is necessary that the woman is able to produce mature eggs. In addition, it is necessary that the patient does not have uterine problems or anomalies that prevent the implantation of the embryo or the evolution of the gestation.
On the other hand, if the woman has a diminished ovarian reserve and it is not possible to obtain mature eggs, IVF with donor eggs can be performed. If you want to know what this treatment consists of, you can read the following post: What is ovodonation, and what is the price of the treatment?
Requirements in the male
In the case of the male, the requirements vary depending on the type of IVF to be performed. If the seminal quality allows it, conventional IVF can be performed. If, on the other hand, the sperm has serious motility, morphology, or concentration problems, the ICSI technique will be chosen.
In any case, even if the requirements for conventional IVF are met, there are fertility clinics that prefer to perform ICSI.
On the other hand, when semen samples do not come from ejaculate, as in the case of a testicular biopsy, ICSI is also required, since their quality is usually very low. The same can occur when frozen semen is used, since performing an ICSI allows optimizing the amount of cryopreserved sample.
It is also possible to perform IVF with donor sperm in cases of azoospermia or absence of a male partner, and even IVF with double donation, that is, with donated eggs and sperm.
What does in vitro fertilization consist of?
The IVF process can become a tough one for many patients, as they have to go through various steps before achieving success.
The following article explains each of these IVF steps in more detail: What is the IVF process step-by-step like?
IVF Results and Probability of Success
Just like other assisted reproductive technologies, IVF success rates are based on several factors, being the patient's age one of the most influential ones.
Experts have been able to establish a series of patterns to grade the odds for success in each case. Such percentages are:
When talking about and comparing the success rates of different techniques or fertility clinics, one should pay attention to the meaning of success in each case. Sometimes, statistical data refers to different percentages, e.g. pregnancy rate, birth rate, live birth rate, etc.
Real IVF outcomes should be based on the live birth rates obtained with this method, and not only on the pregnancy success rate. It should be taken into account that not all pregnancies are successful.
If you want to learn more about IVF success rates and outcomes, the following article may be of interest: Success Rates of IVF.
Advantages and disadvantages
Like any other infertility treatment (e.g. intrauterine insemination or IUI), in vitro fertilization procedures have a series of advantages and disadvantages. You can find them explained below.
What are the benefits of IVF?
The following are the main advantages of in vitro fertilization:
If you are interested in learning more about this topic, you can continue reading here: What are some of the main advantages of in vitro fertilization?
What are the disadvantages of IVF?
However, IVF carries a series of disadvantages as well:
Regardless of whether you go for a classical IVF cycle or an ICSI, the drawbacks associated are similar.
Potential side effects and risks
As seen earlier, ovarian stimulation and follicle puncture can cause a series of adverse reactions. Patients should be informed about all these potential risks before getting started with the treatment.
If you want more information about the risks of IVF, we recommend that you read this article: Side effects of IVF.
How much does IVF cost?
Before giving you particular sums, it is important to remark that there are many variables specific to your particular medical case that can influence the overall cost of IVF.
In countries like Spain or the UK, where IVF and other treatments can be covered by the public health system as long as the patient meets a series of requirements, IVF is available for everyone.
Cost in the USA
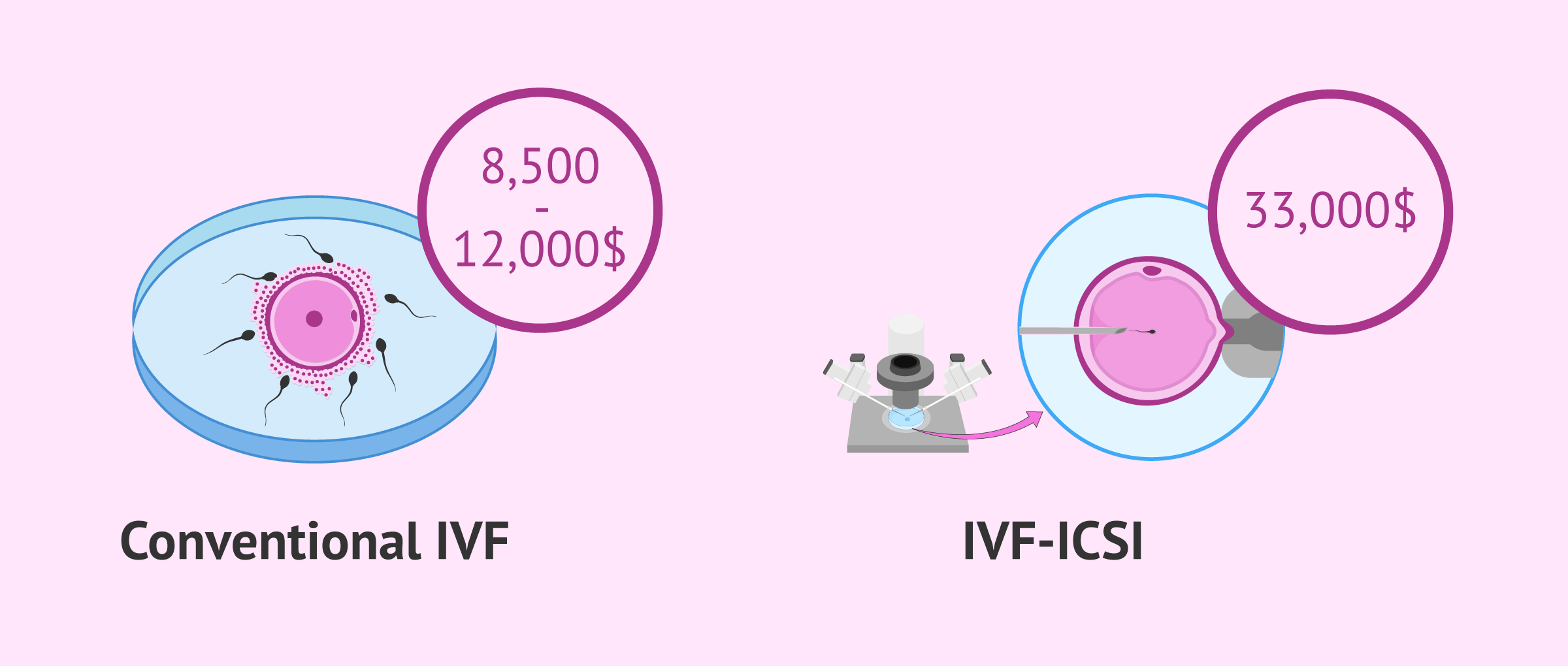
Many US clinics offer different in vitro fertilization cost plans, including multiple cycle packages with different pricing options. For example, single cycle IVF packages using own eggs can range from $8,500 to $12,000.
On the other hand, some fertility clinics offer money-back guarantee programs, available for a higher fee. For example, while a multiple cycle IVF cost plan without money-back guarantee can cost about $16,000, the price with money-back guarantee (usually up to 80%) is typically $18,000 or more.
The availability of these plans is subject to the health insurance plan of each patient. In some IVF centers, multiple cycle IVF cost plans are available only in case the patient is not covered by insurance. However, the standard type of IVF arrangement across the country is a single cycle.
The use of additional techniques contributes to increasing the cost. For example, if ICSI and assisted hatching were necessary, the cost can be as high as $33,000 or over, and using ICSI with PGD for a blastocyst embryo transfer using donor eggs and a surrogate can start from $80,000.
Check out this post to learn more about the costs of surrogacy with egg donation and other fertility treatments involving third parties: Guide to Third Party Reproduction.
If you need to undergo IVF to become a mother, we recommend that you generate your Fertility Report now. In 3 simple steps, it will show you a list of clinics that fit your preferences and meet our strict quality criteria. Moreover, you will receive a report via email with useful tips to visit a fertility clinic for the first time.
Cost in the UK
The costs of IVF vary on a case-by-case basis, and some women may be eligible to have NHS-funded IVF, provided that they meet the criteria that can be found on the fertility guidelines published by the National Institute for Health and Care Excellence (NICE).
If you decide to have IVF treatment at a private clinic, are not eligible for NHS treatment, or want to skip long waiting lists, the cost of a single IVF cycle can be £5,000 or more.
In the case of women aged under 40 years who have not been able to conceive after 2 years of regular unprotected intercourse or 12 artificial insemination cycles (with 6 or more being by IUI), the NHS will offer them 3 full cycles with or without ICSI.
As for women aged 40-42 years who have not been able to conceive after 2 years of regular unprotected intercourse or 12 cycles of artificial insemination (with 6 or more being by IUI), the NHS will offer them 1 full cycle, with or without ICSI, as long as they meet these requirements:
Also, in cases of unexplained infertility, that is, where evidence shows that there is no chance of pregnancy and IVF is clearly the only effective treatment, your doctor will refer you directly to NHS-funded IVF treatment.
Another possibility for British patients in need of IVF is pursuing this treatment abroad. Often, women who opt for this alternative are in need of egg donation. However, you should keep in mind that the HFEA only licensed clinics in the UK.
Cost in Canada
The general cost of in vitro fertilization (IVF) in Canada usually starts from $7,000 (Canadian dollars). However, the total cost is expected to be higher, especially if you are not covered by insurance. To the basic cost of IVF treatment, you should add:
It should be noted that the province of Ontario pays for fertility treatments, provided that you are an Ontario resident and have a valid OHIP card. To qualify for Ontario’s Fertility Program (one-time cycle per lifetime of IVF), the woman must be under the age of 43. You can qualify for an additional cycle if you act as a surrogate.
FAQs from users
What happens if I don't get pregnant the first time after IVF?
Sometimes pregnancy is not achieved with the first transfer. If there are vitrified embryos, a second transfer can be performed.
If there are no vitrified embryos from the first follicular aspiration, a second IVF cycle can be performed with the advantage of being able to take into account all the information provided by the first cycle. This information is usually very valuable for deciding on actions such as changes in the ovarian stimulation pattern, measures to improve embryo transfer, such as performing a hysteroscopy, and even the possibility of performing a laparoscopy, which can help diagnose hidden pathology such as endometriosis.

It is very important the attitude that is taken before a negative first cycle of assisted reproduction. Being aware that success often does not come the first time can lessen the sadness in the face of a negative result. Specialized psychological support has shown advantages in subsequent cycles.
What negative effects can IVF medication have?
Medications used in assisted reproduction can produce various side effects such as headaches, mood swings, abdominal pain, hot flashes and bloating. Occasionally, they can cause ovarian hyperstimulation syndrome.

With ovarian stimulation, more eggs are developed than in a natural cycle, but this will not lead to an earlier menopause. Women are born with a finite number of eggs and maturation has no effect and will not bring an earlier end to the reproductive stage.
Does IVF pregnancy require special care?
Pregnancies achieved with fertility treatments have no greater risk of complications than any other.
The precautions are no different from those of any pregnant woman, including the continuation of sexual activity. Once the embryo has implanted, the risks of a pregnancy achieved through IVF are no different than any other. In addition, the recommendations and special care will be more related to the woman's age, in cases of advanced age, and/or history of previous pathologies.
Is IVF an option for gay couples as well?
On the one hand, lesbian couples have the chance to have a child through lesbian IVF or intra-partner egg sharing. It is a way for both of them to participate in the process actively, as one becomes the biological mother and the other the birth mother.
Intrauterine insemination (IUI) with donor sperm is another option available for lesbian couples. However, it depends on the chances for conception this treatment may bring to the couple, so fertility tests will be performed prior to choosing between one option or another.
On the other hand, gay men can build their family thanks to surrogacy with donor eggs. In this case, a gestational carrier undergoes IVF with the eggs of another woman, who acts as the egg donor for the intended parents, while one of them delivers the semen sample. Thus, the child will be genetically linked to one of the parents.
Can I get pregnant naturally after IVF?
Many couples achieve a natural pregnancy after having had an "test tube" baby. It happens in cases where the cause of infertility declines or disappears.
Stress is a good example. Some patients see their fertilizing potential reduced because of the stress caused when trying to conceive. Anxiety can affect egg and sperm quality, thereby hindering the odds of conception.
Making lifestyle changes (relaxing, changing dietary habits, diminishing or stopping the consumption of toxic substances, etc.) can help improve the chances of getting pregnant to a large extent.
Also, it may occur in cases of unexplained infertility.
What are the symptoms of an IVF pregnancy?
When IVF is successful, there is no reason why pregnancy symptoms should be different to those of a natural pregnancy. Still, drugs to induce ovulation may cause some side effects such as bloating or nuisance, but in principle they are not expected to be different.
Is time off necessary after IVF egg collection?
No, it is not normally needed, either after follicle puncture or after the embryo transfer. Bed rest for IVF recovery is recommended only in exceptional cases.
What is the probability of success of a second IVF?
Depending on the cause of the failure of the first IVF attempt, a second attempt may or may not improve the probability of success.
For example, if the failure of the first IVF was due to poor endometrial preparation, the second attempt will change the medication protocol to try to improve this aspect.
Normally, in the second attempt some guidelines are changed to improve the treatment and this usually results in a greater probability of success, although as we have mentioned, it will depend on each situation.
IVF or ICSI, which one is better?
No treatment is better than the other, as both of them have their pros and cons. Depending on the characteristics of each couple and the origin of their fertility problems, IVF or ICSI would be more advisable.
For example, the most severe cases of asthenozoospermia should be treated with ICSI to guarantee a minimum number of chances for success. On the other hand, when the woman suffers from problems with ovulating or blocked fallopian tubes, conventional IVF can help solve the problem successfully.
Conventional IVF is more similar to natural conception and requires a higher degree of gamete manipulation. However, ICSI helps patients make a step forward toward pregnancy, as the egg-sperm binding is done manually.
Suggested readings
Following IVF embryo transfer, the next phase of the treatment is known as two-week wait or 2WW, which is defined as the time period between the transfer and the moment when you finally test for pregnancy. If you want to learn more and get some useful tips to survive it, check out this post: What is the Two-Week Wait (2WW)? – Tips to Survive It.
Also, if you are interested in learning more about ICSI, a more challenging type of IVF, we recommend that you visit this post: What Is ICSI or Intracytoplasmic Sperm Injection?
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Alper M, Brinsden PR, Fischer R, Wikland M (2002). Is your IVF program good? Hum Reprod; 17: 8-10 (View)
Andersen AN, Gianaroli L, Felberbaum R, de Mouzon J, Nygren KG (2005). Assisted reproductive technology in Europe, 2001. Results generated from European registers by ESHRE. Hum Reprod; 20: 1158 – 1176 (View)
Andersen AN, Goossens V, Ferraretti AP, Bhattacharya S, Felberbaum R, de Mouzon J, Nygren KG, The European IVF-monitoring (EIM) Consortium, for the European Society of Human Reproduction Embryology (ESHRE) (2008). Assisted reproductive technology in Europe, 2004: results generated from European registers by ESHRE. Hum Reprod; 23: 756 – 771 (View)
ASRM, American Society for Reproductive Medicine (2002). Revised minimum standards for in vitro fertilization, gamete intrafallopian transfer, and related procedures. A Practice Committee Report. Guidelines and Minimum Standards (View)
Aytoz A., Camus M., Tournaye H., Bonduelle M., Van Steirteghem A. and Devroey P. (1998): Outcome of pregnancies after intracytoplasmic sperm injection and the effect of sperm origin and quality on this outcome. Fertil. Steril. 70: 500-505 (View)
Broekmans FJ, Kwee J, Hendriks DJ, Mol BW, Lambalk CB (2006). A systematic review of tests predicting ovarian reserve and IVF outcome. Hum Reprod Update; 12:685-718 (View)
ESHRE Capri Workshop Group. Intracytoplasmic sperm injection (ICSI) in 2006 (2007): evidence and evolution. Hum Reprod Update;13:515 – 526 (View)
Fernández A, Castilla JA, Martínez L, Núñez AI, García-Peña ML, Mendoza JL, Blanco M, Maldonado V, Fontes J, Mendoza N (2002). Indicadores de calidad asistencial en un programa de FIV/ICSI. Rev Iberoam Fertil; 19: 249-52 (View)
FAQs from users: 'What happens if I don't get pregnant the first time after IVF?', 'What negative effects can IVF medication have?', 'Does IVF pregnancy require special care?', 'Is IVF an option for gay couples as well?', 'Can I get pregnant naturally after IVF?', 'What are the symptoms of an IVF pregnancy?', 'Is time off necessary after IVF egg collection?', 'What is the probability of success of a second IVF?' and 'IVF or ICSI, which one is better?'.
Authors and contributors
More information about Cristina Algarra Goosman













Hello, my name is Amanda. I’ve endometriosis (grade IV) and did surgery on July. I’ve been trying to conceive ever since with no luck so far. I’d like to know how long should I remain in the waiting list for IVF. Do you know if it will take longer or less?
Hello Amanda,
I am afraid fertility clinics do not give any preference to women suffering from endometriosis or any other pathology. You should take into account that every woman who undergoes IVF has been diagnosed with a fertility problem, and there’s no problem more important than the others. As for waiting lists, it depends on each fertility clinic, and may vary from a few days to several months.
I hope I have been able to help,
Regards
Hello! Thank you for this wonderful article.
Well, I did an ET which finally was negative and after a few months resting, I started a second cycle this time with a frozen embryo I froze after my 1st attempt. This time I’m taking estrogens orally, and also patches and pessaries, but even with all that my endometrium is not growing. Later, provided that the estrogens took me to depression, they tried with my natural cycle, but my endometrium does not grow!
Is there any medication in the world I can take to make my endometrium grow? Natural estrogens or something like that? What about acupuncture or exercise? Anything?
Thanks!
Hello Caitlyn,
In those cases where there is no endometrial growth, knowing what is causing it is very difficult. Anyhow, it was a good idea to try with a natural cycle, since there are times when administering estrogens and progesterone exogenously leads to failure because the organism does not response to medications and therefore endometrial thickness remains the same.
Although you can try with different natural remedies, it should be clear that they are not fertility treatments and won’t make your endometrium grow as expected; but any help is good anyway. Exercise may promote blood circulation in that zone, leading thus to endometrial growth.
And the same applies to acupuncture and some foods that improve blood flow such as oranges and ginger. As for taking natural estrogens, I recommend you to ask your gynecologist firstly.
Best wishes
Good morning! After spending about two years trying to conceive, my husband already has one from his previous marriage. We were told that my ovarian reserve was not bad but not very good either. Besides, my husband has lazy sperm and they aren’t motile. I am 33 and he is 44.
I would like to have someone to guide us through the whole process and which options do we have to become parents.
Hi Lily,
I am very sorry for what the doctors have told you, but don’t be discouraged, you still can try a fertility treatment in a fertility clinic.
Finding a clinic near you that suits your needs is a bit complicated. Patients usually have many doubts and questions when choosing a clinic to undergo treatment, so we have made the article How to choose the best fertility clinic for me?. I hope it will help you and clarify your doubts.
You may also find our Fertility Report very useful. Through it, you will be able to access the assisted reproduction clinics that are closest to you and that meet our quality criteria. You will be able to obtain useful information and guidance on the processes and treatments.
I hope you find it useful,
Wish you all the best.
Hi,
I’d like to know if you can get pregnant after an ovary and tubal removal surgery. Thanks.
Hi Sue,
As long as you keep your uterus, you can get pregnant, because it is the essential organ to carry a pregnancy. However, once your tubes and ovaries have been removed, you will need to have an IVF with donor eggs unless you have vitrified your own eggs before the surgery.
Hope this answers your question,
Best
Good morning!
after trying for two years, we were told that my ovarian reserve was not bad but not very good either. Besides my husband has lazy sperm and they are inmotile.
I’m 34 years old, he is 46.
I would like to have someone to guide me through the process.
Hello Biscuit
I am very sorry for what the doctors have told you, but don’t be discouraged, you can try an assisted reproduction treatment in a clinic.
Finding a clinic near you that suits your needs is a bit complicated. Patients usually have many doubts and questions when choosing a clinic to undergo a treatment, so we have made the article How to choose the best fertility clinic for me. I hope it will help you and clarify your doubts.
You may also find our Fertility Report very useful. This allows you to access the fertility clinics that are closest to you and that meet our quality criteria. You will be able to obtain useful information and guidance on the processes and treatments.
I hope it will be of use to you,
wish you all the best.
Will a blood test be performed after a frozen embryo transfer to see if I got pregnant and for how long I’ve been pregnant?
Hi Cactus,
After a frozen embryo transfer, you should wait at least 10 days to take a pregnancy test to determine if the embryo has implanted and you are pregnant. This time is known as the two-week wait. You can read more about it here: What is the Two-Week Wait (2WW)? – Tips to Survive It.
I recommend you to be calm during these days and try not to think. This is a period of many emotional ups and downs and it is not easy. You should try to keep a positive and relaxed attitude
Good luck!